[box type=”bio”] What to Learn from this Article?[/box]
Stroke may be the cause of divergent shoulder dislocation fracture; consultation between neurologist, anesthesiologist and orthopedist is necessary for patient efficient management.
Case Report | Volume 7 | Issue 3 | JOCR May – June 2017 | Page 13-16| Atchi Walla, Faré Gnandi-Piou, Pilakimwé Egbohou, Komi Assogba, Mawuko Quacoe. DOI: 10.13107/jocr.2250-0685.784
Authors: Atchi Walla[1], Faré Gnandi-Piou [2], Pilakimwé Egbohou [3], Komi Assogba [4], Mawuko Quacoe [5]
[1] Department of Orthopaedics, Sylvanus Olympio Teaching Hospital, Lomé, Togo.
[2] Department of Orthopaedics, Kara Teaching Hospital, Kara, Togo.
[3] Department of Anesthesia, Sylvanus Olympio Teaching Hospital, Lomé, Togo.
[4] Department of Neurology, Campus Teaching Hospital, Lomé, Togo.
[5] Polyclinelle Wossinu and Gbogbo hospital, Lomé, Togo.
Address of Correspondence:
Dr. Atchi Walla,
03 BP 30090 Lomé 03, Togo.
E-mail: atchi.walla@yahoo.fr
Abstract
Introduction: The literature review revealed that nowadays only about 15 cases of bilateral shoulder dislocation associated with the fracture of the upper end of the humerus have been published. The triad of lesional mechanism designated by the triple syndrome E composed of epilepsy, electrocution, and external trauma was the circumstances noted in which these fractures dislocations occur with migration of the two humeral heads either forward or backward.
Case Report: An architect of 36-year-old, right-handed, was admitted in emergency department for loss of knowledge of progressive installation. At admission the blood pressure, pulse, and temperature were normal. There was a right hemiparesis predominantly in brachiofacial side and an aphasia. After intensive resuscitation measures, the cerebral computed tomography scan revealed a left temporoparietal hypodensity area affecting the middle cerebral artery superficial territory with a mass effect compatible with acute ischemic stroke. During the hospitalization, episodes of generalized tonic-clonic convulsions appeared with a fever at 39°C and a leukocytosis at 35 thousand on the 5th day. These convulsions caused on the right shoulder an anterior dislocation under coracoid, associated with a fracture of the greater tubercle and on the left shoulder, posterior dislocation with much displaced comminuted articular proximal humeral fracture. We did reduction by external maneuvers for the right shoulder and open reduction with internal fixation by anatomical plate of left shoulder lesions. In the immediate aftermath of surgery, he presented episodes of agitation which led to the dismantling of the left shoulder fixation. He was evacuated to the North Country where an ablation of the left shoulder material and stabilization by locked plate were carried out. The sequelae were marked by the occurrence of an osteomyelitis with osteolysis of the entire upper right humerus extremity. It will require an inverted prosthesis.
Conclusion: The surgical treatment must be done by a solid assembly and consultation with neurologists and anesthetists is essential. This multidisciplinary management could prevent any convulsive postoperative seizures that would risk sacrificing all therapeutic efforts.
Keywords: Bilateral divergent fracture-dislocation, shoulders, ischemic stroke, Togo.
Introduction
Bilateral posterior or anterior dislocations of the shoulder joint are rare [1, 2]. A review of literature revealed more than 15 cases of bilateral fracture-dislocations of shoulder [3]. In these lesions, humérus proximal fracture is associated with simultaneous shoulder dislocation either in the anterior or posterior plane [4]. In the two forms of humeral head migration, they can be traumatic injuries, electrocution, and generalized seizures in epilepsy. Simultaneous dislocation in different direction exceptional and have been sometimes seen in emotionally disturbed patients [3]. According to reports from today, divergence form of these bilateral shoulder fracture dislocation is a new aspect. Moreover, the occurrence of this lesion following an ischemic stroke appears to be another new element in its ethiopathogenesis. This case is reported to discuss the unusual mechanism behind this divergent bilateral fracture dislocation of shoulder and its management difficulties.
Case Report
An architect of 36-year-old, right-handed, was admitted in emergency department for loss of knowledge of progressive installation in a context of headache without vomiting. At admission the blood pressure, pulse, and temperature were normal. There was a right hemiparesis predominantly in brachiofacial side and an aphasia. The cerebral computed tomography (CT) scan revealed a left temporoparietal hypodensity area affecting the middle cerebral artery superficial territory with a mass effect compatible with acute ischemic stroke (Fig. 1).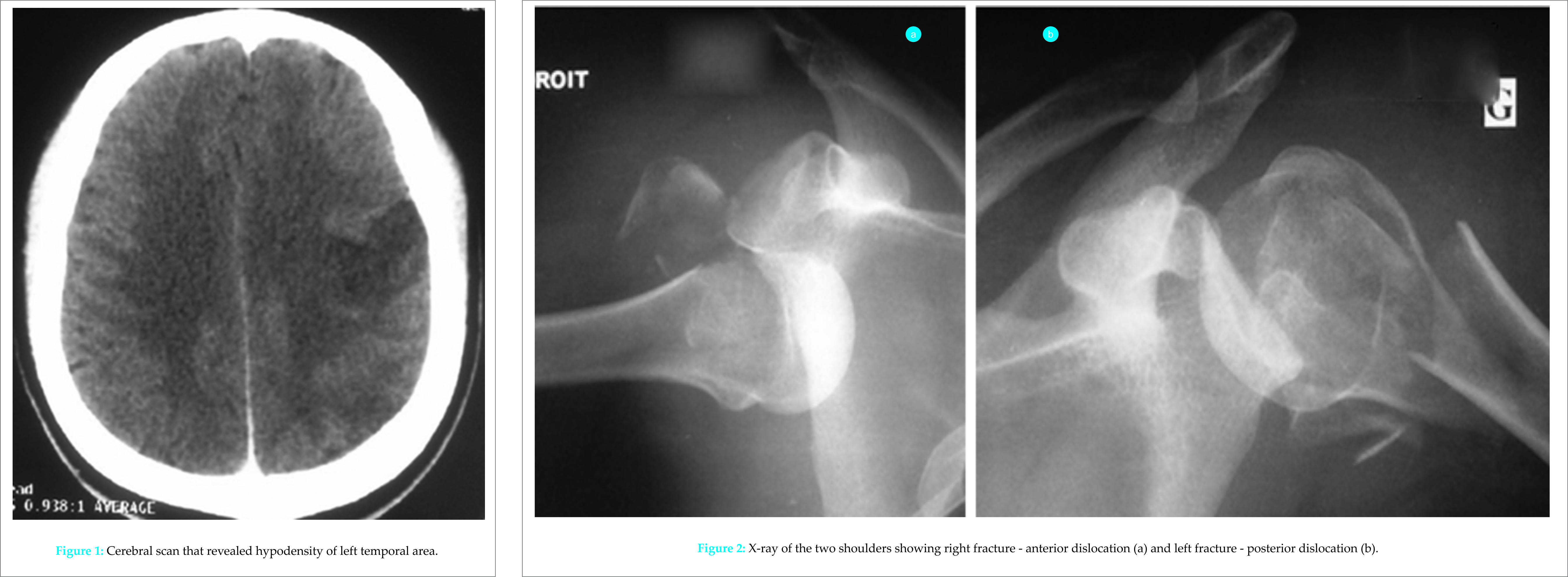
Intensive resuscitation measures were instituted and the patient was put ender diazepam intravenously, carbamazepine, enoxaparin, and then, antibiotics. During the hospitalization, episodes of generalized tonic-clonic convulsions appeared with a fever at 39°C and a leukocytosis with 35 white miles on the 5th day. These convulsions caused on the right shoulder an anterior dislocation under coracoid, associated with a fracture of the major tubercle (Fig. 2a) and on the left shoulder, posterior dislocation with much displaced comminuted articular proximal humeral fracture without axillary nerve lesion (Fig. 2b). The CT scan has detailed bone lesions (Fig. 3). There was no notion of falling during or after these convulsions. The following day, the traumatic lesions were reduced by external maneuvers for the right shoulder (Fig. 4) and open reduction and internal fixation by anatomical plate of left shoulder lesions through a transdeltoid longitudinal approach. The two shoulders were immobilized complementarily by removable splints arm to the body. In the immediate aftermath of surgery, he presented episodes of agitation which led to the dismantling of the left shoulder internal fixation (Fig. 5). The improvement of its neurological state and of the biological markers toward the 15th day allowed a reprise of the left shoulder with contribution of graft and a fixation of the major tubercle on the right.
The CT scan has detailed bone lesions (Fig. 3). There was no notion of falling during or after these convulsions. The following day, the traumatic lesions were reduced by external maneuvers for the right shoulder (Fig. 4) and open reduction and internal fixation by anatomical plate of left shoulder lesions through a transdeltoid longitudinal approach. The two shoulders were immobilized complementarily by removable splints arm to the body. In the immediate aftermath of surgery, he presented episodes of agitation which led to the dismantling of the left shoulder internal fixation (Fig. 5). The improvement of its neurological state and of the biological markers toward the 15th day allowed a reprise of the left shoulder with contribution of graft and a fixation of the major tubercle on the right.
At the request of his entourage, he was evacuated to the North Country where an ablation of the left shoulder material and stabilization by locked plate were carried out (Fig. 6). The sequelae were marked by the occurrence of an osteomyelitis with osteolysis of the entire upper right humerus extremity (Fig. 7). It will require an inverted prosthesis.
Discussion
The rare cases of dislocation of bilateral shoulder fractures occur during epileptic seizures or in the course of trauma that occurs during convulsions [4]. The trauma may be due to a direct impact of the shoulders on objects near the patient or falls. Blackstone evoked the triad or triple E composed of epilepsy, electrocution, and external trauma to explain the circumstances in which these lesions occur [5]. The new fact is the divergence in the migration of the two fractured humeral heads (right anterior and left posterior) in our stroke patient. This divergent character of the dislocated of both shoulders suggests that the lesions did not occur simultaneously but rather sequentially. Because about to Pushpakumara et al. [3] humerus neck fracture can also accompany simultaneous shoulder dislocation either in the anterior or posterior plane. On the right (side with the paralysis), it could be considered that during a convulsion, weak contractions of the lateral rotators made the anterior dislocation possible, especially if the limb was in abduction and lateral rotation, the subscapularis latch being weakened by the paresis [4]. In these conditions, an attempt by the parents of the entourage to keep the patient in supine position in bed [3] by pressing on the anterior face of the distal arm thus achieves the antepulsion and the migration of the humeral head forward. The percussion of the head on the antero-inferior pole of the glenoid cavity in other convulsions would have caused the fracture of the right greater tubercle. On the left side, the persistence of the seizures would explain to the left shoulder probably in adduction, internal rotation and flexion, the propulsion of the humeral head back and top of the glenoid cavity as Shaw and all have described [6]. The fracture comminution of the upper humerus extremity would be due to the repeated impaction of the latter during the various convulsive seizures. This hypothesis is supported by the importance of the swelling and extent of bruising observed on the left shoulder. Thus, to the triple syndrome E described by Bradestone in 2001 to summarize the circumstances of these bilateral shoulder fracture dislocations [5], we could add, considering the stroke involved in our patient, and the letter S of the word stroke. The triple E would then become SEEE. The other aspect that caught our attention in this young patient was the difficulty of choosing the mode of reconstruction and fixation of the left comminuted fracture so that it resists any convulsive seizures in operative continuations. In this context, the locked plate seems to be an interesting solution even if it is not the guarantee of the expected anatomical and functional results [7]. The persistence of convulsions after surgery was, unfortunately, the cause of the secondary displacement observed in our case at the left shoulder. The reconstruction of the humeral head with the addition of bone and the most solid fixation possible so that the assembly can mechanically withstand the possible convulsive seizures in the postoperative period are therefore elements to be taken into account. Moreover, consultation with neurologists and anesthetists is essential to limit the occurrence of convulsive seizures in the post-operative period by appropriate treatments to preserve the reconstruction of the humeral head.
Conclusion
The bilateral dislocated shoulder dislocation fracture is exceptional. Our case shows that stroke may be the cause. The surgical treatment must be done by a solid assembly and consultation with neurologists and anesthetists is essential. This multidisciplinary management could prevent any convulsive postoperative seizures that would risk sacrificing all therapeutic efforts.
Clinical Message
At the triple syndrome E (external trauma, electrocution, and epilepsy), described as the circumstances which can provide bilateral shoulder fracture dislocation, is added stroke. Dislocations in these cases can be divergent. The choice of the mode of reconstruction and fixation of the humeral head in the young patient remains a challenge with regard to the comminution. In all cases, the surgical treatment must be done by a solid assembly and consultation with neurologists and anesthetists is essential. This multidisciplinary management could prevent any convulsive postoperative seizures that would risk sacrificing all therapeutic efforts.
References
1. Sanel S, Sencan S, Öçgüder A, Solakoglu C. Bilateral, locked, recurrent anterior shoulder dislocation: Case report. Eklem Hastalik Cerrahisi 2015;26(1):52-55.1. Sanel S, Sencan S, Öçgüder A, Solakoglu C. Bilateral, locked, recurrent anterior shoulder dislocation: Case report. Eklem Hastalik Cerrahisi 2015;26(1):52-55.
2. Ivkovic A, Boric I, Cicak N. One-stage operation for locked bilateral posterior dislocation of the shoulder. J Bone Joint Surg Br 2007;89(6):825-828.
3. Pushpakumara J, Sivathiran S, Roshan L, Gunatilake S. Bilateral posterior fracture-dislocation of the shoulders following epileptic seizures: A case report and review of the literature. BMC Res Notes 2015;8:704.
4. Sharma L, Pankaj A, Kumar V, Malhotra R, Bhan S. Bilateral anterior dislocation of the shoulders with proximal humeral fractures: A case report. J Orthop Surg (Hong Kong) 2005;13(3):303-306.
5. Brackstone M, Patterson SD, Kertesz A. Triple “E” syndrome: Bilateral locked posterior fracture dislocation of the shoulders. Neurology 2001;56(10):1403-1404.
6. Shaw JL. Bilateral posterior fracture-dislocation of the shoulder and other trauma caused by convulsive seizures. J Bone Joint Surg Am 1971;53(7):1437-1440.
7. Clavert P, Adam P, Bevort A, Bonnomet F, Kempf JF. Pitfalls and complications with locking plate for proximal humerus fracture. J Shoulder Elbow Surg 2010;19(4):489-494.
 |
 |
 |
 |
 |
| Dr. Atchi Walla | Dr. Faré Gnandi-Piou | Dr. Pilakimwé Egbohou | Dr. Komi Assogba | Dr. Mawuko Quacoe |
| How to Cite This Article: Walla A, Gnandi-Pio F, Egbohou P, Assogba K, Quacoé M. Bilateral Divergent Shoulder’s Fracture Dislocation Case in an Ischemic Stroke Patient. Journal of Orthopaedic Case Reports 2017 May-June;7(3):13-16. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




