[box type=”bio”] Learning Points for this Article: [/box]
Proper imaging and surgical approach selection is important in managing pelvic impalement injuries.
Case Report | Volume 7 | Issue 5 | JOCR September – October 2017 | Page 24-28| Nirmal Raj Gopinathan, Rakesh John, Himanshu Kanwat, Pebam Sudesh. DOI: 10.13107/jocr.2250-0685.882
Authors: Nirmal Raj Gopinathan [1], Rakesh John [1], Himanshu Kanwat [1], Pebam Sudesh [1]
[1] Department of Orthopedics, Post Graduate Institute of Medical Education and Research, Sector 12, Chandigarh, Punjab, India.
Address of Correspondence
Dr. Rakesh John,
Department of Orthopedics, Post Graduate Institute of Medical Education and Research, Sector 12, Chandigarh, Punjab, India.
E-mail: rakeshjohn23@gmail.com
Abstract
Introduction: Impalement injuries of pelvis have been reported in children but are uncommon. Impalement could be associated with injuries to deep organs, wound contamination, crush injuries, and in certain instances, can even be fatal.
Case Report: We present a bizarre case of a 2-year-old female child who presented to us with a tapestry needle embedded in the true pelvic cavity after a history of fall on the buttock while playing at home. The impaled needle was eventually successfully extracted surgically using the modified Stoppa’s approach and the post-operative period was uneventful. We also briefly review the literature surrounding such unusual injuries and discuss tips and tricks regarding the surgical technique in such cases.
Conclusions: In impalement injuries, adequate analgesia, tetanus prophylaxis, antibiotics, and immobilization must be given initially followed by meticulous pre-operative planning in the form of radiographs and computed tomography (CT) scans. Minimally invasive CT-guided extraction of needle can be attempted by an experienced interventional radiologist when there is no significant risk of damaging neighboring vital organs or neurovascular structures. The surgical approach if an open approach is decided must be chosen wisely; backup may be needed from an abdominal surgeon, urologist, or gynecologist in certain cases.
Keywords: Foreign body, Pelvis, Impalement injury, Modified Stoppa’s approach.
Introduction
Impalement injuries are defined as those injuries in which a sharp or a blunt object traverses through a part of the body with the object remaining in situ [1, 2, 3]. It can be associated with injuries to deep organs, wound contamination, crush injuries, and in certain instances, can be fatal [1, 2, 3]. In this case report, we present a case of a child who sustained an impalement injury to the left buttock with a tapestry needle; in an attempt to retrieve the needle from the posterior aspect, it was inadvertently pushed further anteriorly into the true pelvis by the primary operating surgeon who eventually referred the case to our institute. It was successfully retrieved by our operating team using an anterior modified Stoppa’s approach under fluoroscopic guidance.
Case Report
A 2-year-old female child was referred to our institute by a local hospital with an alleged history of fall on the buttocks while playing at home 12 days previously. She landed hard directly on a tapestry needle which was lying unattended on a cot, resulting in the needle penetrating the left buttock. At the local hospital, the child was given first aid care, tetanus prophylaxis, and broad-spectrum intravenous antibiotics after admission. The needle was apparently deeply embedded in the gluteal muscles, and the end of the needle was not visible or palpable. 1 week later, they attempted surgical retrieval of the needle using a posterior undefined approach through the left buttock. However, with every attempt to grab the eye of the needle, the needle was inadvertently pushed further anteriorly, and the surgeon eventually abandoned the procedure. The child was referred to our institute 5 days later by the primary surgical team. On presentation, the child complained of dull, aching pain in the left buttock region and the left groin region; tenderness could be elicited at the entry site of the needle. The pain was significant as the child avoided sitting or standing/walking due to the pain and preferred to lie still in the bed; hip range of motion was normal, and there was no distal neurovascular deficit. She had no history of fever, urinary, or bowel disturbances. An oblique scar, 4 cm in length, indicative of the previous surgery was seen in the left buttock region (Fig. 1).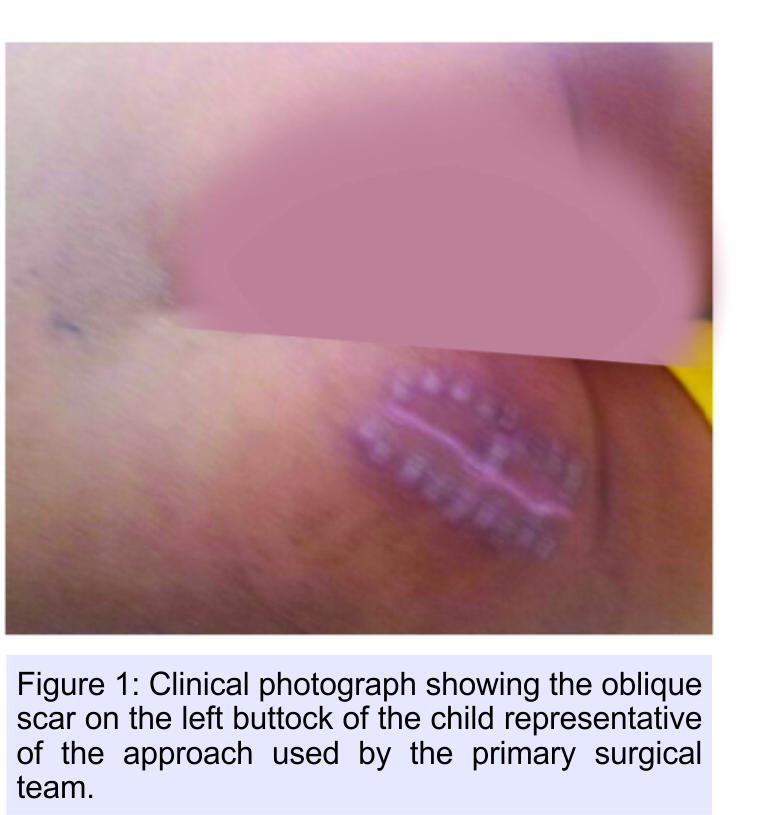 Fresh radiographs of the pelvis including an anteroposterior view, Judet views, pelvis inlet, and outlet views were obtained to ascertain the current position of the needle. The needle was located well within the true pelvic cavity, lying just medial to the left obturator foramen (Fig. 2). Computerized tomogram images with three-dimensional reconstruction were obtained to accurately locate the needle position inside the true pelvis (Fig. 3).
Fresh radiographs of the pelvis including an anteroposterior view, Judet views, pelvis inlet, and outlet views were obtained to ascertain the current position of the needle. The needle was located well within the true pelvic cavity, lying just medial to the left obturator foramen (Fig. 2). Computerized tomogram images with three-dimensional reconstruction were obtained to accurately locate the needle position inside the true pelvis (Fig. 3).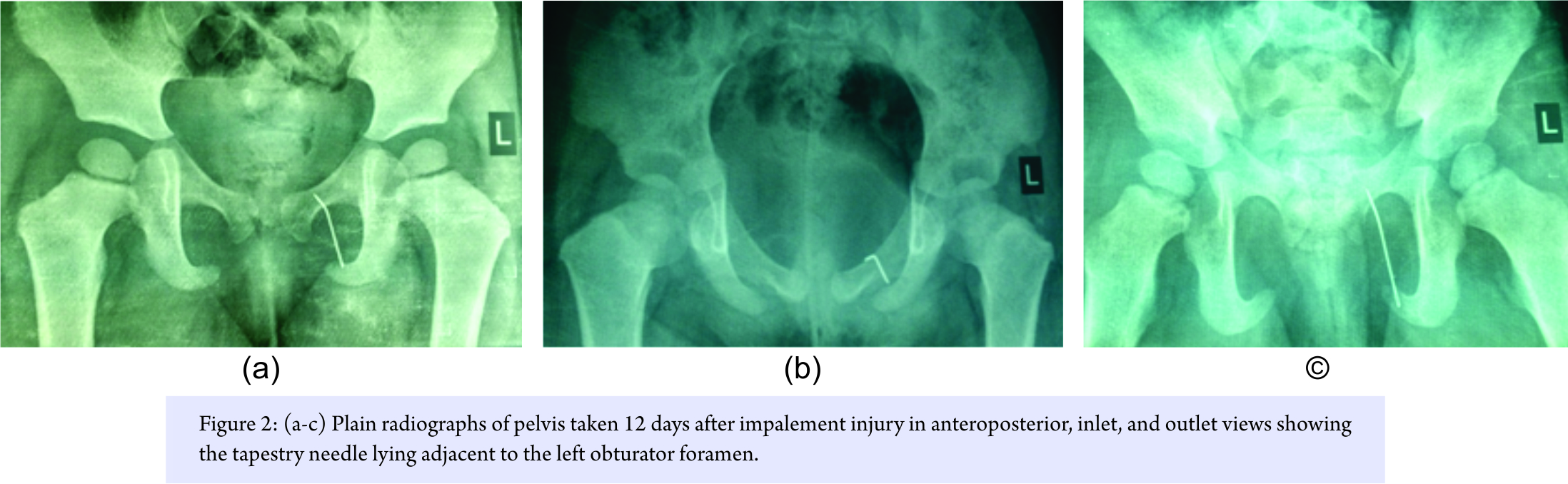
We decided to operate and retrieve the needle from the pelvis due to 3 reasons. First, the needle was in close proximity to the urinary bladder and obturator neurovascular bundle, and chances of further migration of the needle could not be ruled out completely [4, 5]. For the same reason, minimally invasive computed tomography (CT)-guided removal of needle also was not considered safe by the radiologist. Second, the needle could act as a focus of infection leading to abscess formation and/or sepsis [6, 7]. Furthermore, the embedded needle could later present as a chronic source of pain and discomfort for the patient [8, 9, 10, 11, 12].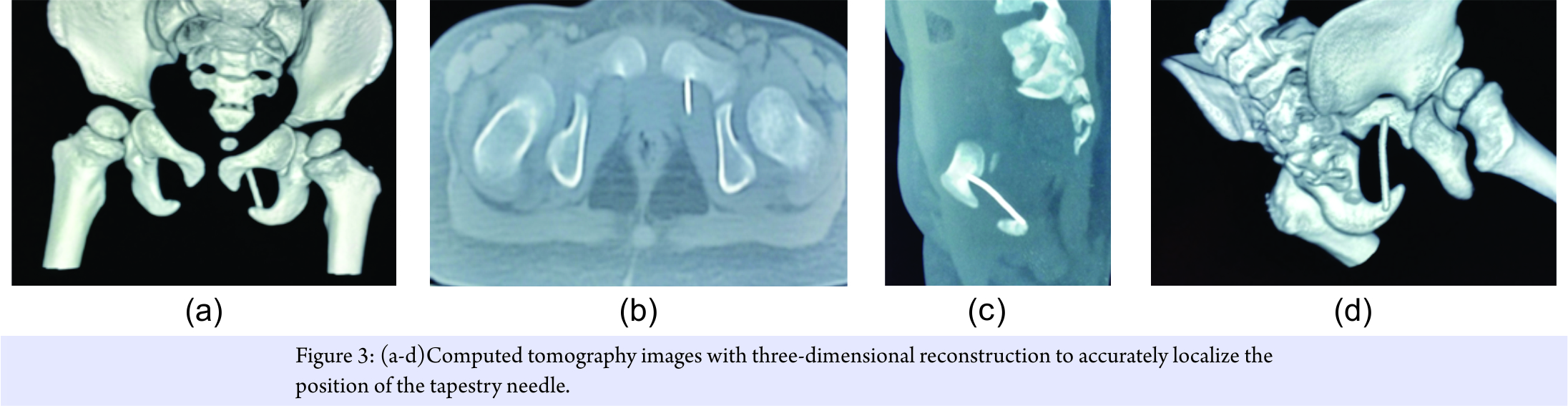
Surgical technique
We used the modified Stoppa’s approach for the surgical retrieval of the impaled needle [13, 14]. A Foley’s catheter was inserted before surgery to improve the visualization. The patient was positioned supine on a radiolucent table. The entire left lower limb and the lower abdomen were aseptically draped for the surgery, and the left hip was flexed by placing a sandbag beneath the left knee to relax the iliopsoas and abdominal muscles and also the external iliac/femoral neurovascular bundle. A transverse, linear skin incision of around 8 cm was made 2 cm proximal to the pubic symphysis, just short of the external inguinal ring, and the incision was deepened to the abdominal fascia. The rectus fascia was incised transversely, and the exposed rectus abdominis muscle was split along the linea alba to approach the internal aspect of the pelvis. We then split the transversalis fascia to enter the potential space of Retzius (Fig. 4).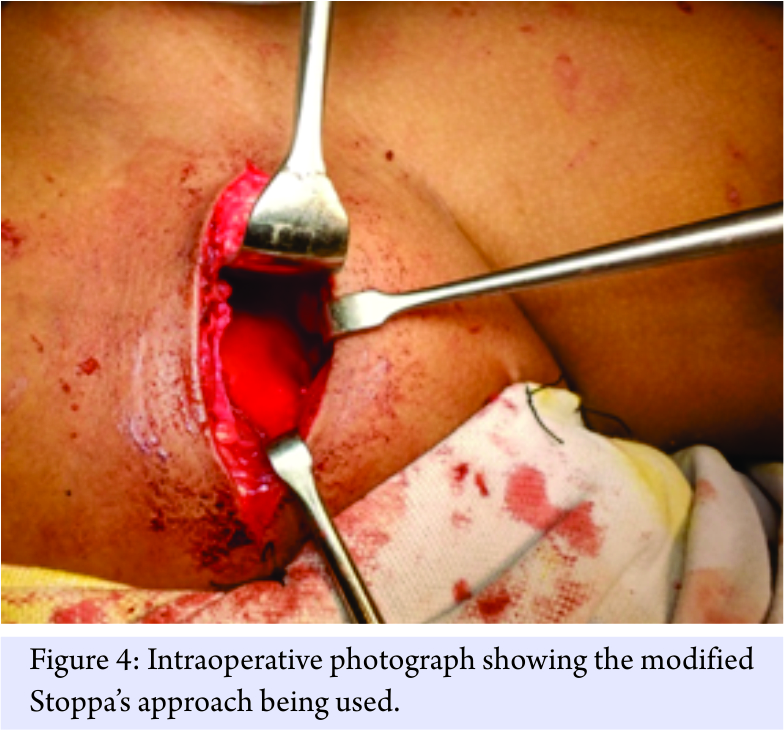
The needle was located under fluoroscopic guidance in anteroposterior, inlet, and outlet views (Fig. 5). It was found to be embedded within the substance of the obturator internus muscle, medial to the left obturator foramen with the sharp end of the needle lying around 2 cm lateral to the symphysis and around 1 cm inferior to the superior margin of the superior pubic ramus.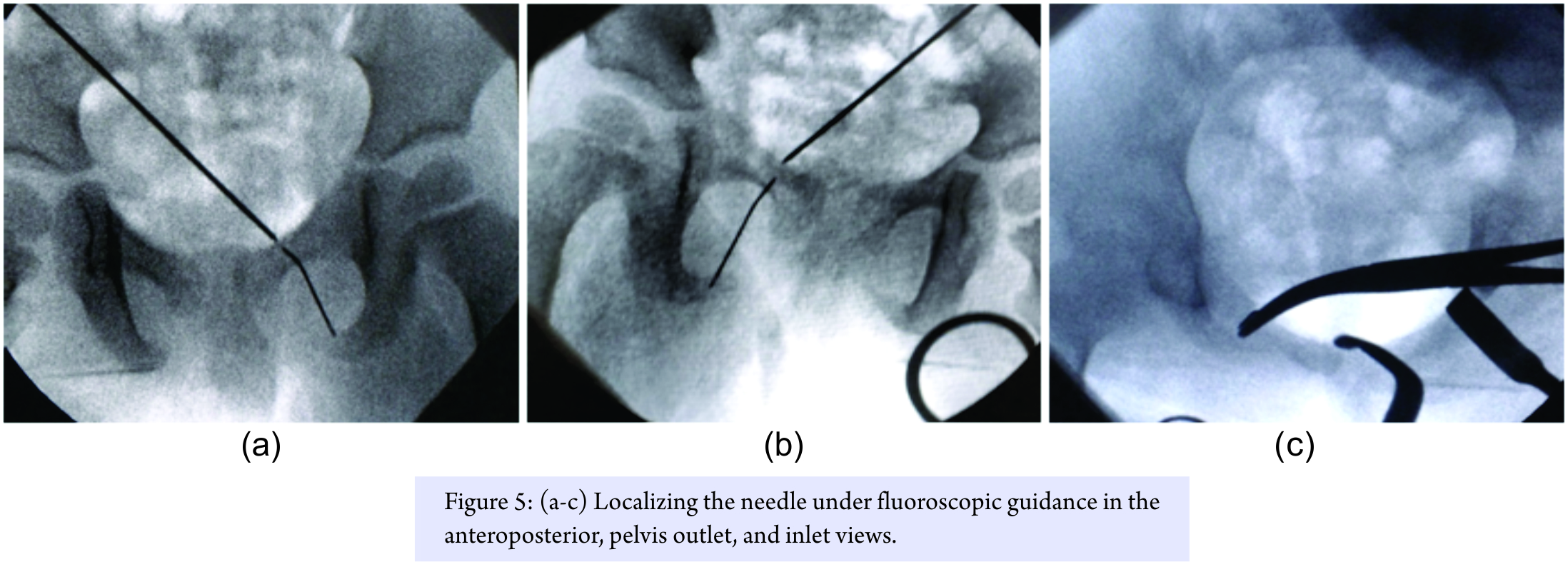
A small incision was given over the fascia of the obturator internus muscle over the needle; the needle was gripped firmly in the middle part using a needle holder forceps and not at its tip to prevent it from retreating back along the preformed tract (Fig. 6). The needle was gently extracted upward, and it came out without much difficulty. The tapestry needle was carefully examined to check if it was extracted in its entirety. It was noted that the needle was 3.6 cm in length and there was a significant amount of corrosion on it which theoretically increases the risk of anaerobic infections (Fig. 7). A thorough wash with 4 L of normal saline was given, and the wound was closed in layers over a suction drain.

Post-operatively, the child was started on triple intravenous antibiotics (cefuroxime, amikacin, and clindamycin) for 5 days. No signs of wound infection were noted, and the sutures were removed 12 days after surgery. Rest of the post-operative period was uneventful.
Discussion
A careful search of the available medical literature did not reveal any similar case reported in the pediatric or adult population. Most of the impalement injuries of the pelvis in children are usually caused by larger objects. Habelt et al. [7] reported 2 young boys with perineal impalement injuries after a history of a fall on the buttocks. In both cases, wooden foreign bodies were lodged in the perineal areas leading to inflammation which necessitated surgical drainage. Ekenze et al. [6] reported a 13-year-old child who suffered a perineal impalement injury with a writing pen which was incompletely extracted by a primary health-care practitioner; the child presented with signs of chronic urinary tract infection 4 months later. A radiopaque object was detected in the urinary bladder on pelvic radiograph and sonograph; on surgical exploration, a 7.5 cm encrusted fragment of the writing pen was extracted from the inflamed bladder cavity. The authors postulated that the retained foreign body in the bladder was most probably secondary to direct penetration of the bladder cavity, but the possibility of upward migration along the urinary tract could not be ruled out. Baeza-Herrera et al. [15] reported on 2 children with traumatic inguinal impalement injuries with a metallic bar and a wooden stake without any distal neurovascular deficit or any visceral/testicular damage; both these foreign bodies, however, were subcutaneous in location and were surgically removed without any complications. No traumatic needle impalement injury of the pelvis has been reported in adults or in children to the best of the authors’ knowledge. Plager et al. [8] reported on two boys with diabetes mellitus with retained metallic needles in the soft tissue of the buttock region which were part of a subcutaneous insulin delivery system and which apparently broke away from the rest of the infusion set during removal. The children were asymptomatic, and the needles were removed surgically under fluoroscopic guidance; however, unlike our case, the location of the metallic needles was quite superficial and well outside the pelvic cavity. In our case, the initial management of the child after the injury in the referring hospital was improper and inadequate; this may reflect the lack of trained personnel that is present in many hospitals in developing countries like India. The child would have benefited from detailed and careful pre-operative planning, proper surgical approach, wound exploration, wound irrigation, and layered closure. She should have been promptly referred to a tertiary care center if the facilities or personnel at the treating hospital were inadequate.
Conclusions
Needle impalement injuries of pelvis are very rare and unusual. Being a relatively small object, it is more likely to completely penetrate into the soft tissue, and the ends of the needle may not be seen or palpated. When faced with such cases, it is imperative not to rush into surgery. Adequate analgesia, tetanus prophylaxis, antibiotics, and immobilization must be given initially followed by meticulous pre-operative planning in the form of radiographs (in multiple views) and CT scans (including angiogram if needed). Minimally invasive CT-guided extraction of needle can be attempted by an experienced interventional radiologist when there is no significant risk of damaging neighboring vital organs or neurovascular structures. The surgical approach if an open approach is decided must be chosen wisely; backup may be needed from an abdominal surgeon, urologist, or gynecologist in certain cases. The needle should never be grasped from the tip as that will only push it further inside which might lead to catastrophic complications. It should be gripped in the middle and stabilized, and only then, an attempt must be made to pull it out.
Clinicla Message
In needle impalement injuries, do not rush patient into operating theater without adequate planning and backup. Try minimally invasive CT-/ultrasonography-guided extraction of the object, if feasible. Choose surgical approach carefully. Do not try to grasp the needle from the tip.
References
1. Oya S, Miyata K, Yuasa N, Takeuchi E, Goto Y, Miyake H, et al. Impalement injury to the left buttock with massive bleeding: A case report. Nagoya J Med Sci 2013;75:147-52.1. Oya S, Miyata K, Yuasa N, Takeuchi E, Goto Y, Miyake H, et al. Impalement injury to the left buttock with massive bleeding: A case report. Nagoya J Med Sci 2013;75:147-52.
2. Pelayo F, Gross RG. Diccionario Usual. México: Larousse; 1994. p. 216.
3. Baeza CH, Osorio DC, Cortés HR, González AL, Godoy AH. Traumatic Oral Cavity Injury in Children. Pediatric Act of Mexico 2001;22:15-8.
4. Gibbs VC, Coakley FD, Reines HD. Preventable errors in the operating room: Retained foreign bodies after surgery-Part I. Curr Probl Surg 2007;44:281-337.
5. Reinmuth N, Förster R, Scheld HH. From the neck to the lung: Pneumothorax caused by a lost needle. Eur J Cardiothorac Surg 1995;9:216-7.
6. Ekenze SO, Ezomike UO, Offor I, Enyanwuma IE. Transperineal migration of a portion of a writing pen into the urinary bladder. Afr J Paediatr Surg 2010;7:121-3.
7. Habelt S, Berberich T, Mayr J. Impalement injury: A case report of two young boys. Injury Extra 2008;39:120-2.
8. Plager P, Murati MA, Moran A, Sunni M. Two case reports of retained steel insulin pump infusion set needles. Pediatr Diabetes 2016;17:160-3.
9. Jayadevan R, Stensland K, Small A, Hall S, Palese M. A protocol to recover needles lost during minimally invasive surgery. JSLS 2014:18:e201400165.
10. Malhotra N, Roy KK, Sinha A. Forgotten needle-An unusual cause of chronic pelvic pain. Arch Gynecol Obstet 2003;269:68-9.
11. Hösli I, Tercanli S, Holzgreve W. Complications of lost needle after suture of vaginal tear following delivery. Arch Gynecol Obstet 2000;264:159-61.
12. Kleinpeter SJ, Kline RC, Finan MA. Retained surgical needle in the perineum. Report of a case with a novel method of search and rescue. J Reprod Med 1997;42:303-5.
13. Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res 1994;305:112-23.
14. Hirvensalo E, Lindahl J, Böstman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res 1993;297:28-32.
15. Baeza-Herrera C, Medellín-Sierra UD, Domínguez-Pérez ST, Atzín-Fuentes JL, García-Cabello LM. Inguinal impalement. Report of two cases. Cir Cir 2008;76:83-6.
 |
 |
 |
 |
| Dr. Nirmal Raj Gopinathan | Dr. Rakesh John | Dr. Himanshu Kanwat | Prof. Pebam Sudesh |
| How to Cite This Article: Gopinathan NR, John R, Kanwat H, Sudesh P. Surgical Retrieval of an Impaled Tapestry Needle from the True Pelvic Cavity of a Child – An Unusual Case Report. Journal of Orthopaedic Case Reports 2017 Sep-Oct ; 7(5): 24-28 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




