[box type=”bio”] What to Learn from this Article?[/box]
The delayed presentation of superior mesenteric artery syndrome in spite of uneventful early post-operative period, to be kept in mind.
Case Report | Volume 7 | Issue 5 | JOCR Sep – Oct 2017 | Page 67-70 | Surya Prakash Rao Voleti, Jakkepally Sridhar. DOI: 10.13107/jocr.2250-0685.898
Authors: Surya Prakash Rao Voleti [1], Jakkepally Sridhar [1]
[1] Department of Orthopaedics and Spine Surgery, Maxcure Hospitals, Madhapur, Telangana. India.
Address of Correspondence
Dr. Jakkepally Sridhar,
Department of Orthopaedics and Spine Surgery,
Maxcure Hospitals, Madhapur, Telangana. India.
E-mail: sridhar.gmc@gmail.com
Abstract
Introduction: Obstruction of the third part of duodenum by superior mesenteric artery is known as superior mesenteric artery syndrome. Incidence of superior mesenteric artery syndrome following spine deformity correction is 0.5–4.7%. Till now, this syndrome after isolated kyphosis correction with vertebral column resection is rarely reported in literature.
Case Report: A 17-year-old male patient with normal body habitus presented with 80° of congenital thoracolumbar kyphosis. He underwent kyphosis correction with vertebral column resection and posterior instrumentation and posterior spinal fusion under neuro monitoring. Deformity correction was excellent; the patient was alright in immediate post-operative period. 2 weeks after surgery presented with repeated vomiting and abdominal pain. Contrast computed tomography was showing decreased aortomesenteric angle and decreased aortomesenteric distance which confirmed the diagnosis of superior mesenteric artery syndrome. Initial management was conservative, but as symptoms were progressive, duodenojejunostomy was done. The patient was completely recovered from obstructive symptoms.
Conclusion: Superior mesenteric artery syndrome is a life-threatening complication that can occur after spine deformity correction. Early recognition and appropriate measures are critical to prevent the development of severe complications including death.
Keywords: Superior mesenteric artery syndrome, aortomesenteric angle, aortomesenteric distance.
Introduction
Superior mesenteric artery syndrome is a rare complication after spine deformity correction. This syndrome was first described by von Rokitansky in 1842 [1] and termed to as “superior mesenteric artery syndrome” by Wilkie. This vascular obstruction of the third part of duodenum by superior mesenteric artery leading to gastric outlet obstruction is known as superior mesenteric artery syndrome. Obstruction of the small bowel by superior mesenteric artery is associated with spinal manipulation in conservative or surgical management of scoliosis, in extensive burns, major surgeries, severe trauma, malignancies, and following application of spica casts. The incidence of superior mesenteric artery syndrome is 1–4.7% [2, 3]. This syndrome presents with pain, immediate postprandial bilious vomiting, and abdominal bloating. Signs of superior mesenteric artery syndrome develop 5–10 days after spine deformity correcting procedure. Secondary complications include poor wound healing secondary to poor nutrition, delayed recovery. The syndrome may progress to serious sequelae with mortality rate of 33% [4]. This is common in patients with low body weight relative to height [5]. Malnourished patients experiencing increase in height after surgery relative to weight after surgery are more susceptible to this.
We present a patient with superior mesenteric artery syndrome who presented late (2 weeks) following correction of congenital kyphosis with vertebral column resection.
Case Report
A 17-year-old male patient presented with progressive spinal deformity. He had difficulty in lying down on the back due to the hump. The deformity was noted since childhood and was progressing gradually. The rest of the history was unremarkable. On physical examination, the patient had severe kyphosis with apex at thoracolumbar junction. His anthropometric measurements were noted, which include, body weight-50 kg, standing height-160 cm, sitting height-80 cm, and arm span-166 cm. Body mass index (BMI) was 19.56, which was 33 percentile of age- and sex-matched controls. The patient had no limb length discrepancy and neurologically intact. Kyphotic angle as measured by Cobb’s method was 80° (Fig. 1 and 2).
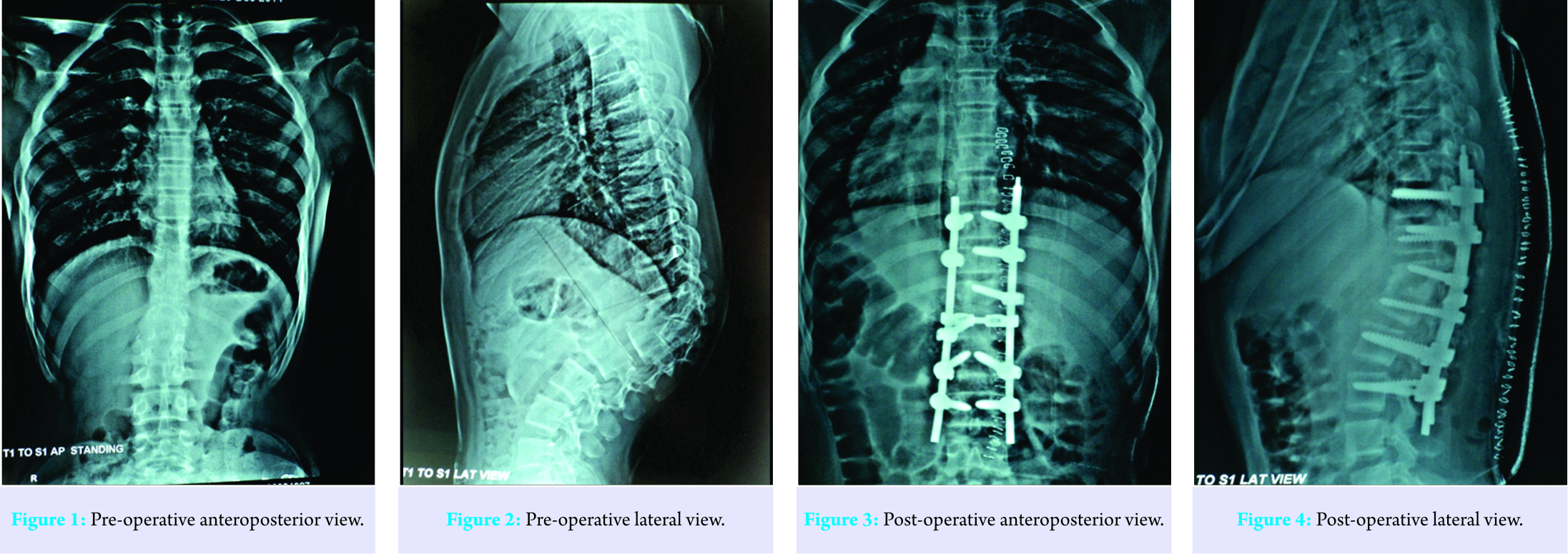
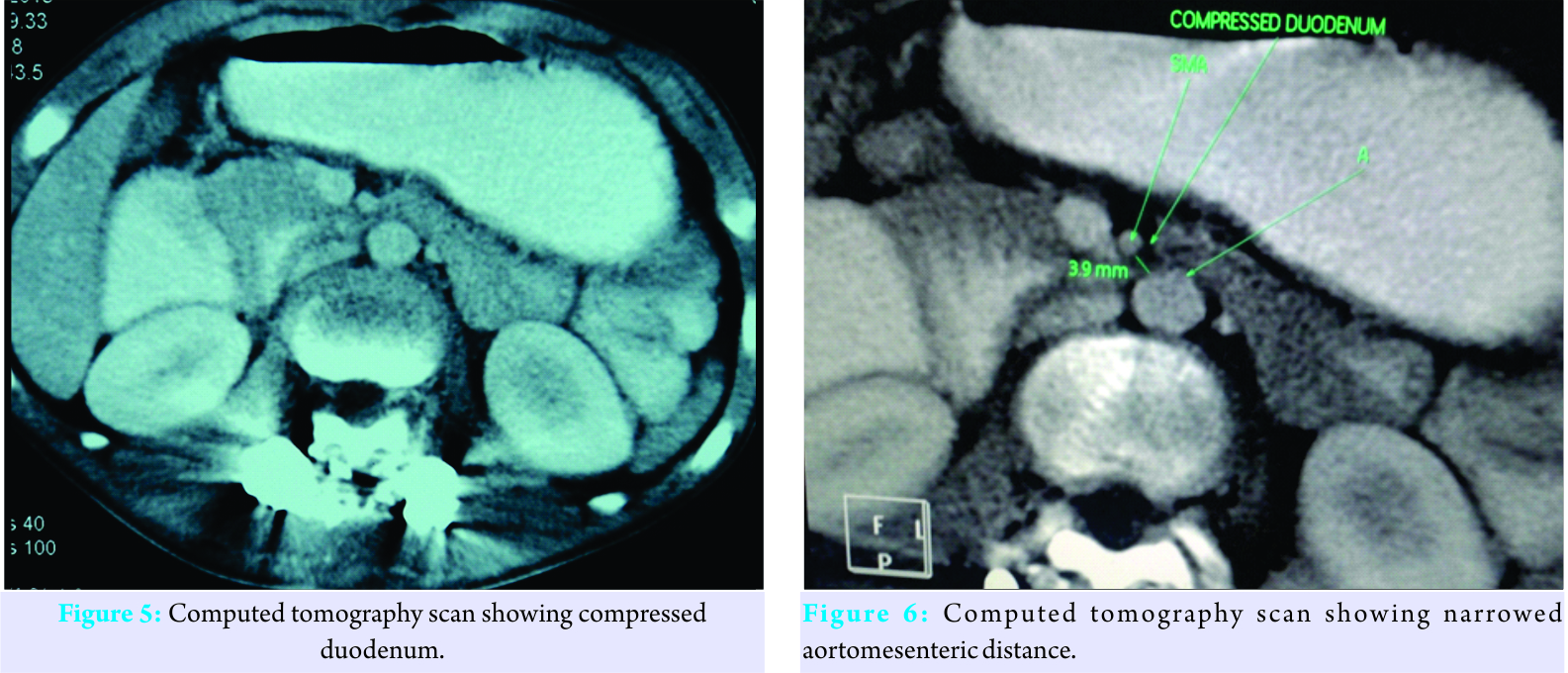
Magnetic resonance imaging was done and it is within normal limits. Pre-operative work up is within normal limits. He was taken up for deformity correction surgery. He underwent kyphosis correction with vertebral column resection at T12, along with posterior instrumentation and posterior spinal fusion under neuromonitoring. Intraoperative blood loss was around 1000 ml. Intraoperative and post-operative course was uneventful. Excellent correction of kyphosis was obtained (Fig. 3 and 4). Immediate post-operative period was uneventful. 2 weeks following surgery patient presented to us with severe nausea, persistent vomiting, and abdominal pain. He was dehydrated with severe electrolyte disorders including hypokalemia and metabolic alkalosis. His body weight had dropped further to 47 kg. On clinical examination, his abdomen was considerably distended but was soft and non-tender. Bowel sounds were normally heard. Radiological investigations were done as advised by general surgeon. Barium studies, ultrasound abdomen and, were suggestive of superior mesenteric artery syndrome. Contrast computed tomography was done, which was showing narrowed aortomesenteric angle (15°) and narrowed aortomesenteric distance (3.9 mm), which clinched the diagnosis of superior mesenteric artery syndrome (Fig. 5 and 6). Nasogastric tube applied and decompression done patient was initially managed conservatively with correction of dyselectrolytemia and was given total parenteral nutrition. As there was no improvement with the conservative care surgical intervention was done. As the superior mesenteric artery was found compressing the third part of duodenum, a gastrojejunostomy was done by passing the block. Duodenal secretion can still drain into the jejunum. With 2–3 days, the patient’s symptoms completely subsided and patient discharged in stable condition. At follow-up, the patient is doing well and was gaining weight. 1 year after surgery patient’s body weight and BMI was improved significantly (BMI 19.3).
Discussion
The superior mesenteric artery syndrome is related to the anatomy of the third part of the duodenum. The superior mesenteric artery is the second branch of aorta. It arises from the aorta at L1 and L2 region. The third part of duodenum starts at the level of L3 and passes in the aortomesenteric angle. The duodenum is supported in this aortomesenteric junction by ligament of Treitz [5]. Normal aortomesenteric distance is 10–34 mm and normal aortomesenteric angle is 28–65° [6]. Any intervention which alters the normal relationship between aorta, superior mesenteric artery and duodenum will cause compression of the duodenum. Normally, the duodenum is surrounded by pad of fat which cushions it. Any conditions that cause depletion of fat around the duodenum such as malnutrition and burns, patients with long-standing paraplegia or quadriplegia are more prone for this [7] condition. This is also common in patients with hip spica or body cast application [8]. This is also common after spine deformity correction secondary to acute alteration of aortomesenteric angle and aortomesenteric distance [9]. As per some studies, the patients with thin body habitus are more prone for superior mesenteric artery syndrome after deformity correction surgery [10], but as per Hutchinson and Bassett [11] there is no relation between body habitus and superior mesenteric artery syndrome. Our patient has decent BMI and was not asthenic. We did not check the pre-operative aortomesenteric angle and aortomesenteric distance in this patient. Patient presents with severe abdominal pain and vomiting after surgery. Some patients may present immediately after surgery, during the first or second post-operative day and some patients present late. Vomiting will be bilious and increased nasogastric aspirate present usually. Abdomen is usually soft on palpation and mild tenderness in epigastric region. Bowel sounds are normal or exaggerated [8]. Vomiting reduces the symptoms and patient will have episodes of symptomatic relief. Major differential diagnosis for this condition is post-operative ileus, which is secondary to general anesthesia and electrolyte imbalance [2], but the symptoms of ileus will start during the immediate post-operative period and relieved after 3–5 days. In our patient, symptoms started after 2 weeks. Initial treatment of superior mesenteric artery syndrome should be conservative [8]. The oral intake should be restricted and the nasojejunal tube inserted distal to the site of obstruction. The electrolyte imbalance and dehydration should be treated with appropriate IV fluids. Usually, the symptoms will get better in 2–3 days with appropriate conservative treatment, when the symptoms continuously worsening the surgical intervention is needed. Surgical methods for correction of this include duodenojejunostomy, division of Treitz ligament. Cause of death in superior mesenteric artery syndrome is due to aspiration pneumonia, acute gastric rupture, severe electrolyte imbalance, hypokalemia, and cardiovascular collapse [5, 12]. In our center, where we operate around 80 deformities per year, this is the 1st time we faced this problem in past 15 years. Post-operative weight loss could be implicated as a cause in our patient. Till now, there are studies which reported the superior mesenteric artery syndrome after scoliosis surgeries. As per Kim et al. [2], the incidence of superior mesenteric artery syndrome after scoliosis correction is 1–4.7%. Qian et al. [13] studied anatomical relationship of superior mesenteric artery and aorta before and after surgical correction of thoracolumbar kyphosis and concluded that aortomesenteric angle and aortomesenteric distance decreased significantly after kyphosis correction. However, there is no report of superior mesenteric artery syndrome after isolated kyphosis correction with vertebral column resection.
Conclusion
Superior mesenteric artery syndrome is not uncommon in patients undergoing scoliosis/kyphosis correction surgeries and needs to be evaluated if the patient presents with symptoms. As it is rare, the routine pre-operative investigation may not be indicated. Any post-operative patient who undergoes spinal deformity correction, if presents with upper gastrointestinal symptoms along with weight loss, it is prudent to rule out superior mesenteric artery syndrome. Once diagnosed, it needs proper intervention. Initial treatment could be conservative and surgical treatment will invariably yield good results.
Clinical Message
For the average spinal deformity surgeon, superior mesenteric artery syndrome has been so rare that it is usually encountered in textbooks only. Surgeons understand it as cast syndrome following plaster application for scoliosis correction, which is now obsolete. The idea that such an entity should be considered in asthenic individuals who undergo corrections for significant spinal deformity, is important. Most of these respond to conservative care and surgical exploration is considered rare. In this case report, we present a case of superior mesenteric artery syndrome following kyphosis correction which ultimately needed surgical intervention. Following intervention, the patient had an uneventful recovery and full resolution of symptoms.
References
1. Rokitansky C. Handbuch der Pathologischen Anotomie. Vienna: Branmiller and Siedel; 1842.
2. Kim JY, Kim HS, Moon ES, Park JO, Shin DE, Lee GK, et al. Incidence and risk factors associated with superior mesenteric artery syndrome following surgical correction of scoliosis. Asian Spine J 2008;2:27-33.
3. Braun SV, Hedden DM, Howard AW. Superior mesenteric artery syndrome following spinal deformity correction. J Bone Joint Surg Am 2006;88:2252-7.
4. Boseker EH, Moe JH, Winter RB, Koop SE. Determination of “normal” thoracic kyphosis: A roentgen graphic study of 121 “normal” children. J Pediatr Orthop 2000;20:796-8.
5. Zhu ZZ, Qiu Y. Superior mesenteric artery syndrome following scoliosis surgery: Its risk indicators and treatment strategy. World J Gastroenterol 2005;11:3307-10.
6. Inal M, Daphan BU, Bilgili MY. Superior mesenteric artery syndrome associated with nutcracker syndrome: A case report. Iran Red Crescent Med J 2014;16:e14755.
7. Laffont I, Bensmail D, Rech C, Prigent G, Loubert G, Dizien O, et al. Late superior mesenteric artery syndrome in paraplegia: Case report and review. Spinal Cord 2002;40:88-91.
8. Tsirikos AI, Anakwe RE, Baker AD. Late presentation of superior mesenteric artery syndrome following scoliosis surgery: A case report. J Med Case Rep 2008;2:9.
9. Crowther MA, Webb PJ, Eyre-Brook IA. Superior mesenteric artery syndrome following surgery for scoliosis. Spine (PhilaPa 1976) 2002;27:E528-33.
10. Munns SW, Morrissy RT, Golladay ES, McKenzie CN. Hyper alimentation for superior mesenteric-artery (cast) syndrome following correction of spinal deformity. J Bone Joint Surg Am 1984;66:1175-7.
11. Hutchinson DT, Bassett GS. Superior mesenteric artery syndrome in pediatric orthopedic patients. Clin Orthop Relat Res 1990;250:250-7.
12. Todd SR, Marshall GT, Tyroch AH. Acute gastric dilatation revisited. Am Surg 2000;66:709-10.
13. Qian BP, Ji ML, Jiang J, Zhu ZZ, Wan B, Qiu Y, et al. Anatomic relationship between superior mesenteric artery and aorta before and after surgical correction of thoracolumbar kyphosis. J Spinal Disord Tech 2013;26:E293-8.

| How to Cite This Article: Voleti SPR, Sridhar J. Superior Mesenteric Artery Syndrome after Kyphosis Correction – A Case Report. Journal of Orthopaedic Case Reports 2017 Sep-Oct;7(5):67-70 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




