[box type=”bio”] Learning Point for this Article: [/box]
Isolated medial compartment osteoarthritis after remote patellectomy can be treated effectively with robot-assisted medial compartment arthroplasty.
Case Report | Volume 8 | Issue 1 | JOCR Jan – Feb 2018 | Page 11-14 | Shalen Kouk, Irene Kalbian, Elizabeth Wolfe, Sabrina M Strickland. DOI: 10.13107/jocr.2250-0685.976
Authors: Shalen Kouk[1], Irene Kalbian[2], Elizabeth Wolfe[2], Sabrina M Strickland[3]
[1]Department of Orthopaedic Surgery, NYU Hospital for Joint Diseases, New York, USA.
[2]Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, USA.
[3]Department of Orthopaedic Surgery and Sports Medicine, Hospital for Special Surgery, New York, USA.
Address of Correspondence:
Dr. Sabrina M. Strickland,
Hospital for Special Surgery,523 E 72nd Street, New York, NY 10021, USA.
E-mail: Stricklands@hss.edu
Abstract
Introduction: Total patellectomies are uncommon procedures that are reserved as salvage treatment for severely comminuted fractures of the patella. Due to the alteration of normal joint mechanics, these patients present later on in life with degenerative cartilage damage to the femorotibial joint and altered extensor mechanism. There are very few reports of unicondylar knee arthroplasties following previous patellectomy and none that specifically address robot-assisted unicompartmental knee arthroplasty. A recent case report by Pang et al. described the use of minimally invasive fixed-bearing unicondylar knee arthroplasty in a patellectomized patient with moderate medial compartment osteoarthritis. Our report details a case with more significant chondral loss along with patellar tendon subluxation.
Case Report: This is a case report of a patient with severe medial compartment osteoarthritis after a patellectomy following a motor vehicle collision. After failing conservative treatment, the patient underwent a medial MAKOplasty with complete resolution of arthritic pain.
Conclusion: Significant pain relief and improved knee function can be achieved with MAKOPlasty partial knee resurfacing system in a previously patellectomized patient with severe medial compartment osteoarthritis.
Keywords: Robot-assisted, unicondylar, arthroplasty, patellectomy, MAKOplasty.
Introduction
Patellectomies have historically been used as salvage treatment for severely comminuted fractures of the patella but have also been used as a surgical treatment option for chondromalacia patella, osteoarthritis, and recurrent patellar dislocations [1]. However, the resulting alteration of knee biomechanics from the procedure can lead to progressive, degenerative cartilage damage years later [2,3,4]. While there have been studies recommending reconstruction of the patella and total knee arthroplasty as treatment options for patients status post-patellectomy[5, 6, 7, 8], there are very few reports discussing the use of unicondylar knee arthroplasty as a treatment option [9, 10, 11]. A systematic review of the literature revealed only one case report discussing the procedure within the past 20 years [12]. Pang et al. discussed the use of minimally invasive unicondylar knee arthroplasty in a patellectomized patient and found good quadriceps strength without knee pain or instability 5years post-arthroplasty. This case report differs both in the severity of gonarthrosis, the instability of the quad/patellar tendon as well as in the surgeon’s use of robot assistance for the arthroplasty. Robotic assistance for arthroplasty has been shown to have better precision than the manual technique with good short-term clinical and radiological outcomes [13, 14, 15].
Case report
A 60-year-old female initially presented to the office complaining of worsening right knee pain dating back to a motor vehicle accident in 1975 that resulted in a shattered right patella and subsequent patellectomy. Before injury, the patient had no right knee pain or extensor mechanism dysfunction. Postoperatively, the patient remained fairly pain-free with symptoms of quad/patellar tendon subluxation resulting in a non-painful pop over the lateral aspect of her distal femur during flexion including ascending and descending stairs that had been present since her patellectomy. 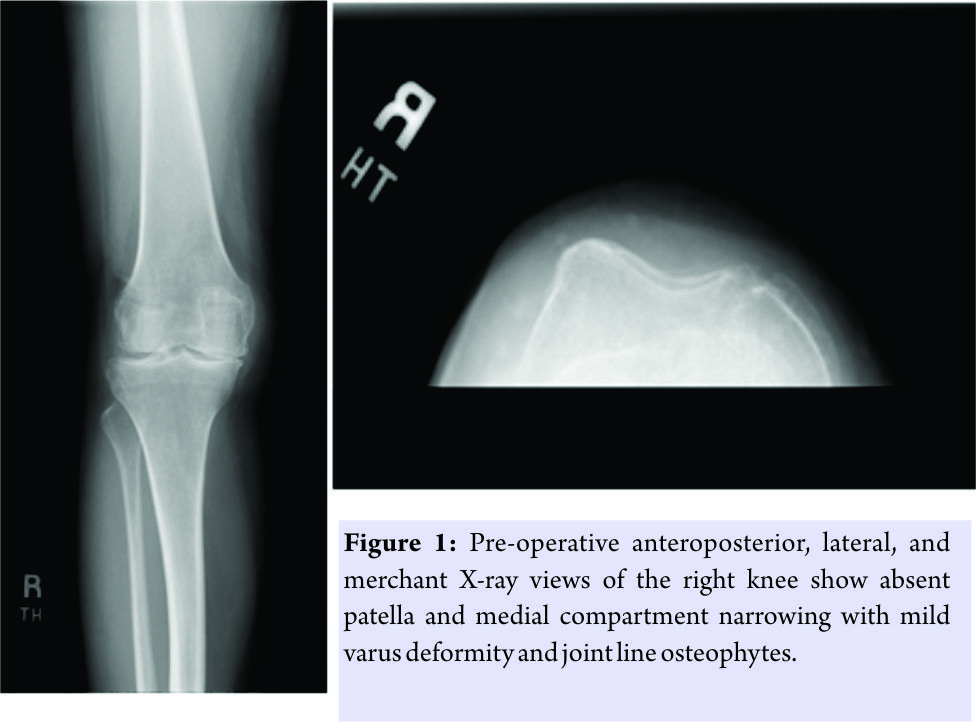 Approximately 6 months before presentation, the patient noticed increased medial sided pain but denied any pain anteriorly or pain with subluxation of the patellar tendon. She was treated conservatively with physical therapy and a medial unloader knee brace but returned to the clinic 2years later with worsening pain that began to significantly affect her activities of daily living.The patient has a body mass index of 20. Her past medical history is significant for diabetes and negative for tobacco use. The patient’s past surgical history is significant for patellofemoral arthroplasty on the contralateral knee. On examination, the patient ambulated with a normal gait and had 5/5 distal motor strength of the extensor hallucislongus, tibialis anterior, and gastrocnemius bilaterally. Sensation was intact to the L1 through S1 dermatomes. Knee range of motion was 0–135°, without extensor lag. The knee was stable to varus and valgus stress with 1A Lachman and posterior drawer tests. The patient had significant medial joint line tenderness to palpation, no pain laterally or anteriorly. On flexion, the patellar tendon subluxed laterally out of the trochlear groove at about 80°. Bilateral hip examination showed no abnormalities. Examination of the contralateral knee was unremarkable, with good clinical result status post-patellofemoral arthroplasty. The right knee radiographs, including anteroposterior, lateral, merchant, and posteroanterior views, revealed an absent patella, medial compartment narrowing with mild, correctible varus deformity of approximately 5° and medial joint line osteophytes (Fig. 1). Magnetic resonance imaging of the right knee confirmed that the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL) were intact. There was diffusely exposed bone over the weight-bearing medial femoral condyle and tibial plateau. The trochlear sulcus was hypoplastic with exposed bone over the central portion and chronic remodeling of the anterior inferior margin. The lateral and patello femoral compartments were without any significant osteoarthritic changes with no chondral defects or degeneration. Finally, the patellar tendon was laterally subluxed over the anterolateral trochlear margin on extension views (Fig. 2). To track knee function preoperatively and postoperatively, the patient completed the previously validated International Knee Documentation Committee (IKDC) subjective knee evaluation form. After discussing the imaging results with the patient, we reviewed potential operative management following her failed course of conservative management. The risks and benefits of quadriceps realignment versus unicondylar knee arthroplasty versus total knee arthroplasty were discussed at length with the patient. We decided to proceed with a unicondylar knee arthroplasty of the medial compartment utilizing the MAKOplasty partial knee resurfacing system. The patient had compensated for her patellar tendon subluxation for >20 years, and the decision was made to leave the patellar tendon tracking alone rather than perform a soft tissue alignment which could have limited knee flexion, causing the tendon to rub, or abrade the trochlea and lead to a new source of pain and disability. At the time of surgery, the patient was placed in a supine position and a well-padded tourniquet was placed around the proximal right thigh. The limb was prepped and draped and a time-out procedure was completed along with confirmation of Ancef (Cefazolin) administration. Two pins were then drilled in the tibia and femur for the attachment of the MAKO arrays. The limb was then exsanguinated and the tourniquet was inflated to 250mmHg. A median prepatellar approach was utilized and a 7cm incision was made along the anteromedial aspect of the knee. A minimal medial release was then completed. Retractors were placed and the appropriate data points were collected using the MAKO system array.
Approximately 6 months before presentation, the patient noticed increased medial sided pain but denied any pain anteriorly or pain with subluxation of the patellar tendon. She was treated conservatively with physical therapy and a medial unloader knee brace but returned to the clinic 2years later with worsening pain that began to significantly affect her activities of daily living.The patient has a body mass index of 20. Her past medical history is significant for diabetes and negative for tobacco use. The patient’s past surgical history is significant for patellofemoral arthroplasty on the contralateral knee. On examination, the patient ambulated with a normal gait and had 5/5 distal motor strength of the extensor hallucislongus, tibialis anterior, and gastrocnemius bilaterally. Sensation was intact to the L1 through S1 dermatomes. Knee range of motion was 0–135°, without extensor lag. The knee was stable to varus and valgus stress with 1A Lachman and posterior drawer tests. The patient had significant medial joint line tenderness to palpation, no pain laterally or anteriorly. On flexion, the patellar tendon subluxed laterally out of the trochlear groove at about 80°. Bilateral hip examination showed no abnormalities. Examination of the contralateral knee was unremarkable, with good clinical result status post-patellofemoral arthroplasty. The right knee radiographs, including anteroposterior, lateral, merchant, and posteroanterior views, revealed an absent patella, medial compartment narrowing with mild, correctible varus deformity of approximately 5° and medial joint line osteophytes (Fig. 1). Magnetic resonance imaging of the right knee confirmed that the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL) were intact. There was diffusely exposed bone over the weight-bearing medial femoral condyle and tibial plateau. The trochlear sulcus was hypoplastic with exposed bone over the central portion and chronic remodeling of the anterior inferior margin. The lateral and patello femoral compartments were without any significant osteoarthritic changes with no chondral defects or degeneration. Finally, the patellar tendon was laterally subluxed over the anterolateral trochlear margin on extension views (Fig. 2). To track knee function preoperatively and postoperatively, the patient completed the previously validated International Knee Documentation Committee (IKDC) subjective knee evaluation form. After discussing the imaging results with the patient, we reviewed potential operative management following her failed course of conservative management. The risks and benefits of quadriceps realignment versus unicondylar knee arthroplasty versus total knee arthroplasty were discussed at length with the patient. We decided to proceed with a unicondylar knee arthroplasty of the medial compartment utilizing the MAKOplasty partial knee resurfacing system. The patient had compensated for her patellar tendon subluxation for >20 years, and the decision was made to leave the patellar tendon tracking alone rather than perform a soft tissue alignment which could have limited knee flexion, causing the tendon to rub, or abrade the trochlea and lead to a new source of pain and disability. At the time of surgery, the patient was placed in a supine position and a well-padded tourniquet was placed around the proximal right thigh. The limb was prepped and draped and a time-out procedure was completed along with confirmation of Ancef (Cefazolin) administration. Two pins were then drilled in the tibia and femur for the attachment of the MAKO arrays. The limb was then exsanguinated and the tourniquet was inflated to 250mmHg. A median prepatellar approach was utilized and a 7cm incision was made along the anteromedial aspect of the knee. A minimal medial release was then completed. Retractors were placed and the appropriate data points were collected using the MAKO system array.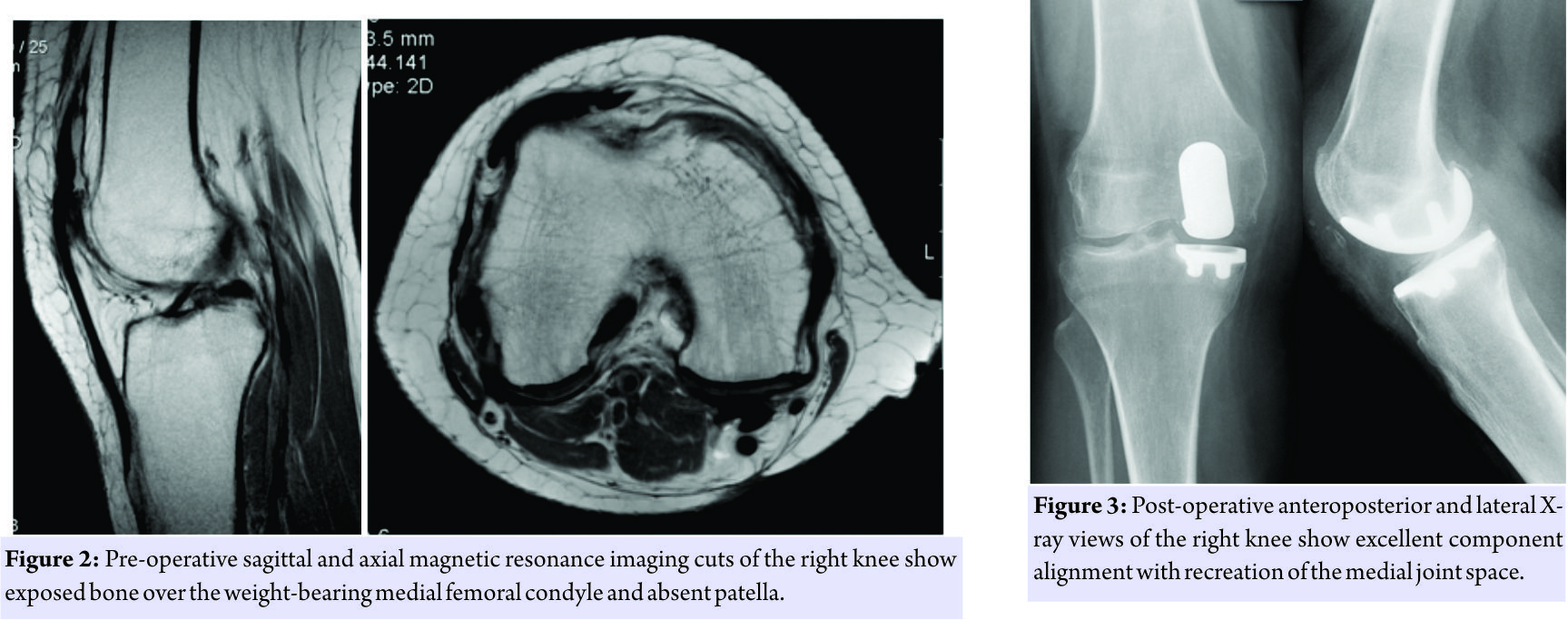 The knee was put through a full range of motion and examined for stability as well joint space opening with valgus stress. The ACL, PCL, LCL, and MCL were found to be intact without instability. The lateral and patellofemoral compartments were examined and confirmed to be without significant degeneration. At this time, it was determined appropriate to proceed with the unicondylar knee arthroplasty instead of a total knee arthroplasty. Bone resection was completed on the femur and the tibia, and then, the trial components were placed with good stability. The patella tendon continued to subluxlaterally at approximately 80° of flexion, but no correction was performed as discussed with the patient preoperatively. The trial components were removed and the bony surfaces were copiously irrigated with pulse lavage. The appropriate components (size 3 femur, size 3 tibia, and 8mm polyethylene liner) were cemented (non-antibiotic loaded) into position beginning with the femur, then the tibia, and finally, insertion of the polyethylene after removal of excess cement. The knee was held in extension while the cement was allowed to harden. The final alignment was evaluated to be in neutral alignment with appropriate varus/valgus stability. No intraoperative pain cocktail or long-acting analgesic was utilized. A single ConstaVac drain was placed. The arthrotomy was closed, with the knee in approximately 30° of flexion, w+++++++++++++++++++ith figure-of-eight 0 Vicryl sutures. The skin was closed deeply with absorbable suture followed by running Monocryl stitch and Dermabond tape. A sterile compressive dressing was placed and the patient was taken to recovery after having tolerated the procedure without complication. Following the procedure, the patient was discharged with a home physical therapy program that focused on motion and muscle strengthening on post-operative day 1. Patient received 3 doses of IV antibiotics post-operatively, and the drain was removed prior to discharge. Post-operative pain control was managed with a 2-week course of narcotics. No post-operative antibiotics or deep vein thrombosis prophylaxis were prescribed. Upon her first post-operative visit at 2 weeks, the wounds were clean and dry without any evidence of wound dehiscence or infection. At her 5-week follow-up, the patient returned to the clinic with complete resolution of her pain. On examination, she had no medial joint line tenderness and range of motion from 0 to 120°. Radiographs of the right knee showed excellent alignment of medial components with restored medial joint space. Varus deformity was corrected to 1 degree of residual varus (Fig. 3). The patient returned at3months status post right knee medial unicondylar arthroplasty with significant improvement. On examination, she had no pain and symmetric knee range of motion, 0–140° bilaterally. She continued to have patellar tendon subluxation laterally at approximately 80° of flexion, stable from pre-operative evaluation. At 6months and 1year status post-surgery, the patient filled out an online version of the IKDC Subjective Knee Evaluation Form with stepwise improvement at each time point (Table 1).
The knee was put through a full range of motion and examined for stability as well joint space opening with valgus stress. The ACL, PCL, LCL, and MCL were found to be intact without instability. The lateral and patellofemoral compartments were examined and confirmed to be without significant degeneration. At this time, it was determined appropriate to proceed with the unicondylar knee arthroplasty instead of a total knee arthroplasty. Bone resection was completed on the femur and the tibia, and then, the trial components were placed with good stability. The patella tendon continued to subluxlaterally at approximately 80° of flexion, but no correction was performed as discussed with the patient preoperatively. The trial components were removed and the bony surfaces were copiously irrigated with pulse lavage. The appropriate components (size 3 femur, size 3 tibia, and 8mm polyethylene liner) were cemented (non-antibiotic loaded) into position beginning with the femur, then the tibia, and finally, insertion of the polyethylene after removal of excess cement. The knee was held in extension while the cement was allowed to harden. The final alignment was evaluated to be in neutral alignment with appropriate varus/valgus stability. No intraoperative pain cocktail or long-acting analgesic was utilized. A single ConstaVac drain was placed. The arthrotomy was closed, with the knee in approximately 30° of flexion, w+++++++++++++++++++ith figure-of-eight 0 Vicryl sutures. The skin was closed deeply with absorbable suture followed by running Monocryl stitch and Dermabond tape. A sterile compressive dressing was placed and the patient was taken to recovery after having tolerated the procedure without complication. Following the procedure, the patient was discharged with a home physical therapy program that focused on motion and muscle strengthening on post-operative day 1. Patient received 3 doses of IV antibiotics post-operatively, and the drain was removed prior to discharge. Post-operative pain control was managed with a 2-week course of narcotics. No post-operative antibiotics or deep vein thrombosis prophylaxis were prescribed. Upon her first post-operative visit at 2 weeks, the wounds were clean and dry without any evidence of wound dehiscence or infection. At her 5-week follow-up, the patient returned to the clinic with complete resolution of her pain. On examination, she had no medial joint line tenderness and range of motion from 0 to 120°. Radiographs of the right knee showed excellent alignment of medial components with restored medial joint space. Varus deformity was corrected to 1 degree of residual varus (Fig. 3). The patient returned at3months status post right knee medial unicondylar arthroplasty with significant improvement. On examination, she had no pain and symmetric knee range of motion, 0–140° bilaterally. She continued to have patellar tendon subluxation laterally at approximately 80° of flexion, stable from pre-operative evaluation. At 6months and 1year status post-surgery, the patient filled out an online version of the IKDC Subjective Knee Evaluation Form with stepwise improvement at each time point (Table 1).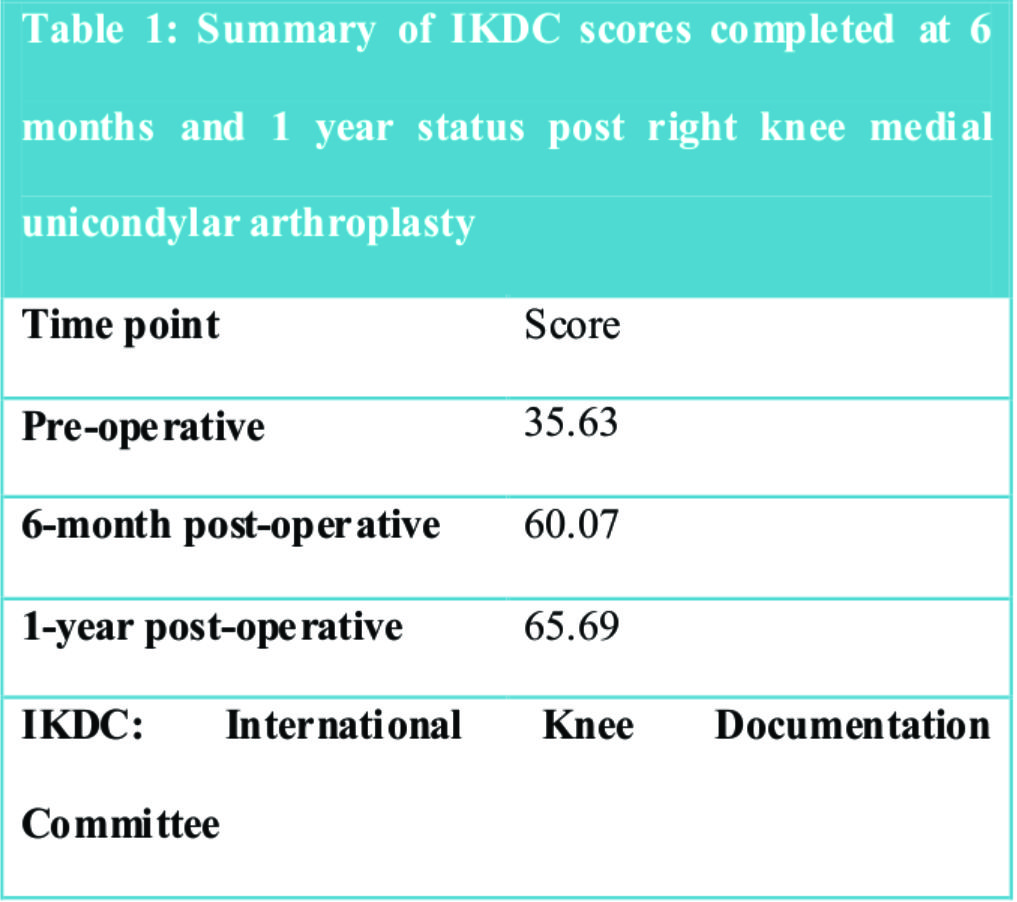
Discussion
Due to the rarity of patellectomies performed in modern orthopedic surgery, standard of care has not been established for patellectomized patients who complain of pain following a remote history of the procedure. Insall and Walker in 1976 and Marmor in 1987, both found good, long-term results in patients undergoing unicondylar arthroplasty for isolated medial compartment osteoarthritis [9, 10]. However, Capra et al., in 1992, reported that all three of their patients undergoing unicondylar arthroplasty status post-patellectomy required revision to a total knee prosthesis due to failure [11]. Pang et al., more recently in 2012, presented a case report utilizing a minimally invasive approach for a unicondylar knee arthroplasty. The patient was followed for 5 years with a good range of motion and no significant knee pain [12]. Currently, there is no data outlining the use of robot-assisted unicondylar knee arthroplasty in patellectomized patients, likely due to the limited indications for patellectomies. This case study discusses one patient’s response to a unicondylar knee arthroplasty, specifically medial compartment MAKOplasty, status post remote patellectomy. The patient’s surgical result thus far has been excellent, suggesting that robot-assisted unicondylar arthroplasties can be utilized, alongside total knee arthroplasties, as a potential surgical option for a patellectomized patient. Despite the patient’s symptoms related to her quad/patellar mal tracking, she is very satisfied with the procedure and was aware that the use of a unicondylar knee replacement was indicated for her medial pain. This case report is limited by its length of follow-up and its subsequent evaluation on the efficacy of the treatment. To fully evaluate the treatment, the patient should be followed longitudinally and additional patients should be added.
Conclusion
This case report recognizes the potentially beneficial effect of robot-assisted unicondylar arthroplasty in a patient with severe medial compartment osteoarthritis and quad/patellar tendon maltracking status post remote patellectomy at this point in her recovery.
Clinical Message
Robot-assisted unicondylar arthroplasty may be a potential treatment option in a patient with severe, isolated medial compartment osteoarthritis status post remote patellectomy.
References
1. Blatter G, Jackson RW, Bayne O, Magerl F. Patellectomy as a salvage operation. Orthopade 1987;16:310-6.
2. Insall J, Aglietti P. A five to seven-year follow-up of unicondylar arthroplasty. J Bone Joint Surg Am 1980;62:1329-37.
3. Wendt PP, Johnson RP. A study of quadriceps excursion, torque, and the effect of patellectomy on cadaver knees. J Bone Joint Surg Am 1985;67:726-7332.
4. Garr EL, Moskowitz RW, Davis W. Degenerative changes following experimental patellectomy in the rabbit. Clin Orthop Relat Res 1973;92:296-304.
5. Steurer PA Jr., Gradisar IA Jr., Hoyt WA Jr., Chu M. Patellectomy: A clinical study and biomechanical evaluation. Clin Orthop Relat Res 1979;144:84-90.
6. Kang JD, Papas SN, Rubash HE, McClain EJ Jr. Total knee arthroplasty in patellectomized patients. J Arthroplast 1993;8:489-501.
7. Martin SD, Haas SB, Insall JN. Primary total knee arthroplasty after patellectomy. J Bone Joint Surg Am 1995;77:1323-30.
8. Lakshmanan P, Wilson C. Total knee arthroplasty in a patellectomized posterior cruciate ligament deficient knee: A new technique of patellar tendon bone grafting. Knee 2004;11:481-4.
9. Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am 1976;58:754-65.
10. Marmor L. Unicompartmental knee arthroplasty following patellectomy. Clin Orthop Relat Res 1987;218:164-6.
11. Capra SW Jr., Fehring TK. Unicondylar arthroplasty. A survivorship analysis. J Arthroplast 1992;7:247-51.
12. Pang HN, Ee G, Lo NN, Yeo SJ. Minimally invasive unicondylar knee arthroplasty in a patellectomized patient. Knee Surg Sports Traumatol Arthrosc 2010;20:1831-3.
13. Citak M, Suero EM, Citak M, Dunbar NJ, Branch SH, Conditt MA, et al. Unicompartmental knee arthroplasty: Is robotic technology more accurate than conventional technique? Knee 2013;20:268-71.
14. Lang JE, Mannava S, Floyd AJ, Goddard MS, Smith BP, Mofidi A, et al. Robotic systems in orthopaedic surgery. J Bone Joint Surg Br 2001;93:1296-9.
15. Pearle AD, O’Loughlin PF, Kendoff DO. Robot-assisted unicompartmental knee arthroplasty. J Arthroplasty 2010;25:230-7.
 |
 |
 |
 |
| Dr. Shalen Kouk | Dr. Irene Kalbian | Dr. Elizabeth Wolfe | Dr. Sabrina M Strickland |
| How to Cite This Article: Kouk S, Kalbian I, Wolfe E, Strickland S. M. Robot-Assisted Medial Compartment Arthroplasty Following Remote Patellectomy: A Case Report. Journal of Orthopaedic Case Reports 2018 Jan-Feb; 8(1): 11-14. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




