[box type=”bio”] Learning Point for the Article: [/box]
The Ilizarov external ring fixator is one of useful treatment options for periprosthetic humeral shaft fractures.
Case Report | Volume 8 | Issue 4 | JOCR July – August 2018 | Page 82-85| Yohei Yanagisawa, Yuki Hara, Daisuke Nozawa, Masashi Yamazaki. DOI: 10.13107/jocr.2250-0685.1172
Authors: Yohei Yanagisawa[1], Yuki Hara[2], Daisuke Nozawa[2], Masashi Yamazaki[2]
[1]Department of Emergency and Critical Care Medicine, University of Tsukuba Hospital, 2-1-1 Amakubo, Tsukuba, Ibaraki 305-8576, Japan.
[2]Department of Orthopaedic Surgery, University of Tsukuba, 1-1-1 Tennodai, Tsukuba, Ibaraki 305-8575, Japan.
Address of Correspondence:
Dr. Yuki Hara,
1-1-1 Tennodai, Tsukuba, Ibaraki 305-8575, Japan.
E-mail: yukihara@md.tsukuba.ac.jp
Abstract
Introduction: Periprosthetic humeral shaft fracture after total elbow arthroplasty (TEA) and open reduction and internal fixation at the same side humeral neck fracture in patients with osteoporosis poses a treatment challenge. Herein, we describe our experience with its treatment using the Ilizarov external ring fixator.
Case Report: A 74-year-old Japanese woman with rheumatoid arthritis and osteoporosis sustained a periprosthetic humeral shaft fracture. The fracture was externally fixated with the Ilizarov external ring fixator, and five wires (Orthofix, Lewisville, Texas) were inserted just beside the components of the TEA (three wires were beside the humeral component and two wires the ulnar component). 4 months postoperatively, the fracture showed bone union and the fixator was removed. There were minor pin tract infections treated with oral antibiotics and transient ulnar nerve palsy with resolution after 6 months of the fixator removal. During the period of wearing the fixator, the left elbow joint was immobilized, and mainly isometric muscle exercises were performed. At 6 months of follow-up after the fixator removal, the patient was pain free, with good functional results (patient-rated elbow evaluation Japanese version 8.6 and quick- disability of the arm, shoulder, and hand Japanese version 20.5), elbow range of motion 10–130°, 80° pronation, and 80° supination. The patient returned successfully to her pre-injury occupational activities.
Conclusion: We believe that the use of the Ilizarov external fixator is a useful option for managing periprosthetic humeral shaft fractures after TEA in patients with osteoporosis.
Keywords: Total elbow arthroplasty, osteoporosis, ilizarov external ring fixator.
Introduction
Periprosthetic humeral shaft fracture after total elbow arthroplasty (TEA) in patients with osteoporosis poses a treatment challenge. The incidence of this fracture is low when compared to similar fractures after total knee and total hip arthroplasties because of those total numbers of primary arthroplasties; therefore, information about it remains limited to a few case series [1, 2]. The surgeon is faced with technical difficulties including poor screw purchase in osteoporotic bone and minimal bone space around the stem for screw fixation. Our literature search revealed no articles about this surgical treatment and periprosthetic humeral shaft fracture after TEA using the Ilizarov external ring fixator. Herein, we describe our experience with this surgical technique and report on the clinical outcome.
Case Report
A 74-year-old Japanese woman with rheumatoid arthritis and osteoporosis fell down and sustained a periprosthetic humeral shaft fracture. She underwent left primary TEA 5 years before sustaining this fracture. 1 year after the TEA, she had a left humeral surgical neck fracture caused by a fall from a standing height. Open reduction and internal fixation (ORIF) was performed with a PERI-LOC plate (Smith and Nephew, London, United Kingdom). This plate pulled out because of the osteoporotic bone 6 months after the ORIF, and repeat ORIF with a PERI-LOC plate was needed. The humeral surgical neck fracture showed union (Fig. 1). The periprosthetic humeral shaft fracture was just proximal to the tip of the stem (Mayo classification type H-Ⅲ) and just around the most distal screw of the PERI-LOC plate. This fracture was classified as simple and oblique (AO/OTA 12-A2). The humeral component of the TEA did not loosen (Fig. 2).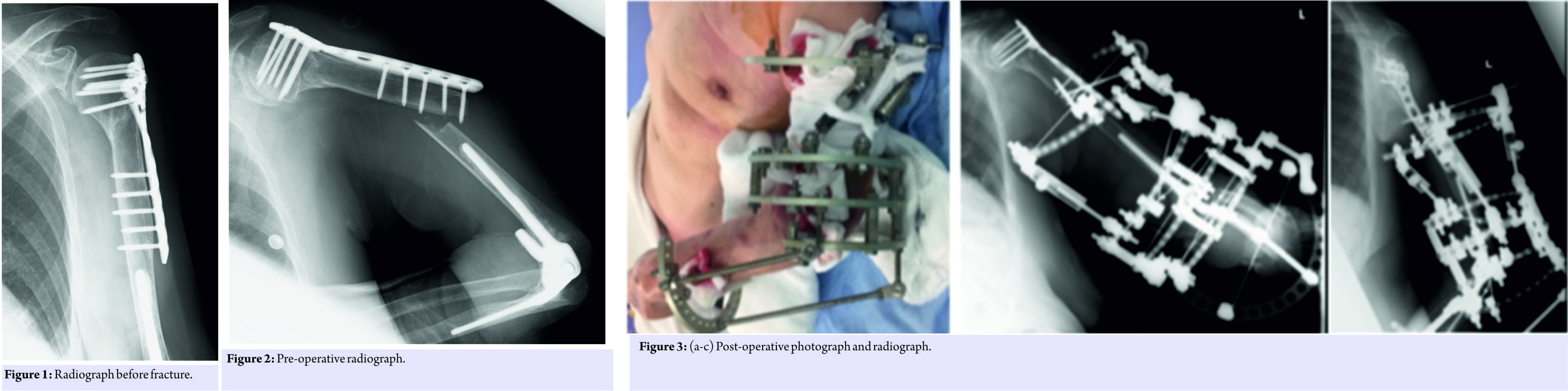 Operative treatment was indicated because acceptable reduction was not obtainable with a hanging arm cast and because the oblique fracture was at the most distal screw of the previous ORIF. The stem and the minimal distance between the stem tip and fracture line did not allow for solid bicortical screw fixation with plate. Plate fixation with a circulating wire system was an alternative but was more invasive than the external fixator. Therefore, we elected to use the Ilizarov external ring fixator for this patient. The surgery was performed in the prone position, under general anesthesia. Five TrueLok (Orthofix, Lewisville, Texas) rings were used as follows, from the proximal ring, 150 mm; 5/8 a semicircular ring, 140 mm: 5/8; 140 mm: 5/8; 140 mm: 1/2; and 140 mm: 5/8. Olive-stopped (1.8-mm) K-wires (Orthofix, Lewisville, Texas) were inserted percutaneously through the safe corridors into the humerus and ulnar olecranon, fixed after tensioning to 80 Nm, and were connected to four rings proximally. The two half pins were inserted in the proximal fragment of the humerus in a position not interfering with the plate, to protect the radial nerve, and were connected to the 150 mm: 5/8 ring. The most distal ring (140 mm: 5/8) secured the radius using one olive-stopped K-wire passing perpendicular to the shaft. The two screws at the fracture site were removed through a small incision (Fig. 3 and 4). After surgery, three additional increases in compression were applied. Weekly pin site care by the surgeon (Y.Y) was done. Superficial pin tract infections occurred once 2 months postoperatively at the most proximal half pin. It was classified as Grade 2 on the Checketts classification [3] and was treated with oral antibiotics (Cefaclor 250 mg po TID for 5 days). Transient ulnar nerve palsy occurred with resolution after 6 months of the fixator removal. The fixator was removed after 4 months when the fracture showed radiographic union and good alignment (Fig. 5). During fixator removal, three bicortical screws inserted into the distal part of the plate were also removed. At 6 months follow-up after removal, the patient had elbow range of motion 10–130°, 80 pronation, and 80 supination (Fig. 6). The patient scored 8.6 on the patient-rated elbow evaluation, Japanese version (PREE-J; where 0 is the best score and 100 is worst) [4], and 20.5 on the quick disability of the arm, shoulder, and hand score [5], where a score of 0 signifies no disability and of 100 severe disability. The patient experienced no pain and returned to her pre-injury occupational activities. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Operative treatment was indicated because acceptable reduction was not obtainable with a hanging arm cast and because the oblique fracture was at the most distal screw of the previous ORIF. The stem and the minimal distance between the stem tip and fracture line did not allow for solid bicortical screw fixation with plate. Plate fixation with a circulating wire system was an alternative but was more invasive than the external fixator. Therefore, we elected to use the Ilizarov external ring fixator for this patient. The surgery was performed in the prone position, under general anesthesia. Five TrueLok (Orthofix, Lewisville, Texas) rings were used as follows, from the proximal ring, 150 mm; 5/8 a semicircular ring, 140 mm: 5/8; 140 mm: 5/8; 140 mm: 1/2; and 140 mm: 5/8. Olive-stopped (1.8-mm) K-wires (Orthofix, Lewisville, Texas) were inserted percutaneously through the safe corridors into the humerus and ulnar olecranon, fixed after tensioning to 80 Nm, and were connected to four rings proximally. The two half pins were inserted in the proximal fragment of the humerus in a position not interfering with the plate, to protect the radial nerve, and were connected to the 150 mm: 5/8 ring. The most distal ring (140 mm: 5/8) secured the radius using one olive-stopped K-wire passing perpendicular to the shaft. The two screws at the fracture site were removed through a small incision (Fig. 3 and 4). After surgery, three additional increases in compression were applied. Weekly pin site care by the surgeon (Y.Y) was done. Superficial pin tract infections occurred once 2 months postoperatively at the most proximal half pin. It was classified as Grade 2 on the Checketts classification [3] and was treated with oral antibiotics (Cefaclor 250 mg po TID for 5 days). Transient ulnar nerve palsy occurred with resolution after 6 months of the fixator removal. The fixator was removed after 4 months when the fracture showed radiographic union and good alignment (Fig. 5). During fixator removal, three bicortical screws inserted into the distal part of the plate were also removed. At 6 months follow-up after removal, the patient had elbow range of motion 10–130°, 80 pronation, and 80 supination (Fig. 6). The patient scored 8.6 on the patient-rated elbow evaluation, Japanese version (PREE-J; where 0 is the best score and 100 is worst) [4], and 20.5 on the quick disability of the arm, shoulder, and hand score [5], where a score of 0 signifies no disability and of 100 severe disability. The patient experienced no pain and returned to her pre-injury occupational activities. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.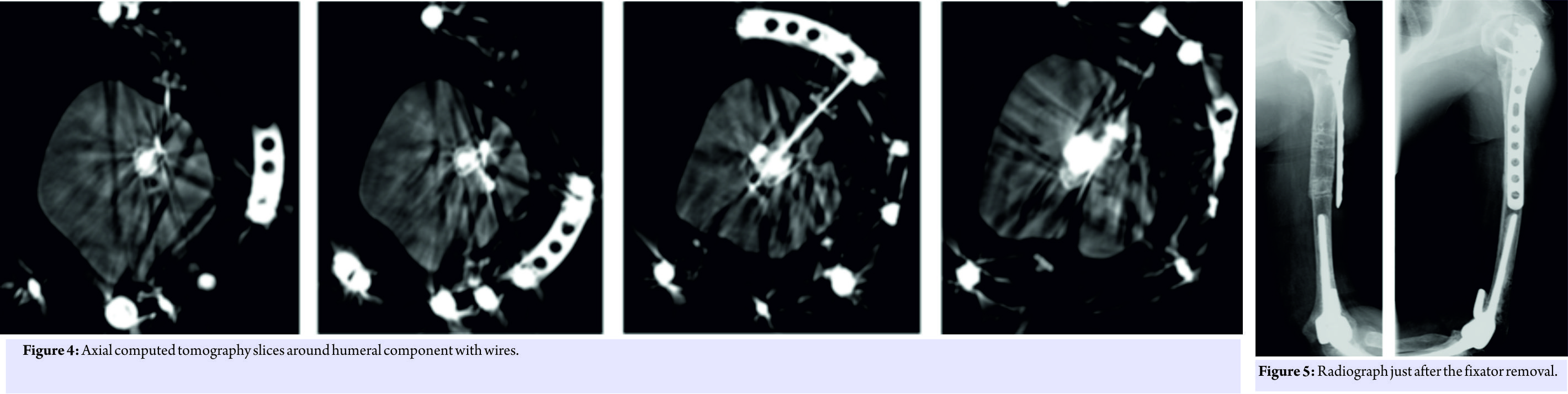
Discussion
Our case report highlights two important findings. First, the Ilizarov external ring fixator method can be one of the best surgical options for periprosthetic humeral shaft fracture after TEA in geriatrics and patients with osteoporosis after trauma. Second, although the elbow joint was fixed for 4 months with the external fixator, no contracture developed and the clinical outcome was good. The Ilizarov external ring fixator can be a surgical option for periprosthetic humeral shaft fracture after TEA. External fixation permits the repeated application of compression force to the fracture site at any time postoperatively, allowing for greater levels of compression force at the fracture site to stimulate osteogenesis [6]. This is a characteristic of external fixation and cannot be done with other surgical methods. Three additional increases in compression were applied postoperatively. One of the possible options was using plate with circular wire as a surgical method, and the other was non-operative treatment. With non-operative treatment, the probability of non-union is higher, especially in simple fracture patterns (i.e., AO/OTA type A), and was reported to range between 20 and 50% in previous reports [7, 8]. Revision arthroplasty of TEA was not an option because the stem was not loosened. Although the elbow joint was immobilized for 4 months with the external fixator, no contracture developed and an explanation was not deducible from previous studies. In our patient, the elbow joint and the surrounding muscles were not damaged at the time of fracture or the surgery, except during the passage of the φ 1.8 mm wires. Some wires were also inserted in the proximal ulna and distal radius, and the elbow joint was immobilized with bridging elbow joint fixator. However, contracture of the elbow joint did not occur. The purpose of joint immobilization was to improve the stability of the fracture by breaking the motion of the forearm. The bone quality around the humeral stem was poor, and hence, fixation with wires inserted only to the humerus was felt to be inadequate. By inserting some wires to the proximal ulna, the stability of the fracture site increased. During fixator placement, two bicortical screws inserted into the distal part of plate were removed through a minor incision because they were in the fracture site. At the time of fixator removal, another three bicortical screws were removed to prevent re-periprosthetic fracture [9]. Finally, the plate and the six screws inserted into the humeral head were not removed. The plate and screws were not removed for three reasons: a long skin incision would have been needed to achieve this, axillary nerve injury during removal would have been a risk, and because the risk of occurrence of humeral neck fracture (not periprosthetic fracture) is not expected to change with or without removal. Although we report a short-term follow-up of 6 months postoperatively, we will continue long-term follow-up and report the clinical result. The Ilizarov external ring fixator method can be a surgical option for periprosthetic humeral shaft fracture after TEA. The number of patients with osteoporosis and post-TEA is expected to increase in an aging society, and this surgical method may evolve as one of the treatment options.
Conclusion
There are few reports about surgical treatment for Mayo classification type H-ⅢA3 periprosthetic humeral shaft fracture after TEA. We believe that the use of Ilizarov external fixator is a useful option in managing periprosthetic humeral shaft fractures after TEA in patients with osteoporosis, as it can achieve anatomical bone union and good clinical outcome.
Clinical Message
The use of Ilizarov external fixator is a useful surgical method in managing periprosthetic humeral shaft fractures after TEA in patients with osteoporosis, because of less invasiveness and good clinical outcome. The orthopedic surgeons specializing in trauma should master the use of the Ilizarov external fixator method.
References
1. Hanyu T, Nakazono K, Ishikawa H. Humeral shaft fracture after a total elbow arthroplasty. J Shoulder Elbow Surg 1998;7:541-4.
2. Sanchez-Sotelo J, O’Driscoll S, Morrey BF. Periprosthetic humeral fractures after total elbow arthroplasty: Treatment with implant revision and strut allograft augumentation. J Bone Joint Surg Am 2002;84A:1642-50.
3. Nikolas NH, Fragomen AT, Rozbruch SR. Prevention of pin site infection in external fixateon: A review of the literature. Strategies Trauma Limb Reconstr 2016;11:75-85.
4. Dowrick AS, Gabbe BJ, Williamson OD, Cameron PA. Outcome instruments for the assessment of the upper extremity following trauma: A review. Injury 2005;36:468-76.
5. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand) [corrected]. The upper extremity collaborative group (UECG) Am J Ind Med 1996;29:602-8.
6. Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part Ⅰ. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res 1989;238:249-81.
7. Ekholm R, Tidermark J, Törnkvist H. Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma 2006;20:591-6.
8. Koch PP, Gross DF, Gerber C. The results of functional (Sarmiento) bracing of humeral shaft fractures. J Shoulder Elbow Surg 2002;11:143-50.
9. Walcher MG, Giesinger K, du Sart R. Plate positioning in periprosthetic or interprosthetic femur fractures with stable implants-A biomechanical study. J Arthroplasty 2016;12:2894-99.
 |
 |
 |
 |
| Dr. Yohei Yanagisawa | Dr. Yuki Hara | Dr. Daisuke Nozawa | Dr. Masashi Yamazaki |
| How to Cite This Article: Yanagisawa Y, Hara Y, Nozawa D, Yamazaki M. Treatment of Periprosthetic Humeral Shaft Fracture after Total Elbow Arthroplasty in an Osteoporotic Patient, using the Ilizarov External Ring Fixator: A Case Report. Journal of Orthopaedic Case Reports 2018 Jul-Aug; 8(4): 82-85. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




