[box type=”bio”] Learning Point of the Article: [/box]
Autologous osteochondral transplantation in focal patellar chondral lesions without patellofemoral malalignment showed excellent results. In cases of large off-centered lesions, however, it took longer for pain relief.
Case Report | Volume 9 | Issue 1 | JOCR January – February 2019 | Page 53-57 | Yasukazu Yonetani, Yoshinari Tanaka, Takashi Kanamoto, Norimasa Nakamura, Ken Nakata, Shuji Horibe. DOI: 10.13107/jocr.2250-0685.1306
Authors: Yasukazu Yonetani[1], Yoshinari Tanaka[2], Takashi Kanamoto[3], Norimasa Nakamura[3], Ken Nakata[3], Shuji Horibe[4]
[1]Department of Orthopedic Sports Medicine, Hoshigaoka Koseinenkin Hospital, 4-8-1 Hoshigaoka, Hirakata, Osaka 573-8511, Japan,
[2]Department of Sports Orthopaedics, Osaka Rosai Hospital, 1179-3 Nagasone-cho, Kita-ku, Sakai, Osaka 591-8025, Japan,
[3]Department of Orthopaedics, Osaka University Graduate School of Medicine, 2-2 Ymadaoka, Suita, Osaka, Japan,
[4]Graduate School of Comprehensive Rehabilitaion, Osaka Prefecture University, Habikino, Osaka, Japan.
Address of Correspondence:
Dr. Yasukazu Yonetani,
Department of Orthopedic Sports Medicine, Hoshigaoka Koseinenkin Hospital, 4-8-1 Hoshigaoka, Hirakata, Osaka 573-8511, Japan.
E-mail: yonechan-osk@umin.ac.jp
Abstract
Introduction: Autologous osteochondral transplantation (AOT) in the focal cartilage lesion of the patella has been reported with less successful results compared with other sites. The purposes were to investigate the clinical outcomes of AOT for focal patellar chondral lesion without patellofemoral instability.
Methods: Between 2001 and 2007, six patients (five males and one female) with a focal patellar cartilage lesion without patellofemoral malalignment and instability were treated with AOT. The mean age was 38 (27–51) years. Intraoperatively, the size and location of lesion were assessed by international cartilage repair society classification. Lysholm score was investigated preoperatively, at 6 months, 1- and 2-year, and final follow-up. Mean follow-up period was 51 months (24–101). Transplanted grafts were evaluated by magnetic resonance imaging (MRI) and second-look arthroscopy.
Results: The mean size was 133mm2 (78–225). All six cases improved at final follow-up (Lysholm score 79–100). Although immediate pain relief obtained in four cases, severe pain was persistent in remaining two cases during the 1styear and gradually relieved by 2 years following surgery. The size of these two cases was significantly larger (over 170 mm2) than that of four cases (100 mm2 in average) (P<0.05), and their locations were apart from center of the patella inspite of four cases localized centrally (P<0.05). Repaired cartilage did not show any difference by MRI and arthroscopically.
Conclusion: AOT in focal patellar chondral lesions without patellofemoral malalignment showed excellent results. In cases of large off-centeredlesions, however, it took longer for pain relief following AOT.
Keywords: Focal patella cartilage lesion, Autologous osteochondral transplantation, Normal patellofemoral alignment.
Introduction
Patella chondral lesions may cause pain, swelling, clicking, and instability and thus potentially impair daily activities. However, in daily clinical situation, these cartilage injuries are diagnosed accidentally on magnetic resonance imaging (MRI) or arthroscopic operation without symptoms[1]. Patella chondral lesions are sometimes observed in the patients with patellofemoral malalignment including recurrent patella dislocation. Focal patellar chondral lesions have historically been treated with various surgical procedures, but reliable and consistent symptomatic relief has not been obtained[2]. However, the emergence of cartilage repair has provided potential treatment options including microfracture [3, 4], autologous chondrocyte implantation [4, 5], and autologous osteochondral (OC) transplantation (AOT) [5, 6, 7, 8]. With press-fit implantation of cylindrical OC complex, AOT could be an attractive option for full-thickness chondral lesions, but there were limited information on the clinical outcome of AOT in patella lesions. Previous studies indicated that AOT to patella has inferior clinical outcome as compared with AOT to femoral condyles [9]. However, these studies included the patients with or without patellofemoral malalignment and did not investigate the clinical results in consideration of patellofemoral instability. The report on AOT for patellar chondral lesions suggested that the patients with patella malalignment may represent a subset of patients who have a poor prognostic outcome compared to patients with normal alignment [10]. On the other hand, the clinical results in patients with normal patellofemoral alignment and stability have almost not been elucidated. The purposes of this study were to evaluate the clinical outcomes of the patients treated by AOT for the repair of isolated symptomatic full-thickness cartilage lesions of the patella without malalignment and instability.
Patients
Between 2001 and 2007, six patients with focal patellar cartilage lesion with normal patellofemoral alignment after failure of conservative treatment for >6 months were included in this study. There were five males and one female with a mean age of 38 ± 8.8 ranging from 27 to 51 years.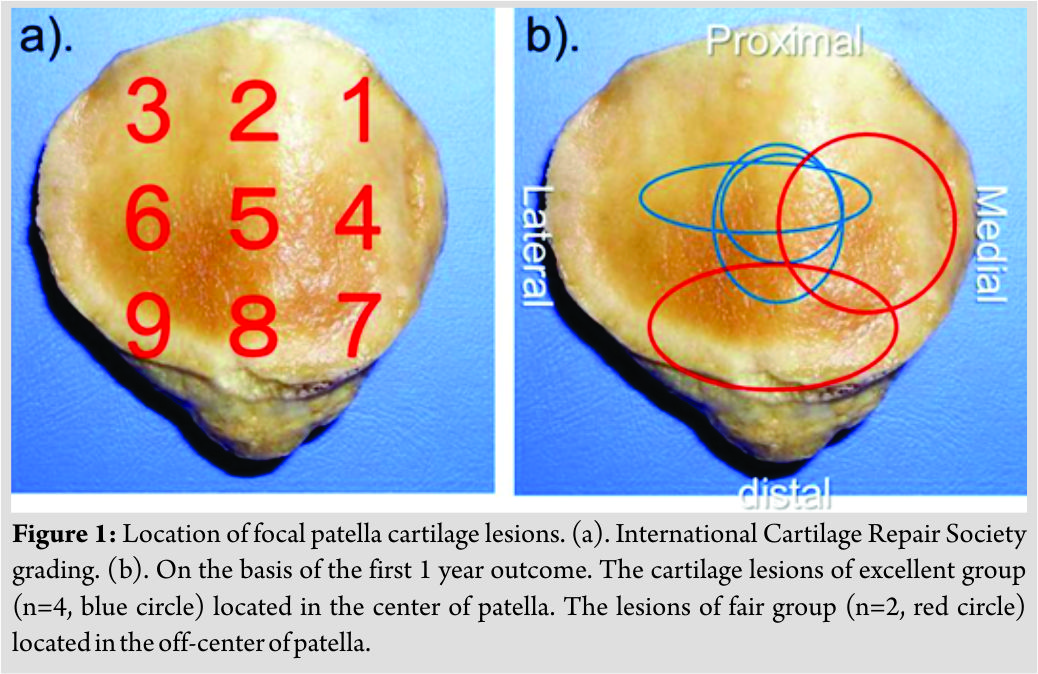
Operative Procedure
After arthroscopic evaluation, the patella was exposed through medial arthrotomy. The articular cartilage surfaces were examined to characterize the location, size, and international cartilage repair society (ICRS) grading. Autologous OC grafts obtained from lateral and medial femoral trochlea were transplanted to patellar cartilage lesion, using “soft delivery system” (Zimmer Germany GmbH, Freiburg, Germany). After harvesting the osteochondral plugs, the donor sites were filled with hydroxyapatite blocks (interconnected porous calcium HA) (Neo-bone®, MMT, Japan).
The most commonly used size of OC plug was 7.45 mm in diameter, with the mean size 7.0 mm (standard deviation [SD] 0.6, range 5.5–7.45mm). The mean number of plugs was 3.3 (SD 1.6, range 2–6). The number of plug transplanted was one plug in one patient, three plugs in three patients, four plugs in one patient, and six plugs in one patient.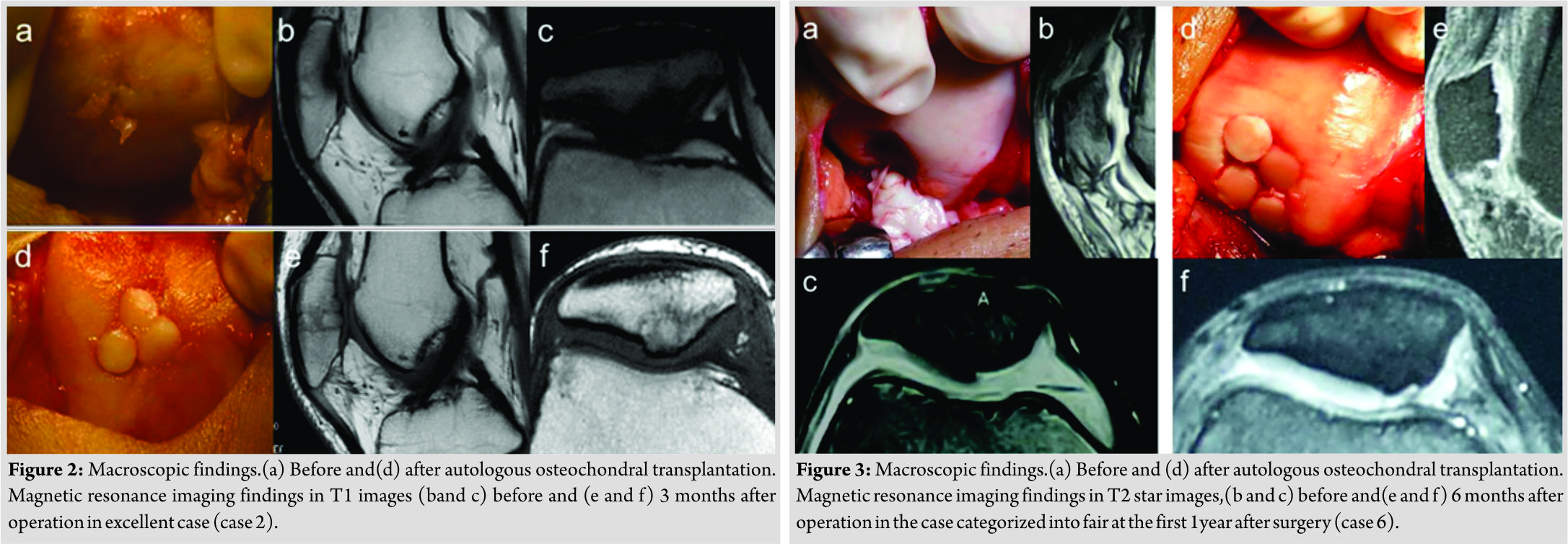
Post-operative Rehabilitation
The knee joint was immobilized at 30°for 3 weeks postoperatively. Full weight-bearing was permitted at 5 weeks. The patients were allowed to be back tostrenuous activities at 6 months. All patients were followed at least 2 years and the average duration of follow-up was 51 months (SD 28, range 24–101months).
Evaluation
The Lysholm score was obtained at preoperatively, 6 months, 1 year, 2 years, and final follow-up point after operation. The patients with over 90 points were graded as excellent, between 84 and 90 points as good, 65–83 as fair, and <65 as poor, respectively. Intraoperative evaluation such as size, location, and degree of cartilage injury was done using ICRS grading. Specifically, the location of the patellar cartilage lesion was evaluated by ICRS grading, which divided nine areas in patellar surface (Fig. 1a). MRI evaluation was performed postoperatively. The congruity of the articular surface and the fissure between surrounding normal structure and transplanted OC plug were examined at final follow-up, using previously described MRI criteria of cartilage repair [10]. Parameters reviewed included signal intensity of the repaired area relative to the surrounding cartilage (hypointense, isointense, or hyperintense), morphologic appearance (depressed, flush, or proud), subchondral edema (none, mild, moderate, or severe), bony overgrowth (absence or presence), interface with adjacent cartilage (absence, presence, and size of fissure), and percentage of fill based on both coronal and sagittal images (0%–33%, 34%–66%, or 67%–100%). Based on informed consent, a second-look arthroscopy was performed in four cases for the evaluation of repair tissue and synovitis. Statistical analysis to compare outcome scores before and after surgery was performed using two related samples comparison with non-parametric Wilcoxon signed-rank test. The size and number of areas which chondral lesion occupied in patella were analyzed to compare between the clinical groups using independent t-test (Statmate III, ATMS, Tokyo, Japan). P <0.05 was considered to be statistically significant.
Results
The mean pre-operative Lysholm score of the patients was 67 (SD 8.8, range 54–80) and improved to 90 (SD13, range 79–100) at final follow-up. However, at the first 1 year after operation, two cases (fair group, cases 5 and 6) had fair Lysholm score (73, 83) in contrast with excellent scores (mean 96, SD 4.8) in the other four cases (excellent group, cases1–4) (Table1 and Fig. 2). The two patients in fair group had severe anterior knee pain after post-operative immobilization, which led arthrofibrosis needed the manipulation within 5 weeks after operation. Although range of knee motion had improved after manipulation, severe anterior knee pain at squatting and stepping continued during the first 1 year after operation. Hereafter, anterior knee pain reduced with time in both cases, and the Lysholm score at final follow-up improved to 79–90 points, respectively(Fig. 3 and Table1). The mean size of the lesion was 133 mm2 (SD 56, range 78–225). The mean size in the fair group was 200 mm2 (SD 36, range 174–225), significant larger than the excellent group with 87mm2 (SD 42, range78–128) (P=0.03). The average number of grafts increased in proportion to the size; five grafts (SD1.4, range 4–6) in fair group and 2.5 grafts (SD1.0, range 1–3) in excellent group(P=0.06) (Table2). The mean number of area occupied by OC lesion in fair group was 3.5 (SD 0.5, range 3–4), significant larger than excellent group with 1.3 (SD 0.25, range 1–2) (P=0.01). On the basis of location, excellent group located atcenter of patella, while fair group positioned widely apart from the center area (Fig. 1b and Table 2). MRI at 6 months after operation revealed that the subchondral bone defect was completely healed and was covered by articular cartilaginous tissue. In all six patients, there was 67–100% filling of the defect by repair tissue being flush with the surrounding cartilage. There was no fissure detected within the lesion. The subchondral bone of the implanted plug showed proud with surrounding subchondral bone in three patients, flush in two patients, and depressed in one patient. The signal intensity of the cartilaginous part of the implanted plugs was observed as similar to surrounding cartilage in five patients and lower in one patient. There was no subchondral edema in three patients and mild in three patients. In the two cases with severe pain during 2 years after operation (cases 5 and 6), there was no significant difference about MRI appearance against remaining four cases with immediate pain relief after surgery(Table1). A second-look arthroscopy (n=4) revealed no instability of OC plug and smoothness of reconstructed articular surface. In one of the two fair cases, debridement of the synovial tissue around the recipient site in spite of good stability and smooth articular surface.
Discussion
AOT in six focal patellar chondral lesions with normal patellofemoral alignment showed excellent results over 2 years after operation. In two cases of large off central lesions, it took >2 years until pain relief was confirmed, although four cases of small central lesions achieved immediate pain relief. To the best of our knowledge, this is the first study which indicated that the location and size of damaged site in patella might affect the clinical results of early phase. The previous clinical studies about AOT showed the inferior results with focal chondral patellar lesions rather than femoral condylar lesions [8]. The several causes were suggested that the differences of articular cartilage thickness between trochlea and patella affected the difficulties of adaptation for mechanical environment of patellofemoral joint[9]. The “step-off” between cartilage thickness of donor plug from trochlea and recipient patella cartilage was indicated the cause of mechanical differences affecting the clinical results. All our six patients showed not only good MRI appearance but also reliable the second-look arthroscopic findings about repaired site. These results indicated that accurate structural reconstruction of patella cartilage and subchondral bone is essential for final clinical outcome over 2 years in patellar lesion with normal alignment. However, post-operative complication occurred in two cases; manipulation was needed due to arthrofibrosis and taking long time for resolving the residual severe pain after surgery. The range and location of chondral lesion in these two fair cases was wide and off central in the patella, in opposition to small center lesions in the other four excellent cases. These findings might be caused by the mechanical strength of the patella depending on the location due to inhomogeneous volume of the cancellous bone and mineral density of subchondral bone plate [11,12]. This clinical tendency and biomechanical situation indicated that not only small size but also central part of patella might be easy to be reconstructed by OC plugs, meanwhile, off central part of patella might be difficult to be reconstructed due to structural and biomechanical complexity of patella. Furthermore, the recipient bone volume in patella except harvested bone plugs was quite less in the large off central lesion than central small lesion. In addition to difficulties about reconstruction of morphologic structure of patella, the larger biomechanical defect caused by AOT in large off central chondral lesion might lead prolonged pain relief after operation because not only patella itself but also multiple transplanted OC plugs had more instability and mechanical stress during squatting motion rather than small central lesion. Thus, in spite of acceptable MRI appearance, two cases took so long time to resolve the squat pain until transplanted OC plugs remodeled to be suitable biomechanical OC structure in patella. There are a number of limitations of the present study. The study was designed to be a retrospective review of data collected prospectively in a registry after cartilage repair procedures. We acknowledge that MRI data are incomplete due to the retrospective nature of the study and, therefore, prone to selection bias. Although a prospective follow-up of the same patients at identical, standardized time intervals would have been ideal, a prospective study for an uncommonly performed procedure would have been impractical and would require a lengthy study period to accumulate an adequate cohort.
Conclusion
Patellar AOT is an effective treatment for focal patellar chondral lesions with significant improvement in clinical follow-up. The both of osseous and cartilage component of the OC plug appears to heal predictably in all case, but patients with large off central lesion may represent a subset of patients who have an immediate poorer outlook compared with patients with small central lesion.
Clinical Message
AOT for focal patellarchondral lesion had been reported not only unsuccessful results but also no affecting factors for clinical outcomes. This article shows that AOT in focal patellar chondral lesions without patellofemoral malalignment showed excellent results. In cases of large off-centered lesions, however, it took longer for pain relief following AOT.
References
1. Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG, et al. Cartilage injuries: A review of 31,516 knee arthroscopies. Arthroscopy 1997;13:456-60.
2. Mouzopoulos G, Borbon C, Siebold R. Patellar chondral defects: A review of a challenging entity. Knee Surg Sports Traumatol Arthrosc 2011;19:1990-2001.
3. Steadman JR, Rodkey WG, Briggs KK. Microfracture to treat full-thickness chondral defects: Surgical technique, rehabilitation, and outcomes. J Knee Surg 2002;15:170-6.
4. Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG, et al. Outcomes of microfracture for traumatic chondral defects of the knee: Average 11-year follow-up. Arthroscopy 2003;19:477-84.
5. Knutsen G, Drogset JO, Engebretsen L, Grøntvedt T, Isaksen V, Ludvigsen TC, et al. A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am 2007;89:2105-12.
6. Matsusue Y, Yamamuro T, Hama H. Arthroscopic multiple osteochondral transplantation to the chondral defect in the knee associated with anterior cruciate ligament disruption. Arthroscopy 1993;9:318-21.
7. Laprell H, Petersen W. Autologous osteochondral transplantation using the diamond bone-cutting system (DBCS): 6-12 years’ follow-up of 35 patients with osteochondral defects at the knee joint. Arch Orthop Trauma Surg 2001;121:248-53.
8. Hangody L, Füles P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: Ten years of experimental and clinical experience. J Bone Joint Surg Am 2003;85-A Suppl 2:25-32.
9. Bentley G, Biant LC, Carrington RW, Akmal M, Goldberg A, Williams AM, et al. A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg Br 2003;85:223-30.
10. Nho SJ, Foo LF, Green DM, Shindle MK, Warren RF, Wickiewicz TL, et al. Magnetic resonance imaging and clinical evaluation of patellar resurfacing with press-fit osteochondral autograft plugs. Am J Sports Med 2008;36:1101-9.
11. Eckstein F, Müller-Gerbl M, Putz R. Distribution of subchondral bone density and cartilage thickness in the human patella. J Anat 1992;180 ( Pt 3):425-33.
12. Hoechel S, Wirz D, Müller-Gerbl M. Density and strength distribution in the human subchondral bone plate of the patella. Int Orthop 2012;36:1827-34.
 |
 |
 |
 |
 |
 |
| Dr. Yasukazu Yonetani | Dr. Yoshinari Tanaka | Dr. Takashi Kanamoto | Dr. Norimasa Nakamura | Dr. Ken Nakata | Dr. Shuji Horibe |
| How to Cite This Article: Yonetani Y, Tanaka Y, Kanamoto T, Nakamura N, Nakata K, Horibe S. Autologous Osteochondral Transplantation in Full-thickness Patella Chondral Lesion: A Case Series. Journal of Orthopaedic Case Reports 2019 Jan-Feb; 9(1): 53-57. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




