[box type=”bio”] Learning Point of the Article: [/box]
Midline sacral fractures are rare and complex injuries that may require anterior and posterior pelvic fixation to address residual pelvic instability.
Case Report | Volume 9 | Issue 2 | JOCR March – April 2019 | Page 64-68 | Nicholas O’Neill, Michael VanWagner, Christopher Vitale. DOI: 10.13107/jocr.2250-0685.1374
Authors: Nicholas O’Neill[1], Michael VanWagner[1], Christopher Vitale[1]
[1]Department of Orthopedic Surgery, McLaren Macomb Regional Medical Center, Graduate Medical Education, Michigan State University, 1000 Harrington St. Mount Clemens, MI, Michigan, USA.
Address of Correspondence:
Dr. Nicholas O’Neill,
Department of Orthopedic Surgery, McLaren Macomb Regional Medical Center, Graduate Medical Education, Michigan State University, 1000 Harrington St. Mount Clemens, MI, Michigan, USA.
E-mail: nickoneill309@gmail.com
Abstract
Introduction: Anterior-posterior compression pelvic injuries occur from high-energy blunt trauma and can result in devastating outcomes. Often, widening of the pubic symphysis occurs with subsequent disruption of posterior pelvic ligamentous structures. Associated sacral fractures may increase the likelihood of neurologic injury and pelvic ring instability. The most common sacral fracture in this injury is an avulsion fracture of the sacral ala. Midline longitudinal sacral fractures into the spinal canal are an extremely rare variant of sacral injuries in conjunction with pelvic trauma. In contrast to traditional anterior-posterior pelvic ring injuries, those associated with this unique fracture type carry a decreased risk of neurologic injury. Only a small number of these cases exist in English literature. Given its rarity, further, investigation of the fracture mechanism and treatment protocol is warranted.
Case Report: A 67-year-old Caucasian male presented with an anterior-posterior compression pelvic ring injury after he was struck by an oncoming vehicle on his motorcycle. Radiographs revealed pubic symphyseal widening of 4.7 cm. A pelvic binder was placed as a temporary measure to minimize intrapelvic hemorrhage. Advanced imaging revealed a complete, midline sagittal sacral fracture through the posterior sacral elements. During his hospital admission, the patient required multiple procedures for sustained upper extremity fractures and subsequently underwent surgical fixation of his anterior and posterior pelvic ring injuries 2 days after admission. Our patient to date has achieved sacral fracture union, minimal residual pubic diastasis, and has no evidence of neurologic injury. He has some persistent impotence and is ambulating without assistance. Despite his significant injuries, his outcome to date has been quite impressive.
Conclusion: It is critical to always examine the posterior pelvis and sacrum when examining anterior-posterior compression injuries. While most cases have reported fixation of only the anterior pelvis, we explain the need for additional posterior pelvic fixation to address the inherent instability of these unique sacral fractures and ultimately decrease patient morbidity. The surgical fixation technique of this patient’s pelvic injuries is described, as well as his post-operative course and outcome to date.
Keywords: Neurologic deficit, Pelvic ring injury, Percutaneous fixation, Sacral fracture.
Introduction
Midline longitudinal sacral fractures are an extremely rare variant of sacral injuries in anterior-posterior pelvic ring trauma [1]. Denis et al. classified sacral fractures based on the involvement of the sacral ala (Zone I), neural foramina (Zone II), or the spinal canal (Zone III) and reported increasing rates of neurologic deficits with more central injuries [2]. However, midline sacral fractures in the sagittal plane, an uncommon subtype of central Zone III fractures, result from different pathomechanics and are less likely to result in neurologic injury [3]. Only a small number of these cases have been reported in the literature (Table 1), and a standard treatment protocol has yet to be established. We present a complete, midline longitudinal sacral fracture in the setting of an anterior-posterior pelvic ring injury and review the paucity of literature on this fracture pattern.
Case Report
A 67-year-old man presented after being struck by a vehicle while riding his motorcycle with complaints of pain in his neck, pelvis, and left upper extremity. There was no loss of consciousness. Urinary function could not be assessed at initial presentation due to the presence of a Foley catheter, but there was no blood at the urethral meatus. Medical history was significant only for hypertension. On examination, he was conscious, oriented, and hypotensive (103/55 mm Hg). There was hypogastric tenderness and exposed bone through an open wound near his left elbow. Neurovascular status was preserved in both the upper and lower extremities. There was no damage to the spinal cord elements. Anteroposterior pelvic radiograph revealed pubic diastasis of 4.7 cm and a midline fracture through the sacral body with 1.0 cm of displacement (Fig. 1a). 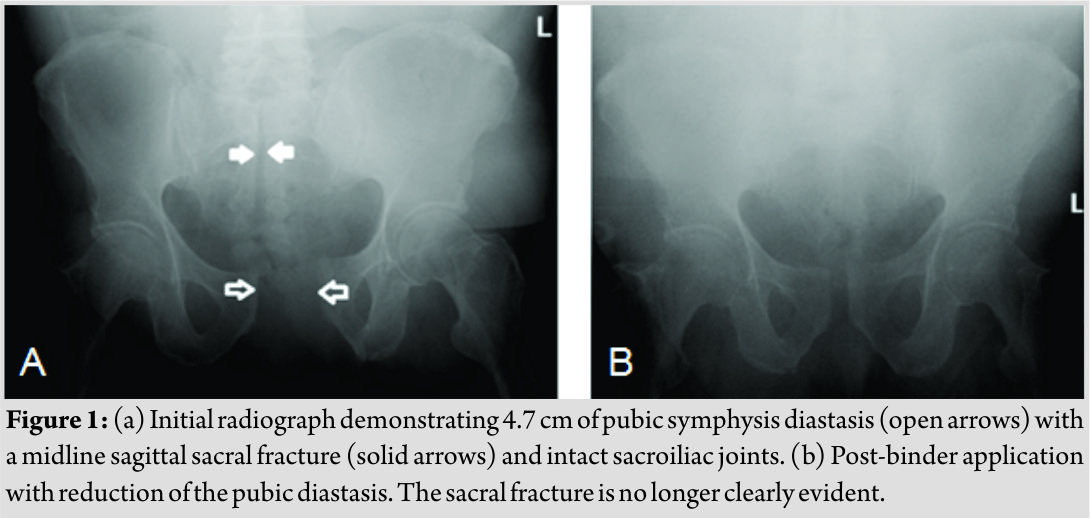 A pelvic binder was placed to decrease intrapelvic hemorrhage and repeat plain films demonstrated acceptable closure of his pelvic diastasis (Fig. 1b). After binder application and the placement of two large-bore intravenous cannulas administering crystalloid isotonic solution, hemodynamic stability was achieved and the patient was deemed stable a contrast-enhanced computed tomography CT scan revealed hemoperitoneum, 1.3 cm of pubic diastasis, and a complete, midline sacral fracture through the spinal canal and posterior sacral elements extending from S1 to the coccyx (Fig. 2). To rule out urologic injury, a CT cystogram was obtained, which revealed no evidence of bladder or urethral rupture. An urgent irrigation and debridement with surgical fixation of his left open ulnar shaft fracture were performed. Great care was taken to monitor the patient’s skin condition beneath the binder to assure he did not experience any areas of skin necrosis or compromise. 2 days after hospital admission, he underwent open reduction internal fixation of the pubic diastasis using a pelvic reduction clamp and a 6-hole non-locking symphyseal plate by Pfannenstiel approach (Fig. 3).
A pelvic binder was placed to decrease intrapelvic hemorrhage and repeat plain films demonstrated acceptable closure of his pelvic diastasis (Fig. 1b). After binder application and the placement of two large-bore intravenous cannulas administering crystalloid isotonic solution, hemodynamic stability was achieved and the patient was deemed stable a contrast-enhanced computed tomography CT scan revealed hemoperitoneum, 1.3 cm of pubic diastasis, and a complete, midline sacral fracture through the spinal canal and posterior sacral elements extending from S1 to the coccyx (Fig. 2). To rule out urologic injury, a CT cystogram was obtained, which revealed no evidence of bladder or urethral rupture. An urgent irrigation and debridement with surgical fixation of his left open ulnar shaft fracture were performed. Great care was taken to monitor the patient’s skin condition beneath the binder to assure he did not experience any areas of skin necrosis or compromise. 2 days after hospital admission, he underwent open reduction internal fixation of the pubic diastasis using a pelvic reduction clamp and a 6-hole non-locking symphyseal plate by Pfannenstiel approach (Fig. 3). 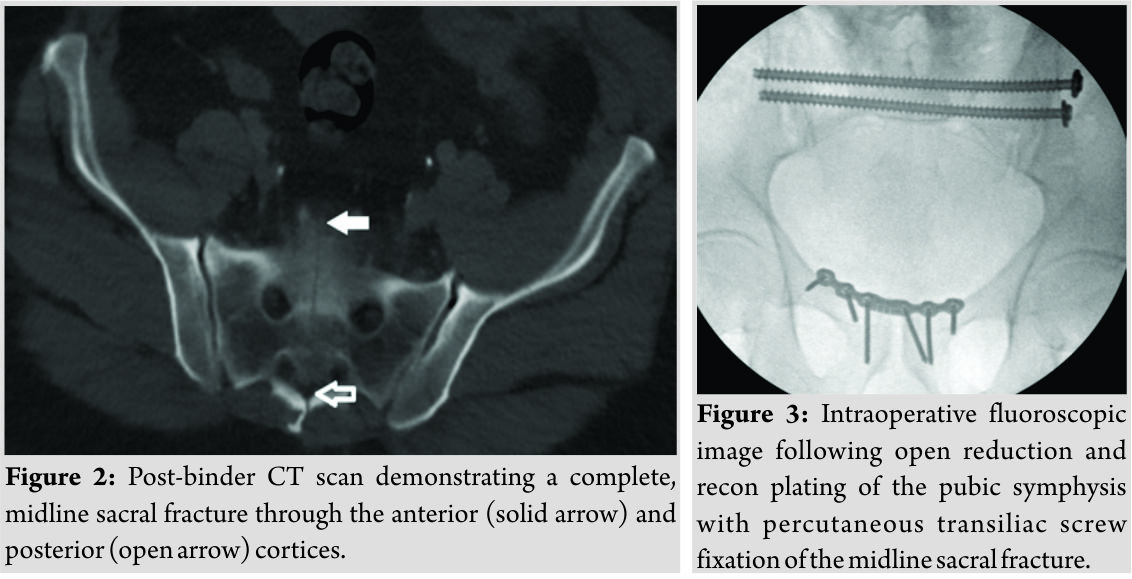 During reduction and fixation of the anterior pelvis, intraoperative fluoroscopic assessment revealed increased widening of the midline longitudinal sacral fracture. Due to the fracture’s involvement of the posterior sacral elements and subsequent axial plane instability, fixation of the sacral fracture was deemed necessary to prevent further displacement and potential symptomatic deformity. Under fluoroscopic guidance, transsacral-transiliac guide pins were then used to insert 7.3mm fully threaded screws into the S1 and S2 body, measuring 150 mm and 140 mm, respectively. The screws were inserted posterior to the iliaccortical density so as not to injure the L5 nerve root. Using lag-screw fixation technique principles, these screws closed down the midline sacral fracture diastasis and anatomic reduction was achieved. Postoperatively, the patient was mobilized to weight bear for transfers. At 10 weeks, he began weight-bearing as tolerated. The patient developed post-operative urinary retention and a Foleycatheter remained in place on hospital discharge. The urology team followed him as an outpatient and the catheter was removed at 1 month, at which time he was able to pass urine normally. The patient received routine follow-up evaluations. Sacral fracture union was evident at 5 months with only mild loss of reduction at the pubic symphysis (1.3 cm of diastasis) (Fig. 4). He had persistent impotence with otherwise normal urologic function and no neurologic deficits.
During reduction and fixation of the anterior pelvis, intraoperative fluoroscopic assessment revealed increased widening of the midline longitudinal sacral fracture. Due to the fracture’s involvement of the posterior sacral elements and subsequent axial plane instability, fixation of the sacral fracture was deemed necessary to prevent further displacement and potential symptomatic deformity. Under fluoroscopic guidance, transsacral-transiliac guide pins were then used to insert 7.3mm fully threaded screws into the S1 and S2 body, measuring 150 mm and 140 mm, respectively. The screws were inserted posterior to the iliaccortical density so as not to injure the L5 nerve root. Using lag-screw fixation technique principles, these screws closed down the midline sacral fracture diastasis and anatomic reduction was achieved. Postoperatively, the patient was mobilized to weight bear for transfers. At 10 weeks, he began weight-bearing as tolerated. The patient developed post-operative urinary retention and a Foleycatheter remained in place on hospital discharge. The urology team followed him as an outpatient and the catheter was removed at 1 month, at which time he was able to pass urine normally. The patient received routine follow-up evaluations. Sacral fracture union was evident at 5 months with only mild loss of reduction at the pubic symphysis (1.3 cm of diastasis) (Fig. 4). He had persistent impotence with otherwise normal urologic function and no neurologic deficits.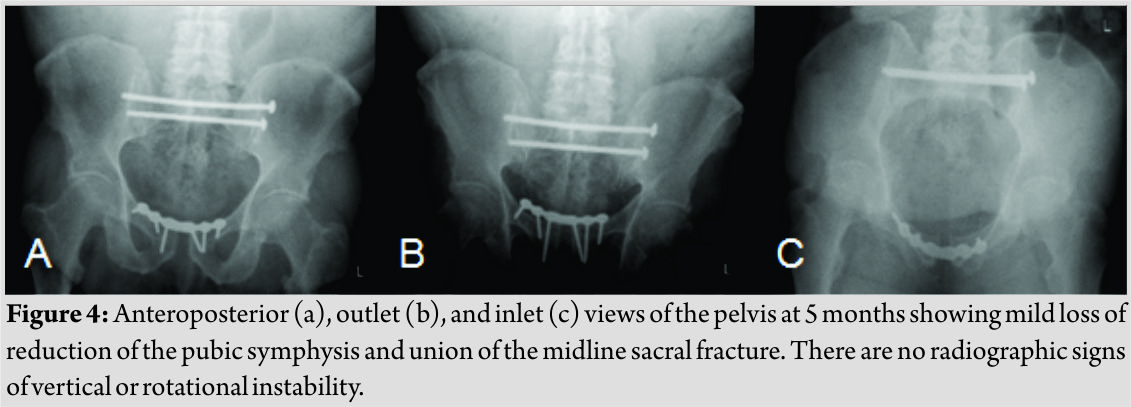
Discussion
Midline longitudinal sacral fractures are incredibly rare injuries. Although the incidence of sacral fractures in pelvic ring injuries can be anywhere from 10% to 45%, most are compression or avulsion fractures of the sacral ala or foramina [1]. These result from lateral compression and anterior-posterior compression forces, respectively. According to the widely used classification established by Denis et al., sacral fractures that involve structures medial to the sacral foramina (Zone III) are typically transverse in nature. These fractures carry a much higher risk of neurologic injury than those occurring through the foramina (Zone II) or sacral ala (Zone I) [2]. While longitudinal sacral fractures may occur in Zone I and Zone II, only a small number of cases document complete midline longitudinal fractures through the central canal, a rare variant of Zone III injuries (Table 1). Anterior-posterior forces causing traumatic pubic symphysis diastasis must also cause disruption of another location in the pelvic ring [4]. As the pubic symphysis widens, each hemipelvis externally rotates, which leads to the disruption of posterior pelvic structures [1]. Although posterior disruption is most often seen as ligamentous failure at the anterior portion of the sacroiliac joints, fractures of the sacrum and ilium may occur. It is uncommon for the posterior pelvis to fail through a fracture of the midline sacral body. There may be association with preexisting sacral abnormalities that predispose patients to this injury [5, 6, 7]. Carter et al. and Ebraheim et al. suggest that a low-lying dural sac and spina bifida occulta are abnormalities that may serve as sacral stress risers, making the midline sacral body prone to traumatic fracture. Our patient had no known underlying sacral deformity. Although these injuries have been reported to occur from a posterior to anterior mechanism [7], such as a fall from height directly onto the posterior sacrum, we do not believe this was the mechanism in our case. It was reported that the vehicle collided with our patient head-on likely causing an anterior blunt force that caused the pelvis to fail in an anterior to posterior direction. He also did not have any abrasions or signs of direct trauma near the posterior pelvis or sacrum on physical examination. Although the complete fracture mechanism is not fully understood, it has been well documented that Zone III midline longitudinal sacral fractures have a significantly decreased risk of neurologic injury when compared to the more common Zone III fracture patterns. Denis et al. reported a 56.7% incidence of neurologic injury in Zone III fractures, the majority of which were transverse. Transverse fractures are often markedly displaced and may involve all three sacral zones, leading to bilateral damage of nearby sacral nerve roots and potential bowel, bladder, and sexual dysfunction [7]. In contrast, midline longitudinal fractures result in lateral displacement of both sacral fragments, which likely protect the relatively mobile nerve roots from the traction and compression injury that is observed in displaced transverse fractures [1]. With the nerve roots pushed to each side of the midline fracture, it is possible that a relatively normal anatomic relationship is maintained within the pelvis, perhaps protecting against further tethering as they exit the neuroforamina and greater sciatic notches [8]. The persistent impotence seen in our patient is likely a consequence of the severe soft tissue trauma he sustained during the event and cannot be attributed to sacral root or plexus injury. Although impotence in certain patients may also be related to the surgical approach to the anterior pelvis, we do not believe that to be the case with our patient. The blunt force patients experience in anterior-posterior compression injuries may lead to thrombosis of perineal arteries, causing impotence and sexual dysfunction [3]. A protocol outlining the evaluation and treatment of these unique fractures has yet to be established. During the primary survey, appropriate measures should be taken to first stabilize the pelvis with a sheet or binder if associated pubic symphysis diastasis is present, as was encountered in this case. A thorough physical examination is necessary to identify the presence or absence of an acute neurologic injury. Thin-slice CT imaging is required to fully understand the sacral injury and fracture characteristics, as the incidence of initially missed sacral fractures may approach 60%–70% with standard radiographs alone [6]. In our case, the sacral fracture was evident on primary radiographs; however, CT imaging provided the necessary detail for appropriate surgical planning. Surgical treatment of sacral fractures, in general, is dependent on the associated pelvic ring disruption [9]. Bellabarba et al. reported a series of 10patients with longitudinal midline sacral fractures in the setting of anterior-posterior compression injuries, nine of which required surgical treatment. A unique characteristic of this series was that the posterior sacral elements remained intact in all patients, evidenced by wide displacement of the anterior sacral body and minimal displacement posteriorly. These injuries were amenable to open reduction internal fixation of the pubic diastasis alone secondary to an intact posterior hinge. Our patient’s fracture characteristics differed from the above series in that the posterior sacral elements were no longer intact. Intraoperative fluoroscopic evaluation revealed unstable gapping, both anteriorly and posteriorly, of the sacral fracture following reduction of the pubic symphysis diastasis. Although the fracture was not vertically unstable, the rotational instability demonstrated by the intraoperative displacement warranted fixation with transiliac screws. Ebraheim et al. reported a similar case in which percutaneous pelvic fixation was necessary to address the fracture displacement that had occurred in the axial plane [7].
Conclusion
This case demonstrates a rare variant of the anterior-posterior pelvic injury, with complete posterior pelvic disruption by means of a midline longitudinal sacral fracture. The initial assessment and treatment of these patients should follow advanced trauma life support. During the course of any necessary resuscitation and provisional pelvic ring closure, it is imperative to examine and document any neurologic dysfunction. Classically, Zone III sacral fractures are associated with a high risk of neurologic injury. However, consistent with our patient’s case, midline longitudinal variants in Zone III appear to have a lower incidence of neurologic injury. These fractures require thin-slice CT scans for a thorough multiplanar understanding of the involved structures. It is well accepted that significant anterior pubic diastasis should be addressed with operative fixation. However, the midline longitudinal sacral fracture pattern has been reported as both stable and unstable following anterior fixation. We recommend anterior pelvic fixation first, with subsequent intraoperative fluoroscopic evaluation to document any increased or residual displacement that may suggest instability of these unique sacral fractures. If the anterior sacral body alone appears wide, but an intact posterior hinge provides adequate stability, posterior fixation may not be necessary. However, if the posterior midline sacral fracture further gaps following acceptable anterior pelvic reduction and fixation, this is evidence that the sacrum is unstable and requires posterior fixation. Although treatment varies on a case by case basis, appropriate identification and treatment of these rare sacral fractures arenecessary to prevent complex deformities and progressive loss of neurologic function [10].
Clinical Message
A thorough evaluation is required in the management of traumatic pelvic injuries including immediate interventions and appropriate imaging studies. Although they are associated with decreased rates of neurologic injury, midline longitudinal sacral fractures represent a complex challenge to orthopedic surgeons. In addition to anterior pelvic stabilization, posterior pelvic fixation may be necessary in the event of residual pelvic instability.
References
1. Bellabarba C, Stewart J, Ricci W, DiPasquale T, Bolhofner B. Midline sagittal sacral fractures in anterior-posterior compression pelvic ring injuries. J Orthop Trauma 2003;17:32-7.
2. Denis F, Davis S, Comfort T. Sacral fractures: An important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res 1988;227:67-81.
3. Vijayan S, Basani V, Naik M, Rao SK, Kumar S. Longitudinal midline sacral split fracture – a rare entity. BMJ Case Rep 2017. DOI:10.1136/bcr-2017-220397.
4. Moed BR, Morawa LG. Displaced midline longitudinal fracture of the sacrum. J Trauma 1984;24:435-7.
5. Ebraheim NA, Savolaine ER, Skie MC, Baril J. Longitudinal fracture of the sacrum: Case report. J Trauma1994;36:447-50.
6. Carter TR, Lambert K. Pubic diastasis with longitudinal fracture of the sacral body: Case report. J Trauma 1990;30:627-9.
7. Ebraheim NA, Biyani A, Salpietro B. Zone III fractures of the sacrum. A case report. Spine 1996;21:2390-6.
8. Wiesel SW, Zeide MS, Terry RL. Longitudinal fractures of the sacrum: Case report. J Trauma 1979;19:70-1.
9. Ruatti S, Kerschbaumer G, Gay E, Milaire M, Merloz P, Tonetti J. Technique for reduction and percutaneous fixation of U- and H-shaped sacral fractures. Orthop Traumatol Surg Res 2013;99:625-29.
10. Vaccaro AR, Kim DH, Brodke DS, Harris M, Chapman J, Schildhauer T, Routt C, Sasso RC. Diagnosis and management of sacral spine fractures. Instructional course lectures, AAOS. J Bone Joint Surg 2004;86:166-75.
 |
 |
 |
| Dr. Nicholas O’Neill | Dr. Michael VanWagner | Dr. Christopher Vitale |
| How to Cite This Article: O’Neill N, VanWagner M, Vitale C. Midline Longitudinal Sacral Fracture in an Anterior-Posterior Compression Pelvic Injury – A Surgical Decision-making and Outcome. Journal of Orthopaedic Case Reports 2019 Mar-Apr; 9(2): 64-68. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




