[box type=”bio”] Learning Point of the Article: [/box]
The diagnosis of Mazabraud’s syndrome requires a strong clinical suspicion in patients presenting with recurrent myxomas and it should not be confused with soft tissue sarcoma.
Case Report | Volume 9 | Issue 3 | JOCR May-June 2019 | Page 26-29 | Divesh Jalan, Princi Jain. DOI: 10.13107/jocr.2250-0685.1404
Authors: Divesh Jalan[1], Princi Jain[2]
[1]Central Institute of Orthopaedics, Vardhmaan Mahavir Medical College and Safdarjang Hospital, New Delhi, India, [2]Department of Medicine, PGIMER and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
Address of Correspondence:
Dr. Divesh Jalan,
Central Institute of Orthopaedics, Vardhmaan Mahavir Medical College and Safdarjang Hospital, New Delhi, India.
E-mail: dvsh_jalan@yahoo.com
Abstract
Introduction: Mazabraud’s syndrome is a rare benign disorder characterized by the association of single or multiple intramuscular myxomas with monostotic or polyostotic form of fibrous dysplasia. Around 80 cases have been described till date; however, a higher incidence may be expected due to silent nature of the disease and missed diagnosis. The authors report one such case of a missed diagnosis.
Case Report: A 39-year-old lady presented with recurrent soft tissue myxomas in thigh. A thorough evaluation with radiographs and magnetic resonance imaging (MRI) and a clinical suspicion of this rare entity helped in making the diagnosis of Mazabraud’s syndrome. The patient was treated with wide excision of the recurrent thigh swelling and watchful observation of two other asymptomatic swelling detected on MRI examination. Bisphosphonate therapy was given for fibrous dysplasia. At latest follow-up after 2 years, the patient was asymptomatic with no recurrence.
Conclusion: The report highlights the importance of a high degree of suspicion of this clinical entity in patients treated for recurrent soft tissue swelling as both myxomas and fibrous dysplasia behave differently than their isolated counterparts.
Keywords: fibrous dysplasia, myxoma, Mazabraud’s syndrome, monostotic, polyostotic.
Introduction
Mazabraud’s syndrome is a rare benign disorder characterized by the association of single or multiple intramuscular myxomas with monostotic or polyostotic form of fibrous dysplasia [1-6]. In nearly all the cases, myxomas and fibrous dysplasia tend to be localized in the same anatomical region [4-6]. The first case of intramuscular myxomas in association with fibrous dysplasia was described by Henschen in 1926 [7], but the clear association between the two was established by Mazabraud in 1967 [8]. Although around 80 cases have been described till date, due to the clinically silent nature of the disease and missed diagnosis, a higher incidence can be expected [1]. We present a case of Mazabraud’s syndrome in a 39-year-old female with recurrent soft tissue swelling in the thigh and undiagnosed fibrous dysplasia.
Case Report
A 39-year-old female presented to the outpatient clinic with the complaints of recurrent painless swelling in the left thigh and had a history of surgery twice for its removal. She was apparently well until 2001 when she noticed a painless swelling over left mid-thigh. The swelling progressively increased in size and she underwent surgical excision in 2005. She remained asymptomatic for the next 2 years when she again noticed a new swelling over the left distal thigh which was excised surgically in 2009. She remained asymptomatic for the next 3 years when she had a recurrent swelling over the left distal thigh. The swelling was progressively increasing in size and was associated with some discomfort. At the time of presentation to us, she had a large, oval, around 8 cm × 4 cm size, painless swelling over the medial aspect of the left distal thigh. There was a healed scar over the left medial thigh with quadriceps wasting. The swelling was intramuscular on clinical examination. Systemic examination was unremarkable. She was further evaluated with radiographs of the thigh which was suggestive of fibrous dysplasia. This led us to go for a thorough skeletal survey, which showed the involvement of the left femur and tibia (Fig. 1). She was also evaluated with magnetic resonance imaging (MRI) of whole of the thigh which showed two additional soft tissue masses; one in left mid-thigh and the other in the left inguinal region (Fig. 2). As the previous biopsy report was suggestive of myxoma, clinical diagnosis of Mazabraud’s syndrome was made. The patient decided for operative management of the large distal thigh symptomatic swelling and conservative management for the remaining two small, asymptomatic swelling. After informed consent, she underwent wide excision of the distal thigh swelling through the previous skin incision. The mass was intramuscular, located within vastus medialis. A single, globular, pale white, encapsulated nodular mass measuring 8 cm × 4 cm × 3 cm was excised (Fig. 3).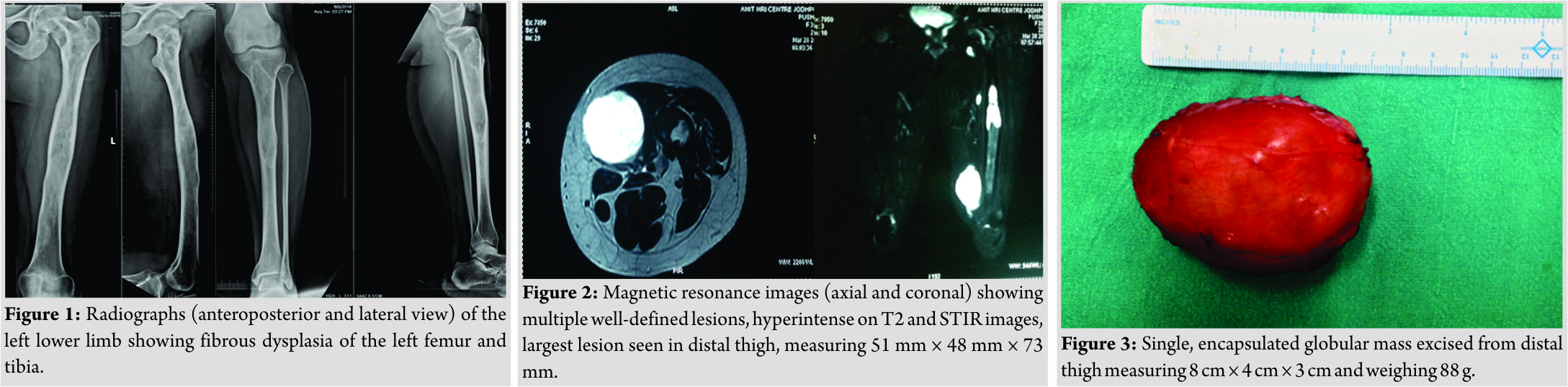 The mass weighed around 88 g. Histopathological examination was suggestive of intramuscular myxoma (Fig. 4). No necrotic areas or atypical mitotic figures were identified, ruling out any malignancy. The patient was managed with weekly oral bisphosphonates for fibrous dysplasia, which was stopped after 1.5 years. A regular MRI every 6 months was advised to assess the recurrence and interval enlargement of the remaining two lesions. On follow-up, MRI was done 6 months postoperatively, and these two masses seemed to have slightly increased in size; however, the patient remained asymptomatic (Fig. 5). At latest follow-up after 2 years, the patient was pain free with no recurrence and the MRI showed decrease in the size of the mid-thigh lesion and minimal increase in the size of the left inguinal lesion (Fig. 6).
The mass weighed around 88 g. Histopathological examination was suggestive of intramuscular myxoma (Fig. 4). No necrotic areas or atypical mitotic figures were identified, ruling out any malignancy. The patient was managed with weekly oral bisphosphonates for fibrous dysplasia, which was stopped after 1.5 years. A regular MRI every 6 months was advised to assess the recurrence and interval enlargement of the remaining two lesions. On follow-up, MRI was done 6 months postoperatively, and these two masses seemed to have slightly increased in size; however, the patient remained asymptomatic (Fig. 5). At latest follow-up after 2 years, the patient was pain free with no recurrence and the MRI showed decrease in the size of the mid-thigh lesion and minimal increase in the size of the left inguinal lesion (Fig. 6).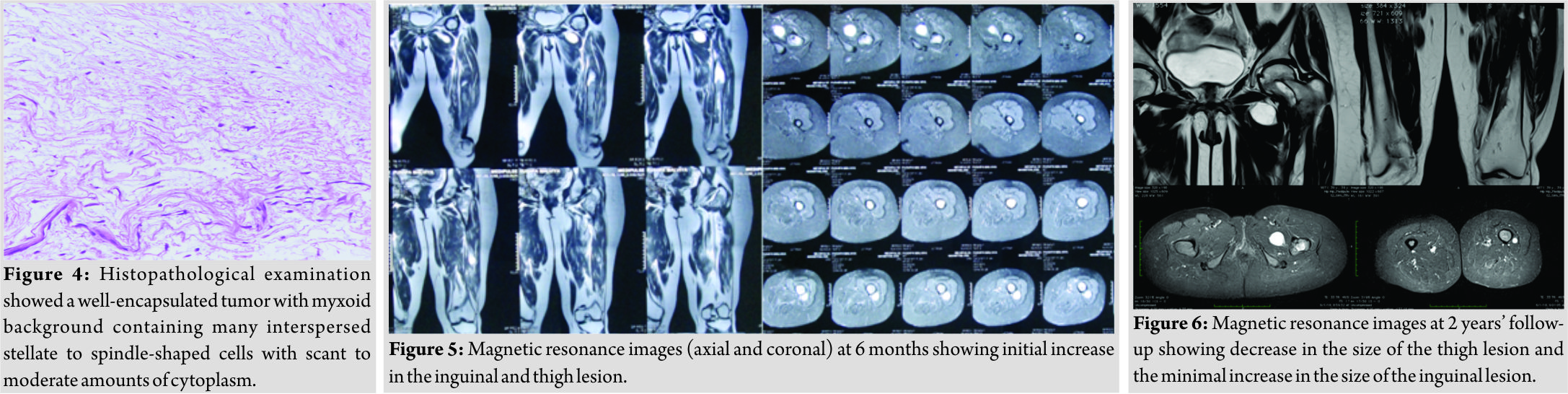
Discussion
Mazabraud’s syndrome is a rare phenomenon of the association of two relatively common benign lesions. However, these individual lesions behave differently to some extent from their isolated counterparts. Myxomas in Mazabraud’s syndrome are exclusively intramuscular [4]. Fibrous dysplasia in Mazabraud’s syndrome presents at a later age in adulthood, in contrast to isolated fibrous dysplasia which presents in childhood [4]. Moreover, fibrous dysplasia in Mazabraud’s syndrome follows a more indolent course and shows a greater potential for malignant transformation into osteosarcoma [1-6]. The disease is seen most commonly in middle-aged females and the most common sites for myxomas are the thigh, buttocks, arm, and chest wall [9]. The exact etiology of the disease is unknown. Various theories suggested include inborn error of tissue metabolism [10], abnormal bone and tendon development [11], or reactive response of soft tissue to fibrous dysplasia [12]. Molecular genetic analysis has shown point mutation in codon 211 of GNAS-1 gene encoding a signal transduction protein regulating cAMP levels in intramuscular myxomas. Similar mutations have been detected in McCune-Albright syndrome as well as in sporadic intramuscular myxomas [1-3, 6]. Fibrous dysplasia usually precedes the myxoma lesions in Mazabraud’s syndrome [5, 6] unlike our case where fibrous dysplasia may be present before but was not detected in the beginning. This may be attributed to the initial surgeon not suspecting it and predominantly managing it as a soft tissue swelling. Myxomas generally arise near the affected bones, commonly in the lower limb, as in our case. However, there is no evidence of continuity between the two. The occurrence of the two lesions in the same anatomical compartment may be attributed to mutations in GNAS-1 gene [1-3, 6]. The identification of the syndrome requires MRI of the soft tissue lesion, confirmation of myxoma by needle biopsy, and skeletal survey to look for any bony lesions. In our case, the disease was being managed for recurrent myxomas suspected to be a sarcoma in view of multiple recurrences. The diagnosis was missed as this clinical entity was not suspected and skeletal survey was not done. One study has described the role of 18FDG-PET/CT in Mazabraud’s syndrome, although owing to rather indolent course of disease and its relatively localized distribution, this modality has not gained much popularity [2]. The main differentials for myxomas in histopathology include benign lesions such as myxolipoma, myxoid neurofibroma, and myxochondroma as well as malignant lesions such as myxoid liposarcoma, myxoid malignant fibrous histiocytoma, low-grade fibromyxoid sarcoma, extraskeletal myxoid chondrosarcoma, and botryoid type rhabdomyosarcoma [2]. A prior knowledge of association with fibrous dysplasia can overcome a significant diagnostic dilemma. The treatment options for Mazabraud’s syndrome include wide excision of myxomas in case of development of pain or pressure symptoms. Local recurrence of incompletely excised myxomas has been reported as has been in our case. This warrants a regular follow-up for local recurrence as well as the development of new lesions. Fibrous dysplasia is generally managed with bisphosphonate therapy, and surgical intervention is rarely needed [1-6]. The presence of myxomas warrants a more vigorous monitoring of fibrous dysplasia lesions for the risk of malignant transformation [1-6].
Conclusion
The incidence of Mazabraud’s syndrome may be higher than reported due to its silent course and missed diagnosis. The risk of malignant transformation of fibrous dysplasia, local recurrence of myxomas after excision, and possibility of new swelling necessitate regular follow-up of known cases. The treatment consists of wide excision of symptomatic myxomas, whereas bisphosphonates are the mainstay for the management of fibrous dysplasia. The case should not be confused with soft tissue sarcomas as the presence of an associated fibrous dysplasia can be suggestive of benign nature of the soft tissue lesion.
Clinical Message
The diagnosis of Mazabraud’s syndrome requires a strong clinical suspicion in patients presenting with recurrent myxomas. It should not be confused with soft tissue sarcoma as the presence of associated fibrous dysplasia suggests benign nature of the lesion. In addition, these group of patients need close monitoring due to the higher chances of recurrence and possible risk of malignant transformation of fibrous dysplasia of bone.
References
1. Wamba JD, Bermudez MJ, Dominguez TL, Pascua LR. Polyostotic fibrous dysplasia associated with intramuscular myxomas: Mazabraud syndrome. Ind J Radiol Imaging 2015;25:280-3.
2. Munksgaard PS, Salkus G, Iyer VV, Fisker RV. Mazabraud’s syndrome: Case report and literature review. Acta Radiol Short Rep 2013;2:2047981613492532.
3. Gaumetou E, Tomeno B, Anract P. Mazabraud’s syndrome: A case with multiple myxomas. Orthop Traumatol Surg Res 2012;98:455-60.
4. John AM, Behera KK, Mathai T, Parmar H, Paul TV. Mazabraud syndrome. Ind J Endocrinol Metab 2013;17:740-2.
5. Kabukcuoglu F, Kabukcuoglu Y, Yilmaz B, Erdem Y, Evren I. Mazabraud’s syndrome: Intramuscular myxoma associated with fibrous dysplasia. Pathol Oncol Res 2004;10:121-3.
6. Kabukcuoglu F, Kabukcuoglu Y. Mazabraud’s syndrome: Intramuscular Myxoma associated with Fibrous Dysplasia. Orphanet Encyclopedia; 2005. Available from: https://www.orpha.net/data/patho/GB/uk-Mazabraud.pdf. Last accessed on 10/11/2018.
7. Henschen F. Fall von Ostitis Fibrosa mit multiplen tumoren in der umgebenden muskulatur. Verh Dtsh Ges Pathol 1926;21:93-7.
8. Mazabraud A, Semat P, Roze R. A propos de lassociation de fibromyxomes des tissus mous a ladysplasie fibrreuse des os. Presse Med 1967;75:2223-8.
9. Cabral C, Guedes P, Fonseca T, Yue HE. Polyostotic fibrous dysplasia associated with intramuscular myxoma: Mazabraud’s syndrome. Skeletal Radiol 1998;27:278-82.
10. Gianoutos M, Thompson J, Marsden F. Mazabraud’s syndrome: Intramuscular myxoma associated with fibrous dysplasia of bone. Aust N Z J Surg 1990;60:825-8.
11. Mazabraud A, Cirard J. Un cas particulier de dysplasie fibreuse a localisations osseuses et tendineuses. Rev Rheum Mal Osteoartic 1957;34:652-9.
12. Wirth WA, Leavitt D, Enzinger FM. Multiple intramuscular myxomas. Another extraskeletal manifestation of fibrous dysplasia. Cancer 1971;27:1167-73.
 |
 |
| Dr. Divesh Jalan | Dr. Princi Jain |
| How to Cite This Article: Jalan D, Jain P. Mazabraud’s Syndrome – A Diagnosis Commonly Missed. Journal of Orthopaedic Case Reports 2019 May-June; 9(3): 26-29. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




