[box type=”bio”] Learning Point of the Article: [/box]
Not all pathological fractures due to simple bone cyst be managed conservatively, some fractures require surgery for better functional outcome.
Case Report | Volume 9 | Issue 3 | JOCR May-June 2019 | Page 49-51 | Hariharan Mohan, Balgovind S Raja. DOI: 10.13107/jocr.2250-0685.1416
Authors: Hariharan Mohan[1], Balgovind S Raja[1]
[1]Department of Orthopedics, Seth GS Medical College and KEM Hospital, Parel, Mumbai, Maharashtra, India.
Address of Correspondence:
Dr. Hariharan Mohan,
Department of Orthopedics, Seth GS Medical College and KEM Hospital, Parel, Mumbai – 400012, Maharashtra, India.
E-mail: hariharan274@gmail.com
Abstract
Introduction: Simple bone cyst (SBC) is the most common cause of pathological fracture in children. The most common sites are proximal humerus and proximal femur. There is no specific protocol in the management of pathological fractures with SBC. Treatment options include intralesional injection of steroids and bone marrow aspirate, percutaneous or open curettage of the lesion with or without bone grafting.
Case Report: We report a case of pathological fracture of distal humerus due to SBC in a 16-year-old male. The fracture was treated surgically. Open reduction was done; curettage of cyst wall followed by non-vascularized fibula strut grafting was done and fixed with bicolumnar plating. Early post-operativemobilization was started. The patient had good outcome with incorporation of graft and healing of fracture and lesion.
Conclusion: Unstable pathological fractures due to SBC require osteosynthesis and curettage of lesion with bone grafting. Stable fractures can be managed conservatively.
Keywords: Simple bone cyst, pathological fracture, humerus, bone grafting.
Introduction
The simple bone cyst (SBC) (unicameral bone cyst) is the most common benign lytic bone lesion in childhood. 80% of these lesions are found in the second decade of life with a male predominance (3:1). SBC is usually solitary developing in the metaphysis of long bones. 80% of the cases are seen in proximal humerus and proximal femur. Other rare sites include proximal or diaphyseal tibia, diaphyseal humerus, distal femur, fibula, radius, ulna, and calcaneum. SBC consists of a solitary cavity lined by a membrane of variable thickness and filled with a clear yellow fluid. The lesion appears to be reactive or developmental rather than to represent a true neoplasm. There is no risk of malignant transformation. Radiographically, SBC appears as a centrally located, well-circumscribed, radiolucent lesion with sclerotic margins. With growth of the bone, the lesion migrates toward the diaphysis and usually ends up filled and ossified. The symptoms include pain, swelling, or stiffness of the joints. A pathological fracture is often the first sign of the lesion. Fracture is the most common complication. Spontaneous resolution following fracture is seen in 15% of cases [1]. Clinical factors such as pain, young age, or superior humeral location and radiologic factors such as cavity enlargement overtime, cavity distance from growth plate, and multicameral aspect are signs of cyst activity and fracture risk. Growth disorder may be induced by the cyst crossing the growth plate and extending toward the epiphysis. We hereby present a rare case of SBC of distal humerus complicated by pathological fracture in a 16-year-old male that was treated with curettage, autologous fibula strut grafting, and internal fixation. SBC of distal humerus is a rare occurrence and there are no similar case reports in literature.
Case Report
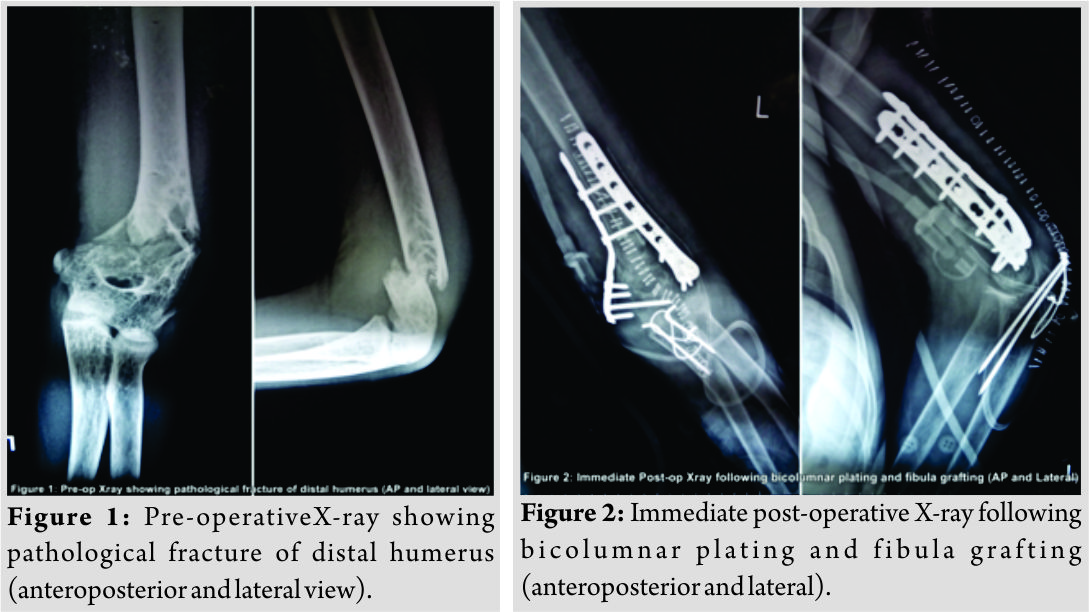
A 16-year-old student was brought to the emergency with a history of trivial fall following which he developed pain and swelling in his left distal arm. X-rays showed a fracture of distal humerus with a lytic lesion involving the distal third of the humerus (Fig.1).Hematological and biochemical investigations were normal. The arm was initially stabilized in a U slab and the patient was taken for fixation in routine OT. Under general anesthesia, the patient was placed in lateral position. Posterior midline incision was taken from distal third of humerus to proximal ulna. Ulnar nerve isolated and olecranon osteotomy was performed to expose the fracture site in distal humerus. A cavity filled with homogenous grayish-white nodular membrane was found. Entire cavity was curetted and the tissue removed was sent for histopathological examination. Fracture margins were freshened. Fibular graft was harvested from the ipsilateral lower limb. The cavity was filled with fibular strut graft. Fixation of the fracture was done with bicolumnar plating (lateral column – posterior and medial column – medial). K-wire tension band wiring was done for olecranon osteotomy (Fig. 2).
Wound closed in layers. The limb was immobilized in above elbow slab. Post-operative period was uneventful. Suture removal was done after 2 weeks. Passive-assisted elbow range of motion was started at 2 weeks as per pain tolerance. Active range of motion was started after 4 weeks. Histopathology report confirmed the diagnosis of SBC. The patient had good functional range of motion at 4 months (10–130) (Fig. 3). There was no donor site morbidity. Follow-up radiographs after 8 months showed full integration of fibular graft (Fig. 4 and 5).
There was no donor site morbidity. Follow-up radiographs after 8 months showed full integration of fibular graft (Fig. 4 and 5).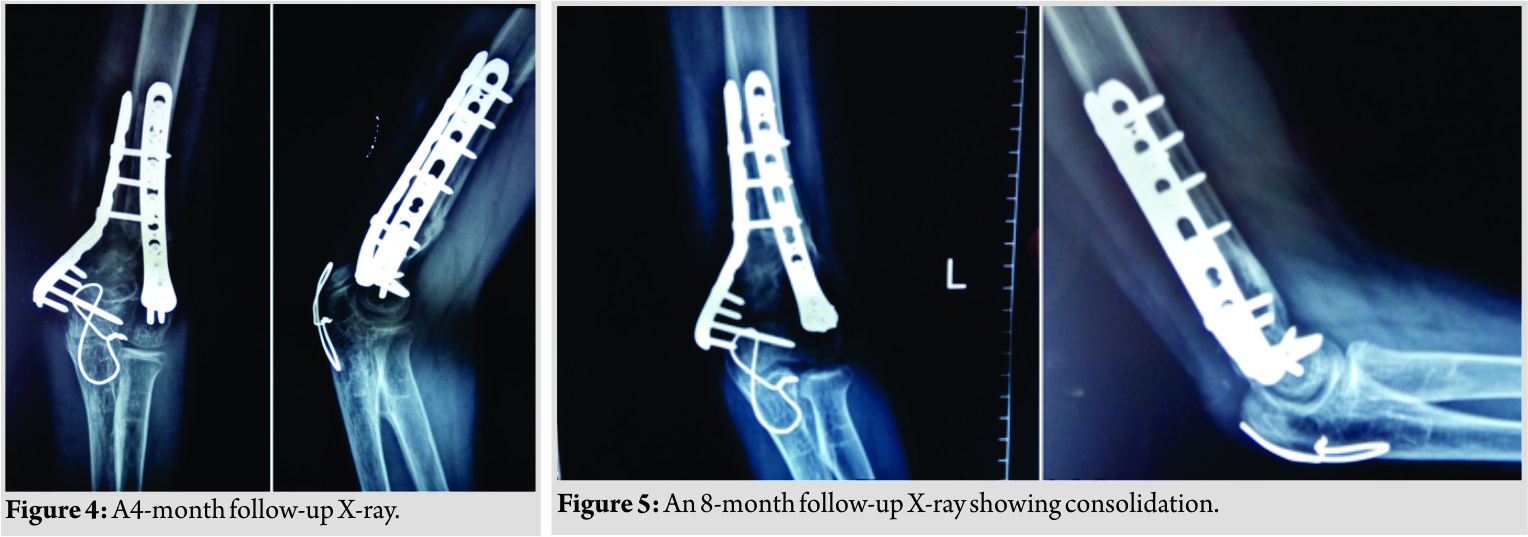
Discussion
SBCis commonly seen in the second decade of life. SBC of distal humerus is very rare accounting for <1%. Our patient presented with pathological fracture, which is the most common complication of SBC. There is no standard approach in the treatment of SBCs. The treatment strategy depends on the nature of presentation, whether pathological fracture is present or not. For lesions presenting without fracture, the main objectives of treatment include prevention of pathological fracture, eradication of the lesion, and pain relief [1]. Non-fractured SBC is treated with less aggressive techniques such as intralesional injection of methylprednisolone acetate, bone marrow aspirate, or demineralized bone matrix. Scaglietti et al. were the first to suggest intralesional steroid injection. They obtained 90% cure rates with local injection therapy and showed that surgical treatment of bone cysts in youth is seldom necessary in non-complicated cases [2]. In 2011, Canaves et al. compared the effect of percutaneous curettage, steroid injection, and autologous bone marrow injections. They found that mechanical disruption of the cyst membrane (percutaneous curettage) was associated with better cyst healing compared to simple intralesional injections [3]. Treatment of pathological fractures depends on the bone involved and the type of fracture. The priority for treatment is to treat the fracture first and then the lesion. Upto 15% of the lesions undergo spontaneous resolution following a fracture. Fractures of non-weight-bearing areas that are minimally displaced and stable can be managed with simple immobilization of the extremity for between 4 and 6weeks.The majority of the fractures heal, but the SBC will persist in upto 50% of cases and these lesions can be managed by non-surgical techniques. This technique of staged management reduces the need for internal fixation in children. However, this approach requires a long pre-operative and post-operative immobilization period in children resulting in stiffness of adjacent joints [4]. Majority of the fractures require curettage of the lesion and bone grafting with or without internal fixation. Unstable fractures or fracture in a weight-bearing bone require simultaneous treatment of fracture and the cyst. Fracture is fixed with suitable internal fixation and the cyst wall is curetted and the cavity filled with bone graft or bone graft substitute. This approach is associated with lesser chance of cyst recurrence and the internal fixation allows early mobilization [5]. Roposch et al., de Sanctis, Pogorelić et al.,and Erol et al. achieved high rates of cyst healing in children with pathologic fractures through acute intramedullary nailing. They showed that internal fixation with curettage gave better results for pathological fractures compared to other forms of treatment [6, 7, 8, 9]. Our patient had an unstable fracture of distal humerus that was managed by open reduction internal fixation, curettage, and autologous fibula grafting. There were no similar case reports in literature. The patient had a good outcome with complete resolution 6 months after surgery.
Conclusion
Unstable fractures and fractures in weight-bearing bones due to SBC require surgical curettage and bone grafting with simultaneous osteosynthesis. Stable fractures can be managed conservatively. Cyst recurrence after fracture healing requires curettage with or without bone grafting.
Clinical Message
Pathological fractures due to SBC in proximal humerus can be conservatively managed. However, in other areas such as distal humerus, proximal femur, and distal femur, the fracture is usually unstable. Such cases require early surgery with curettage of the lesion, internal fixation, and bone grafting. This allows early weight-bearing and mobilization and prevents recurrence.
References
1. Mascarda E, Gomez-Brouchet A, Lambot K. Bone cysts: Unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res 2015;101:S119-27.
2. Scaglietti O, Marchetti PG, Bartolozzi P. The effects of methylprednisolone acetate in the treatment of bone cysts. Results of three years follow-up. J Bone Joint Surg Br 1979;61-B:200-4.
3. Canavese F, Wright JG, Cole WG, Hopyan S. Unicameral bone cysts: Comparison of percutaneous curettage, steroid, and autologous bone marrow injections. J Pediatr Orthop 2011;31:50-5.
4. Muayad K, Mihir T, Amjed K, Laurens H. Treatment of unicameral bone cyst: systematic review and meta-analysis. J Child Orthop 2014;8:171-91.
5. De Mattos CB, Binitie O, Dormans JP. Pathological fractures in children. Bone Joint Res 2012;1:272-80.
6. de Sanctis NA. Elastic stable intramedullary nailing is the best treatment of unicameral bone cysts of the long bones in children: Prospective long-term follow-up study. J Pediatr Orthop 2006;26:520-5.
7. Pogorelić Z, Furlan D, Biocić M, Mestrović J, Jurić I, Todorić D, et al. Titanium intramedullary nailing for treatment of simple bone cysts of the long bones in children. Scott Med J 2010;55:35-8.
8. Erol B, Onay T, Çalışkan E, Aydemir AN, Topkar OM. Treatment of pathological fractures due to simple bone cysts by extended curettage grafting and intramedullary decompression. Acta Orthop Traumatol Turc 2015;49:288-96.
9. Roposch A, Saraph V, Linhart WE. Flexible intramedullary nailing for the treatment of unicameral bone cysts in long bones. J Bone Joint Surg Am 2000;82:1447-53.
 |
 |
| Dr. Hariharan Mohan | Dr. Balgovind S Raja |
| How to Cite This Article: Mohan H, Raja B S. Pathological Fracture of Distal Humerus due to a Simple Bone Cyst Managed with Fibula Grafting and Osteosynthesis. Journal of Orthopaedic Case Reports 2019 May-June; 9(3): 49-51. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




