[box type=”bio”] Learning Point of the Article: [/box]
Medial patellar dislocation is a rare condition, which often requires surgical treatment.
Case Report | Volume 9 | Issue 3 | JOCR May-June 2019 | Page 87-89 | G Pagliazzi, D Davanzo, M Delcogliano, Filippo Del Grande, C Candrian. DOI: 10.13107/jocr.2250-0685.1436
Authors: G Pagliazzi[1], D Davanzo[1], M Delcogliano[1], Filippo Del Grande[2], C Candrian[1]
[1]Department of Orthopedics and Traumatology, Lugano Regional Hospital, Via Tesserete 46, 6900 Lugano, Switzerland,
[2]Department of Radiology, Lugano Regional Hospital, Via Tesserete 46, 6900 Lugano, Switzerland.
Address of Correspondence:
Dr. Pagliazzi Gherardo,
Lugano Regional Hospital, Service of Orthopedics and Traumatology, Via Tesserete 46, 6900 Lugano, Switzerland.
E-mail: gherardo pagliazzi@eoc.ch
Abstract
Introduction: Patellar dislocation encompasses the 2–3% of the knee joint injuries, and lateral patellar luxation is by far more common than the medial one. Medial patellar dislocation is described only by few reports and generally as a consequence of previous surgeries. The purpose of this case report is to describe the surgical management of a rare case of traumatic bilateral medial patellar dislocation in a 15-year-old girl with no previous patellofemoral surgeries.
Case Report: The patient underwent a traumatic medial patellar dislocation on the left knee, and 18 months later also on the right one. In both cases, the first proposed treatment was a conservative therapy, encompassing the use of a brace and muscular imbalance correction. After a 6-month period, the patient still referred to the persistent sensation of “giving away,” so surgery was advised. The surgical operation consisted of an open medial retinacular release with complete dissection of the hypertrophic medial patellofemoral ligament and a transfer of the vastus medialis oblique to the superior border of the patella. Seven years after surgery, the patient declared to be satisfied with the procedure, referring only slight difficulty in squatting, jumping, and running. So far, no further episodes of dislocation occurred.
Conclusions: The present case report showed the favorable result of surgical correction of a unique case of bilateral non-iatrogenic medial patellar luxation, in the absence of any underlying bony-structural abnormality. No other papers dealing with medial traumatic bilateral patellar dislocation are found in current literature.
Keywords: Patellar dislocation, patellofemoral, medial patellofemoral ligament, vastus medialis oblique.
Introduction
Patellar dislocation encompasses the 2–3% of the knee joint injuries, affecting mainly young athletes, with a predilection toward the female gender [1, 2, 3]. Lateral patellar dislocation is by far more common than a medial patellar dislocation. The latter is usually the consequence of previous surgery, such as a lateral release, an excessive medialization of the tibial tubercle, or an over tight medial patellofemoral ligament (MPFL) graft [2, 4, 5]. The purpose of this case report is to describe the surgical management of a rare case of traumatic bilateral medial patellar dislocation in a 15-year-old girl with no previous patellofemoral surgeries.
Case Report
A healthy 15-year-old girl suffered a first episode of medial patellar dislocation of the left knee as a consequence of a traumatic impact during a skiing accident. In the following 9 months, she reported further eight spontaneous luxation episodes, which resolved after auto repositioning. The patient did not refer to any previous surgery. At the clinical examination, the left patella appeared to be medialized compared to the opposite healthy side; the medial shift test showed a clear tendency toward medial subluxation accompanied by patient’s discomfort (positive medial apprehension test) (Fig. 1). The lateral retinacular showed to be hyperlax. Pre-operative imaging assessment included weight-bearing anteroposterior and lateral views of both knees (Fig. 2).
The lateral retinacular showed to be hyperlax. Pre-operative imaging assessment included weight-bearing anteroposterior and lateral views of both knees (Fig. 2). 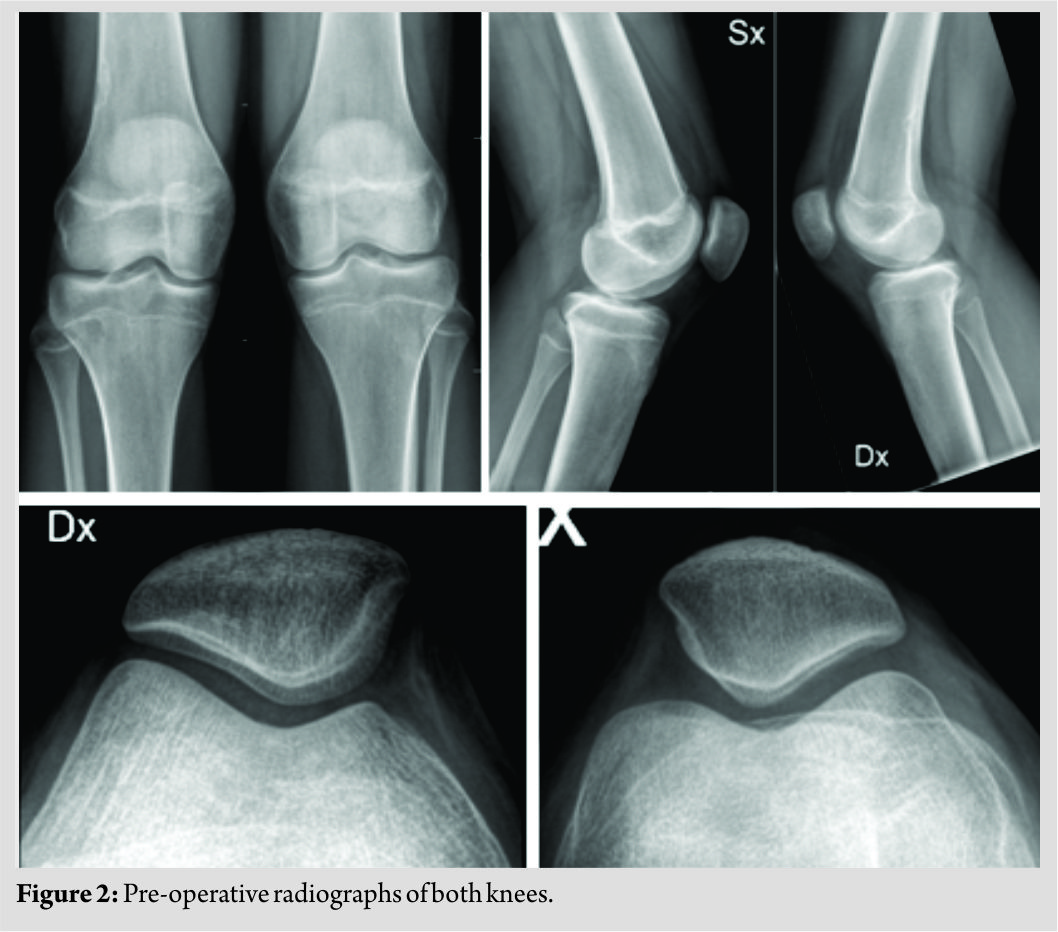 A magnetic resonance imaging (MRI) and also a computed tomography-scan of the left knee were collected. No rotatory malalignment was found. As pathological MRI findings, substantial hypertrophy of both the medial patellar retinaculum and the tendon of the oblique medial vastus muscle was documented. The initially proposed conservative treatment encompassed the use of a brace during sports activities and muscular imbalance correction. As the girl referred persistent sensation of “giving away,” 10 months after the first dislocation episode, the surgical operation was performed. It consisted in an open medial retinacular release with complete dissection of the hypertrophic MPFL and a transfer of the vastus medialis oblique (VMO) to the superior border of the patella (Figs. 3 and 4).
A magnetic resonance imaging (MRI) and also a computed tomography-scan of the left knee were collected. No rotatory malalignment was found. As pathological MRI findings, substantial hypertrophy of both the medial patellar retinaculum and the tendon of the oblique medial vastus muscle was documented. The initially proposed conservative treatment encompassed the use of a brace during sports activities and muscular imbalance correction. As the girl referred persistent sensation of “giving away,” 10 months after the first dislocation episode, the surgical operation was performed. It consisted in an open medial retinacular release with complete dissection of the hypertrophic MPFL and a transfer of the vastus medialis oblique (VMO) to the superior border of the patella (Figs. 3 and 4). 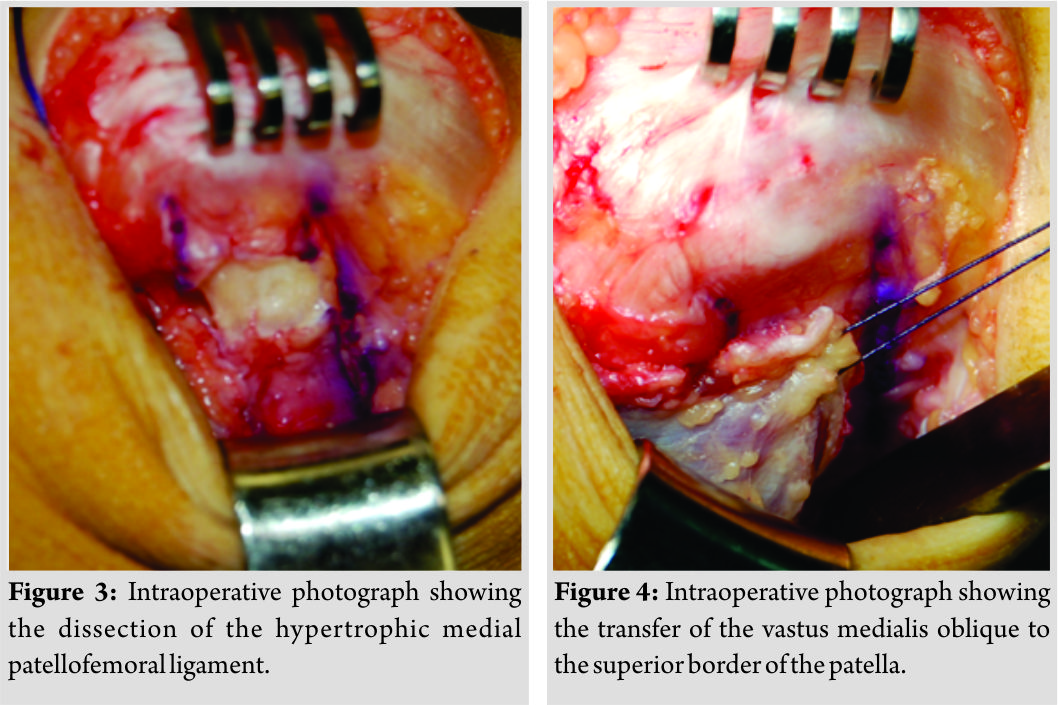 The medial retinaculum was dissected on a line drawn from 1 cm medial to the superior pole of the patella to the anteromedial portal. The inferomedial corner of the VMO was detached, and then transferred and sutured to the superomedial pole of the patella, using No. 2 PDS sutures with the knee flexed at 30°. The lateral retinaculum was tensioned, dissecting the two layers and consequently suturing them together in a “pants over vest” fashion. We did not perform a lateral retinaculum reconstruction to avoid over tightening. At the end of the surgery, we achieve regular patellar tracking without any tendency to medial or lateral subluxation during stress-testing. Postoperatively, the knee was placed in a knee brace, and partial weight bearing was advised for the first 4 weeks. Flexion was limited at 45° within the first 2 weeks, and at 90° within the first 4 weeks. Recovery to a full weight bearing was permitted 4 weeks after surgery, and range of motion was gradually increased. The post-operative 6 and 12-week follow-up showed promising results as far as the patient walked without pain and/or sensation of instability. Eight months after surgery on the left knee, the patient experienced a traumatic medial patellar dislocation also in the right knee, occurred during sports activity. Furthermore, in this case, the conservative treatment did not lead to favorable results. The right knee was addressed surgically with the same surgical steps already performed on the contralateral knee. The post-operative protocol was the same used for the left knee. The patient was reassessed 7 years after the surgical operation on the left knee and 6 years after surgical correction of the right one; so far, no further episodes of dislocation have occurred. In the right knee, the Lysholm score improves from 48 to 87, while the Kujala score increased from 55 to 88. The pre-operative Lysholm and patellofemoral Kujala scores improved, respectively, from 45 to 85 and from 56 to 88 in the left knee. The patient declared to be highly satisfied with the procedure, and the only complain was a slight difficulty in squatting, jumping, and running.
The medial retinaculum was dissected on a line drawn from 1 cm medial to the superior pole of the patella to the anteromedial portal. The inferomedial corner of the VMO was detached, and then transferred and sutured to the superomedial pole of the patella, using No. 2 PDS sutures with the knee flexed at 30°. The lateral retinaculum was tensioned, dissecting the two layers and consequently suturing them together in a “pants over vest” fashion. We did not perform a lateral retinaculum reconstruction to avoid over tightening. At the end of the surgery, we achieve regular patellar tracking without any tendency to medial or lateral subluxation during stress-testing. Postoperatively, the knee was placed in a knee brace, and partial weight bearing was advised for the first 4 weeks. Flexion was limited at 45° within the first 2 weeks, and at 90° within the first 4 weeks. Recovery to a full weight bearing was permitted 4 weeks after surgery, and range of motion was gradually increased. The post-operative 6 and 12-week follow-up showed promising results as far as the patient walked without pain and/or sensation of instability. Eight months after surgery on the left knee, the patient experienced a traumatic medial patellar dislocation also in the right knee, occurred during sports activity. Furthermore, in this case, the conservative treatment did not lead to favorable results. The right knee was addressed surgically with the same surgical steps already performed on the contralateral knee. The post-operative protocol was the same used for the left knee. The patient was reassessed 7 years after the surgical operation on the left knee and 6 years after surgical correction of the right one; so far, no further episodes of dislocation have occurred. In the right knee, the Lysholm score improves from 48 to 87, while the Kujala score increased from 55 to 88. The pre-operative Lysholm and patellofemoral Kujala scores improved, respectively, from 45 to 85 and from 56 to 88 in the left knee. The patient declared to be highly satisfied with the procedure, and the only complain was a slight difficulty in squatting, jumping, and running.
Discussion
The present case report showed the favorable result of surgical correction of a unique case of bilateral non-iatrogenic medial patellar luxation, in the absence of any underlying bony-structural abnormality. No other papers dealing with medial traumatic bilateral patellar dislocation are found in current literature. Medial patellar luxation was first described by Hughston and Deese in a cohort of patients previously treated with arthroscopic lateral retinacular release associated with vastus lateralis release [4]. Other cases dealing with medial patellar subluxation after failed patellofemoral surgeries are reported in current literature. McCarthy and Bollier reported three cases after MPFL malpositioning and over tightening, associated with the lateral retinacular release [6]. Aksahin et al. reported a case of a 21-year-old male with spontaneous medial patellar instability treated with the imbrication of lateral structures and a patellotibial ligament augmentation [7]. No pathophysiologic explanation for spontaneous medial patellar instability was found in literature [8, 9, 10]. In our opinion, medial instability was due both to the preponderance of the medial structures, especially the vastus medialis, and the inability of the lateral structures to function as a rein, thus limiting medial translation. Surgical correction has shown to be capable to obtain favorable results at a remarkable follow-up of 7 years. Nevertheless, lacking the final follow-up radiographs, to predict the development of patellofemoral osteoarthritis, is the major limitation of this case report. In literature, good to excellent outcomes was reported postoperatively in most of the patients after surgical correction of medial patellar instability. Unfortunately, unlike lateral patellar dislocation, clear recommendations regarding indications and surgical procedures are still missing.
Conclusion
Up to now, no other case series dealing with bilateral traumatic patellar dislocation are reported in literature. The patient underwent a soft tissue procedure in both knees and the results were favorable. The patient declared to be satisfied with the operation.
Clinical Message
Medial patellar dislocation is a rare condition, especially in non-operated knees. Surgical treatment is challenging but frequently needed. In the absence of an underlying bone deformity, a soft tissue procedure is usually able to stabilize the patella.
References
1. Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med 2002;21:499-519.
2. Moatshe G, Cram TR, Chahla J, Cinque ME, Godin JA, LaPrade RF. Medial patellar instability: Treatment and outcomes. Orthop J Sports Med 2017;5:2325967117699816.
3. Gravesen KS, Kallemose T, Blønd L, Troelsen A, Barfod KW. High incidence of acute and recurrent patellar dislocations: A retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg Sports Traumatol Arthrosc 2017;26:1204-9.
4. Hughston JC, Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med 1998;16:383-8.
5. Hughston JC, Flandry F, Brinker MR, Terry GC, Mills JC 3rd. Surgical correction of medial subluxation of the patella. Am J Sports Med 1996;24:486-91.
6. McCarthy MA, Bollier MJ. Medial patella subluxation: Diagnosis and treatment. Iowa Orthop J 2015;35:26-33.
7. Aksahin E, Yumrukcal F, Yuksel HY, Dogruyol D, Celebi L. Role of pathophysiology of patellofemoral instability in the treatment of spontaneous medial patellofemoral subluxation: A case report. J Med Case Rep 2010;4:148.
8. Petri M, Ettinger M, Stuebig T, Brand S, Krettek C, Jagodzinski M, et al. Current concepts for patellar dislocation. Arch Trauma Res 2015;4:e29301.
9. Nonweiler DE, DeLee JC. The diagnosis and treatment of medial subluxation of the patella after lateral retinacular release. Am J Sports Med 1994;22:680-6.
10. Richman NM, Scheller AD Jr. Medial subluxation of the patella without previous lateral retinacular release. Orthopedics 1998;21:810-3.
 |
 |
 |
 |
 |
| Dr. G Pagliazzi | Dr. D Davanzo | Dr. M Delcogliano | Dr. Filippo Del Grande | Prof. C Candrian |
| How to Cite This Article: Pagliazzi G, Davanzo D, Delcogliano M, Del Grande F , Candrian C. Traumatic bilateral medial patellar instability in a 15-year-old girl. Journal of Orthopaedic Case Reports 2019 May-June; 9(3): 87-89. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




