[box type=”bio”] Learning Point of the Article: [/box]
Avulsion of the patellar tendon from the tibial tubercle is uncommon and presents a unique treatment challenge since sutures cannot be as easily passed in a tranosseous fashion. Combining this unique challenge with a history of previous surgery may compromise patella tendon quality making it unsuitable for primary repair.
Case Report | Volume 9 | Issue 5 | JOCR September – October 2019 | Page 26-30 | Sarah Dawn Lang, Matthew Robert Henry Irons, Brian Brandon Gilmer. DOI: 10.13107/jocr.2019.v09i05.1518
Authors: Sarah Dawn Lang[1], Matthew Robert Henry Irons[1], Brian Brandon Gilmer[1]
[1]Department of Orthopaedics, Mammoth Orthopedic Institute, PO Box 660, Mammoth Lakes, California 93546, U.S.A.
Address of Correspondence:
Dr. Brian Brandon Gilmer,
Mammoth Orthopedic Institute, PO Box 660, Mammoth Lakes, California 93546, U.S.A.
E-mail: Brian.gilmer@mammothhospital.com
Abstract
Introduction: Pre-existing conditions and surgical interventions, such as those associated with Osgood-Schlatter disease, can lead to atypical patellar tendon ruptures. These cases can present irregularly and be challenging to diagnose. Patellar tendon rupture from the tibial tubercle insertion region is a rare, and currently undocumented condition, requiring surgical intervention to restore knee joint functionality for daily activities. This presentation requires a unique treatment approach, as standard reconstruction techniques do not apply.
Case Report: A 65-year-old Caucasian male, with a remote history of gout and surgical intervention for symptomatic Osgood-Schlatter disease, suffered sudden hyperflexion with eccentric contraction of the right knee while hiking. The patient presented with massive right knee effusion and significant tenderness over the tibial tubercle, with an inability to extend the knee. After radiographs were inconclusive, magnetic resonance imaging was performed showing a tear of the medial aspect of the distal patellar tendon.
Conclusion: Surgical intervention for Osgood-Schlatter disease can be a potential risk factor for patellar tendon rupture from the tibial tubercle. Since a variety of surgical interventions for symptomatic Osgood-Schlatter disease exist, it is important to consider the long-term effects and counsel patients on the associated risks of the procedures. Initial diagnosis of patellar tendon rupture can be surprisingly challenging when the presentation is atypical. Attention to detail during physical examination and evaluation of imaging is a necessity for early detection and treatment, which can afford excellent functional outcomes.
Keywords: Patellar tendon avulsion, primary repair patella tendon, tendon augmentation, tibial tubercle avulsion.
Introduction
Ruptures of the patellar tendon most commonly occur as an avulsion directly from the inferior pole of the patella or a midsubstance tear near the proximal insertion. Since lack of active terminal knee extension leads to a deterioration of activities of daily living and loss of function, surgical intervention is the gold standard in both the acute and chronic patellar tendon rupture settings [1, 2]. Avulsion of the patellar tendon from the tibial tubercle is uncommon and presents a unique treatment challenge since sutures cannot be as easily passed in a transosseous fashion.
A history of previous surgery may compromise patellar tendon quality making it unsuitable for primary repair. In this occurrence, a primary rupture of a previously compromised tendon can mimic a chronic patellar tendon rupture. Primary repair alone is not indicated for chronic patellar tendon rupture because of superior patellar migration, poor tissue quality of the remaining tendon, bone atrophy of the patella, and tissue scarring [1, 3]. In chronic instances, tendon augmentation can be utilized to strengthen the construct and allows for earlier functional rehabilitation and range of motion exercise [4].
We present an unusual case of patellar tendon avulsion from the tibial tubercle in a patient who had undergone a remote procedurefor symptomatic Osgood-Schlatter disease.
Case Report
A 65-year-old male sustained a sudden traumatic hyperflexion, eccentric contraction of his right knee while hiking. Four days after the event, he presented to the outpatient orthopedic clinic with a massive effusion, loss of motion, and inability to achieve active terminal knee extension. His passive range of motion was 60 degrees with painlimiting knee flexion. He was able to ambulate unassisted with a mild antalgic gait with the knee maintained in extension. Both knees demonstrated large prominent ossicles over the tibial tubercles consistent with Osgood-Schlatter disease. The right knee was maximally tender over the tibial tubercle, and there was no palpable defect at the inferior pole of the patella.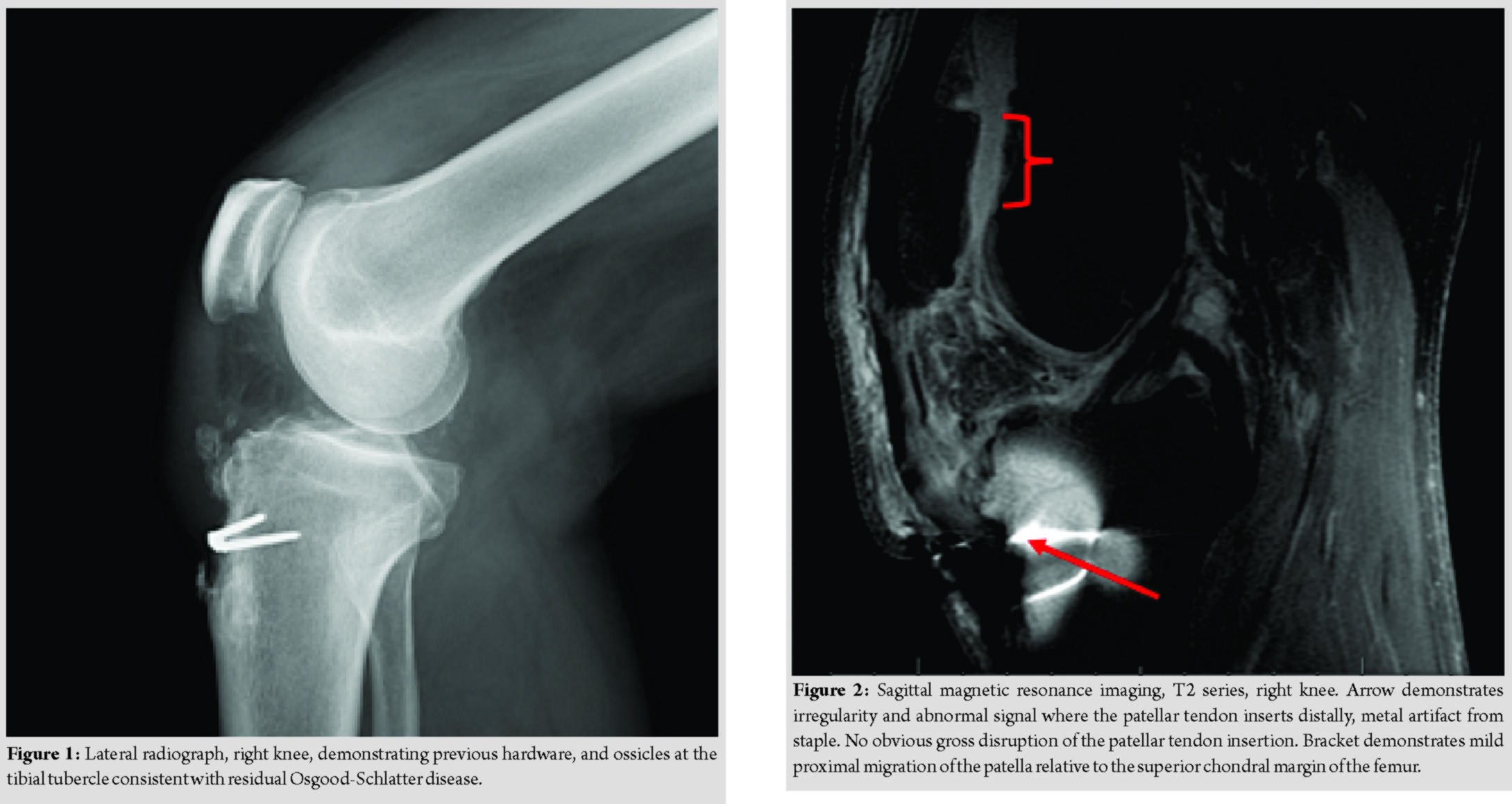
The patient reported amedical history of gout and surgical history of a procedure performed in young adulthood for symptomatic Osgood-Schlatter disease. While the operative records and reports were unavailable, the patient indicated the procedure included trephination and open debridement of the tubercle with a staple inserted for fixation of the tendon to the remaining tibial tubercle. He further indicated this was conducted after reaching skeletal maturity. The patient reported no history of previous patellar instability or arthrosis to indicate the procedure may have, in fact, been a tibial tubercle osteotomy fixed with staples. He reported the procedure was considered experimental at the time and was specifically for the treatment of patellar tendinopathy.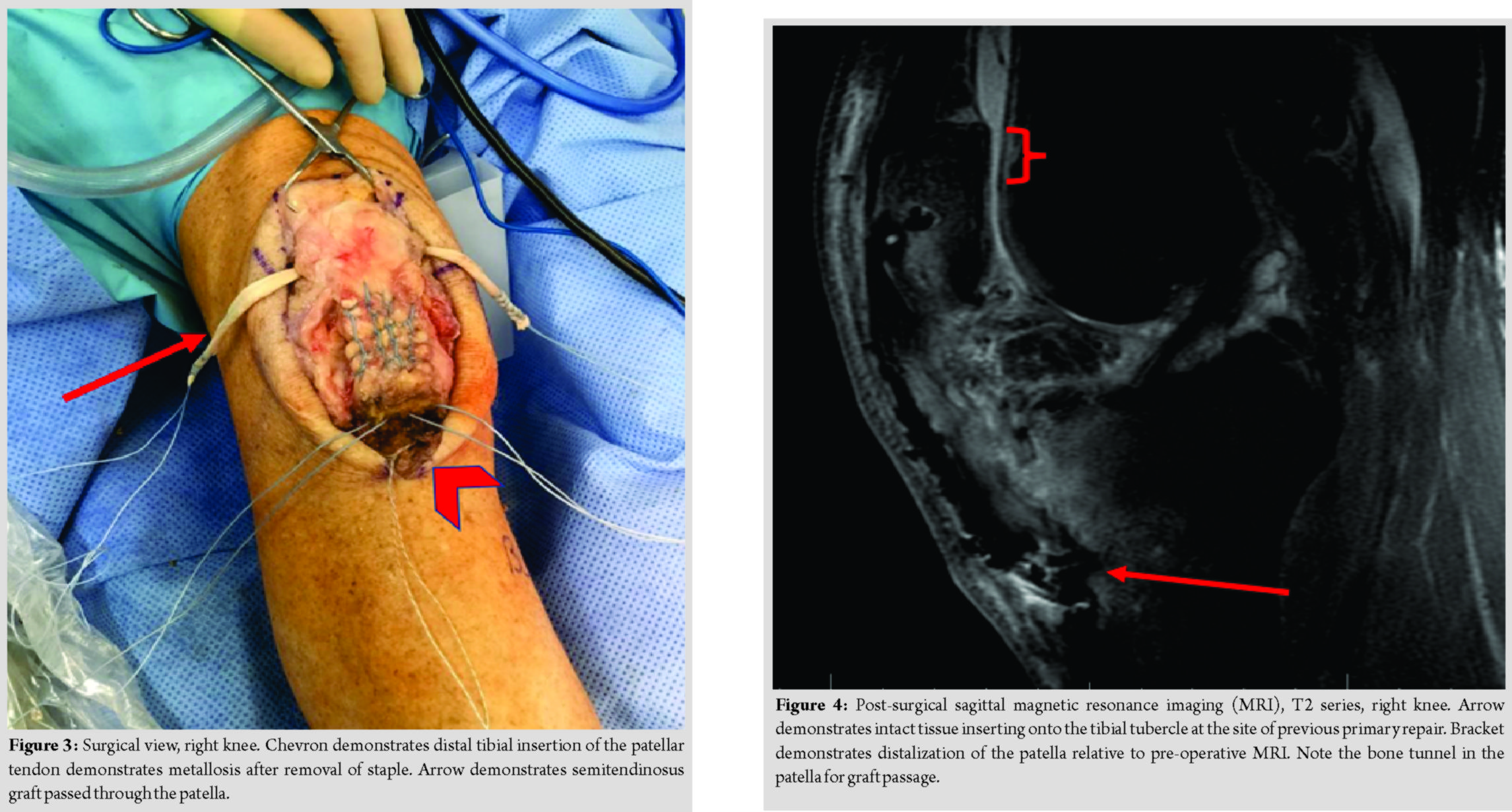
Radiographs revealed a staple from his prior procedure. On the lateral view, several exostoses remained apparent at the tibial tubercle. There was a mild superior migration of the patella compared to a contralateral knee image (Fig. 1). Because of the patient’s history, atypical findings on physical examination, and radiographs; a magnetic resonance imaging (MRI) was performed, revealing a tear of the medial aspect of the distal patellar tendon near the insertion on the tibial tubercle and metallic staple. The examination was limited due to artifact from the staple. MRI demonstrated a normal-appearing patellar tendon inserting onto the inferior pole of the patella (Fig. 2). Given the combination of an MRI confirming a compromised patella tendon and a clinical exam of tenderness over the insertion on the tibial tubercle, lack of ability to perform a straight leg raise and an extension lag; surgical intervention was determined necessary. A knee arthroscopy, examination under anesthesia, and open patellar tendon reconstruction were planned.
Surgical treatment
Initially, diagnostic arthroscopy was performed which revealed no underlying intraarticular pathology. Attention was then turned to the open procedure. The previous incision, a medial parapatellar arthrotomy was identified and opened. Severe chronic prepatellar bursitis was encountered and excised down to the level of the intact retinaculum. The patellar tendon itself was thickened and fibrous. The tendon remained lax with the knee in extension, at 30 degrees flexion, and at 90 degrees flexion. There were a few remaining fibers in continuity laterally which gave the appearance of an intact tendon and prevented gross proximal migration of the patella. Distally, the tendon was abnormal in its appearance at the tibial tubercle with significant metallosis and degeneration of the tendon and underlying bone. An osteotome was used to remove the hardware resulting in leaving the distal tendon very thin and friable and of very poor tissue quality (Fig. 3). Due to the poor tissue quality, the decision was made to proceed with primary repair and allograft augmentation. The remainder of the patella was exposed proximally. A semitendinosus allograft was prepared at a diameter of 4 mm. Each end was whipstitched with a #2 looped non-absorbable suture. A 5 mm reamer was placed in the central aspect of the patella, and drilling was undertaken lateral to medial in preparation for passing the graft. This was confirmed under fluoroscopic guidance to ensure the chondral surface was not compromised, and the dorsal aspect of the patella was not at risk of fracture. A #5 FiberWire was used in a modified Krakow fashion exiting in the midportion of the tendon distally. This was repeated on the opposite side providing a four-strand repair. This was vigorously pulled and the tissue was well fixed. Two 4.75 mm suture anchors (SwiveLok, Arthrex Inc., Naples, FL) were placed in the tibial tubercle securing the four-stranded repairs to the tibial tubercle. The knee was held in terminal extension during fixation. This provided a stable repair to 90 degrees without gapping. Once the sutures were placed, the allograft was shuttled across the horizontal tunnel in the patella. A separate tunnel was then placed at the level of the tibial tubercle just distal to the anchors, and one limb of the semitendinosus allograft was placed medial to lateral. The knee was placed at 30 degrees knee flexion allowing the two suture limbs of the graft to be tied to one another and then tied with additional sutures to the native tendon proximally and more distally. Before final graft passage and fixation, intraoperative fluoroscopy was utilized to confirm the placement of the tunnel in a central location in the patella to reduce iatrogenic fracture risk, and imaging was performed of the contralateral knee to determine the appropriate tensioning of the graft to prevent patella alta or baja. The knee was again ranged to 90 degrees and which demonstrated a fluid range of motion with maintained integrity of the repair. Postoperatively, the patient was allowed weight bearing as tolerated with knee locked in full extension in a brace and allow 0–90 degrees knee flexion to prevent stiffening for the first 6 weeks. After the 6 weeks period, the patient gradually weaned from the brace and began gait training. Physical therapy was initiated after 1 week to allow for healing of the incision. The physical therapy protocol was the same as used for quadriceps and patellar tendon ruptures in our institution. This protocol includes active and active-assisted flexion to 90 degrees for the first 6 weeks with gentle passive range of motion as tolerated. After 6 weeks range of motion is increased incrementally to full and the brace is unlocked sequentially at higher flexion angles until the brace is discontinued around 10–12 weeks and gait has normalized. Formal strengthening is initiated at 3 weeks emphasizing closed chain exercises first and progressing to open chain exercises as tolerated. Full return to activities is typically allowed between 4 and 6 months. A complete description of the post-operative protocol may be referenced here: https://www.mammothortho.com/pdf/quadriceps-tendon-repair-gilmer.pdf
Follow-up
Six weeks postoperatively, the patient had returned to activity and experienced an insidious onset of pain and edema after increasing his activity without discrete injury. He presented with a large effusion, and on evaluation, he demonstrated difficulty and pain with straight leg raise but no extension lag. A bedside ultrasound was performed in the clinic of the patella tendon and adjacent structures and revealed the integrity of the repair and graft were intact. An MRI was obtained which confirmed the integrity of the patella tendon, the graft, and maintained the distal position of the patella relative to the initial presentation (Fig. 4). The decision was made to use crutches as needed with his post-operative brace locked in extension for ambulating. An aspiration was recommended, but the patient deferred due to concerns of infection. He was treated symptomatically for a presumed gout flare with indomethacin. Uric acid levels were drawn but were within normal limits. Two weeks later, the patient returned to clinic reporting complete resolution of symptoms. The remainder of his recovery was uneventful and he returned to full activities and CrossFit 4 months postoperatively and was discharged from further follow-up. Incidentally, the patient returned for an unrelated injury to his wrist 15 months postoperatively. At that time, he reported no complaints of pain or weakness and had full flexion and extension strength without clinical evidence of atrophy. He reported continued high-impact activities without limitation.
Discussion
Rupture of the patellar tendon from the tibial tubercle is uncommon [5, 6, 7]. Surprisingly, the diagnosis of patellar tendon rupture can, at times, be challenging. Critical evaluation of radiographs and careful physical exam in the setting of high clinical suspicion based on history are paramount in making an early and accurate diagnosis. In most cases, early primary repair yields excellent functional results [8]. Partial injuries can be even more challenging to diagnose and treat because intact tendon or retinaculum can prevent gross superior migration of the patella. Cooper and Selesnick reported partial ruptures of the distal patellar tendon in two skeletally mature athletes. Like our patient, those in their series had a history of tendinosis and in one case, previously diagnosed Osgood-Schlatter disease [9]. Late presentation or misdiagnosed patellar tendon rupture results in a clinical scenario which compromises the results of primary repair. Siwek and Rao reported 38% of the knee extensor ruptures were misdiagnosed at the time of the initial visit, and 18% had progressed to chronic cases more than 2 weeks after the injury, before diagnosis [10]. In these cases, reconstructive techniques are often required [11]. Classically, this entity is associated with predisposing factors in adults such as chronic kidney insufficiency, diabetes, rheumatoid arthritis, fluoroquinolone treatment, hyperparathyroidism, and corticosteroid injection or systemic treatment. None of these risk factors was present in this patient. Osgood-Schlatter disease itself has not been commonly cited as a risk factor for patellar tendon rupture from the tibial tubercle. In this case, there was prior surgical management for Osgood-Schlatter disease, and we hypothesize the surgical intervention with a combination of chronic tendinopathy resulted in a predisposition to traumatic rupture. Several procedures, both arthroscopic and open, have been described for the treatment of symptomatic Osgood-Schlatter disease [12, 13, 14, 15]. Surgeons considering these should consider the potential effects on the extensor mechanism and counsel patients regarding the potential risks of late tendon rupture. Di Giacomo et al. presented a similar case of atraumatic patellar tendon avulsion which was treated with a primary repair [16]. These authors utilized transosseous suture fixation in the tubercle with #5 FiberWire and did not utilize a graft. That patient had minimal trauma and insidious onset of pain without a history of prior surgical intervention and had some mild limitations and pain at final follow-up. In contrast, our patient had a more acute traumatic presentation with a history of prior surgery and had no functional limitations despite returning to a high level of physical activity. Based on our current experience, reconstruction of patellar tendon avulsions in the setting of prior surgery should be approached in a manner similar to chronic patellar tendon rupture. Because of the abnormal tissue quality, augmentation with additional collagen should be strongly considered as an adjunct to primary repair. Several techniques have been described for allograft reconstruction of the extensor mechanism [11]. Interestingly, other clinical entities in the early postoperative period may present with extension pain but do not necessarily indicate a compromise of the extensor mechanism and care should be taken to establish a clear diagnosis before any additional surgical exploration or procedure. In these cases, ultrasound and MRI may be useful modalities to evaluate the integrity of the tissue.
Conclusion
Surgical intervention for Osgood-Schlatter disease can be a potential risk factor for patellar tendon rupture from the tibial tubercle. Since a variety of surgical interventions for symptomatic Osgood-Schlatter disease exist, it is important to consider the long-term effects and counsel patients on the associated risks of the procedures. Initial diagnosis of patellar tendon rupture can be surprisingly challenging when the presentation is atypical. Attention to detail during physical examination and evaluation of imaging is a necessity for early detection and treatment, which can afford excellent functional outcomes.
Clinical Message
Avulsion of the patellar tendon from the tibial tubercle is uncommon and presents a unique treatment challenge since sutures cannot be as easily passed in a transosseous fashion. Combining this unique challenge with a history of previous surgery may compromise patellar tendon quality making it unsuitable for primary repair.
References
1. Harato K, Kobayashi S, Udagawa K, Iwama Y, Masumoto K, Enomoto H, et al. Surgical technique to bring down the patellar height and to reconstruct the tendon for chronic patellar tendon rupture. Arthrosc Tech 2017;6:e1897-e1901.
2. Greis PE, Lahav A, Holmstrom MC. Surgical treatment options for patella tendon rupture, part II: Chronic. Orthopedics 2005;28:765-9.
3. Temponi EF, Camelo N, Tuteja S, Thaunat M, Daggett M, Fayard JM, et al. Reconstruction of chronic patellar tendon rupture with contralateral bone-tendon-bone autograft. Knee Surg Sports TraumatolArthrosc2017;25:2468-73.
4. Maffulli N, Buono AD, Oliva F. Ipsilateral hamstring tendon graft reconstruction for chronic patellar tendon ruptures: Surgical technique. Muscles Ligaments Tendons J 2017;7:157-62.
5. Chloros GD, Razavi A, Cheatham SA. Complete avulsion of the patellar tendon from the tibial tubercle in an adult without predisposing factors. J Orthop Sci 2014;19:351-3.
6. Capogna B, Strauss E, Konda S, Dayan A, Alaia M. Distal patellar tendon avulsion in association with high-energy knee trauma: A case series and review of the literature. Knee 2017;24:468-76.
7. Clarke DO, Franklin SA, Wright DE. Avulsion fracture of the tibial tubercle associated with patellar tendon avulsion. Orthopedics 2016;39:e561-4.
8. Larsen E, Lund PM. Ruptures of the extensor mechanism of the knee joint. Clinical results and patellofemoral articulation. Clin OrthopRelat Res 1986;???:150-3.
9. Cooper ME, Selesnick FH. Partial rupture of the distal insertion of the patellar tendon. A report of two cases in professional athletes. Am J Sports Med 2000;28:402-6.
10. Siwek CW, Rao JP. Ruptures of the extensor mechanism of the knee joint. J Bone Joint Surg Am 1981;63:932-7.
11. Gilmore JH, Clayton-Smith ZJ, Aguilar M, Pneumaticos SG, Giannoudis PV. Reconstruction techniques and clinical results of patellar tendon ruptures: Evidence today. Knee 2015;22:148-55.
12. Pihlajamäki HK, Mattila VM, Parviainen M, Kiuru MJ, Visuri TI. Long-term outcome after surgical treatment of unresolved osgood-schlatter disease in young men. J Bone Joint Surg Am 2009;91:2350-8.
13. DeBerardino TM, Branstetter JG, Owens BD. Arthroscopic treatment of unresolved osgood-schlatter lesions. Arthroscopy 2007;23:1127.e1-3.
14. El-Husseini TF, Abdelgawad AA. Results of surgical treatment of unresolved osgood-schlatter disease in adults. J Knee Surg 2010;23:103-7.
15. Kaya DO, Toprak U, Baltaci G, Yosmaoglu B, Ozer H. Long-term functional and sonographic outcomes in osgood-schlatter disease. Knee Surg Sports TraumatolArthrosc2013;21:1131-9.
16. Di Giacomo LM, Khan MS, Bisaccia M, Rende R, Rinonapoli G, Caraffa A, et al. Surgical repair of an atraumatic avulsion of patellar tendon at the tibial tuberosity in an adult patient. Case Rep Orthop2015;2015:192023.
 |
 |
 |
| Dr. Sarah Dawn Lang | Dr. Matthew Robert Henry Irons | Dr. Brian Brandon Gilmer |
| How to Cite This Article: Lang S D, Irons M R H, Gilmer B B. Repair of Patellar Tendon Avulsion from the Tibial Tubercle: Case Report. Journal of Orthopaedic Case Reports 2019 Sep-Oct; 9(5): 26-30. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com








