[box type=”bio”] Learning Point of the Article: [/box]
Pyogenic vertebral osteomyelitis even though rare in children responds well to antibiotic therapy when instituted in time and heals without any sequelae.
Case Report | Volume 10 | Issue 2 | JOCR March – April 2020 | Page 70-72 | Sitanshu Barik, P Venkata Sudhakar, Shobha S Arora. DOI: 10.13107/jocr.2020.v10.i02.1702
Authors: Sitanshu Barik[1], P Venkata Sudhakar[1], Shobha S Arora[1]
[1]Department of Orthopaedic Surgery, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
Address of Correspondence:
Dr. Sitanshu Barik,
Department of Orthopaedic Surgery, All India Institute of Medical Sciences, Veerbhadra Marg, Rishikesh – 249 203, Uttarakhand, India.
E-mail: sitanshubarik@gmail.com
Abstract
Introduction: Pyogenic vertebral body osteomyelitis is rarer in children in comparison to adults. A rare case of pyogenic vertebral body osteomyelitis in a 10-year-old male is presented which was managed conservatively with antibiotics on the basis of antibiogram of blood culture. With 6 weeks of antibiotic therapy and at 12-month follow-up, the patient has no symptoms with no affection of any activity. This should be considered as a differential diagnosis in pediatric patients presenting with atypical symptoms related to spine and hip.
Case Report: A 10-year-old child presented with a 7-day history of progressively increasing insidious onset pain in the lower back radiating to the right hip, with an associated limp and restriction of floor level activities and activities of daily living. On examination, the child had tenderness at L3, L4, and L5 vertebral level and normal neurology in both lower limbs. A pseudoflexion deformity 20° was also noted in the right hip with normal range of motion in other planes. Keeping a differential of infective etiology of either hip or spine, routine blood investigations, blood culture, and radiological evaluation were done which included X-rays of lumbosacral spine and hip, ultrasound of bilateral hips and abdomen, and magnetic resonance imaging (MRI) of lumbosacral spine. The blood investigations showed an increase in white blood cell count, erythrocyte sedimentation rate, and high-sensitivity C-reactive protein, with the isolation of methicillin-sensitive Staphylococcus aureus in blood culture. Ultrasonography of hip showed mild effusion in the right hip and collections in the psoas; MRI confirmed the findings with an enhancement of L4 vertebral body.
Conclusion: Pyogenic vertebral body osteomyelitis is a rare diagnosis in children that should be considered in patients with atypical symptoms. MRI is the investigation of choice with prompt antibiotic therapy instituted on time which leads to healing without any sequelae.
Keywords: Pyogenic vertebral body osteomyelitis, spine, methicillin-sensitive Staphylococcus aureus.
Introduction
Vertebral body involvement occurs commonly in adults with hematogenous osteomyelitis. In children, pyogenic osteomyelitis commonly involves the long bones of the appendicular skeleton rather than the axial skeleton [1]. Pyogenic infection of the spine was first reported by Lannelongue, in 1879; however, spondylodiscitis was not defined as an independent entity until 1925 by Mayer [2]. Among the pyogenic infections, the term spondylodiscitis covers vertebral osteomyelitis, spondylitis, and discitis, which are different manifestations of the same disease process [3]. Pyogenic vertebral osteomyelitis is diagnosed infrequently in children. Because its presentation often is subtle and non-specific, vertebral osteomyelitis may not be considered in the initial evaluation, resulting in a delay in the diagnosis and initiation of treatment [4]. Patients with pyogenic vertebral osteomyelitis usually present with fever with pain over the affected area of spine. Discitis and vertebral osteomyelitis were once considered distinct entities; however, most clinicians now believe they represent a similar infectious process with bacterial infection originating in the well-perfused end plate and extending into the disc and vertebral body. We present a case of pyogenic vertebral body osteomyelitis in a 10-year-old child which was managed conservatively after ruling out tuberculosis in a tuberculosis endemic country.
Case Report
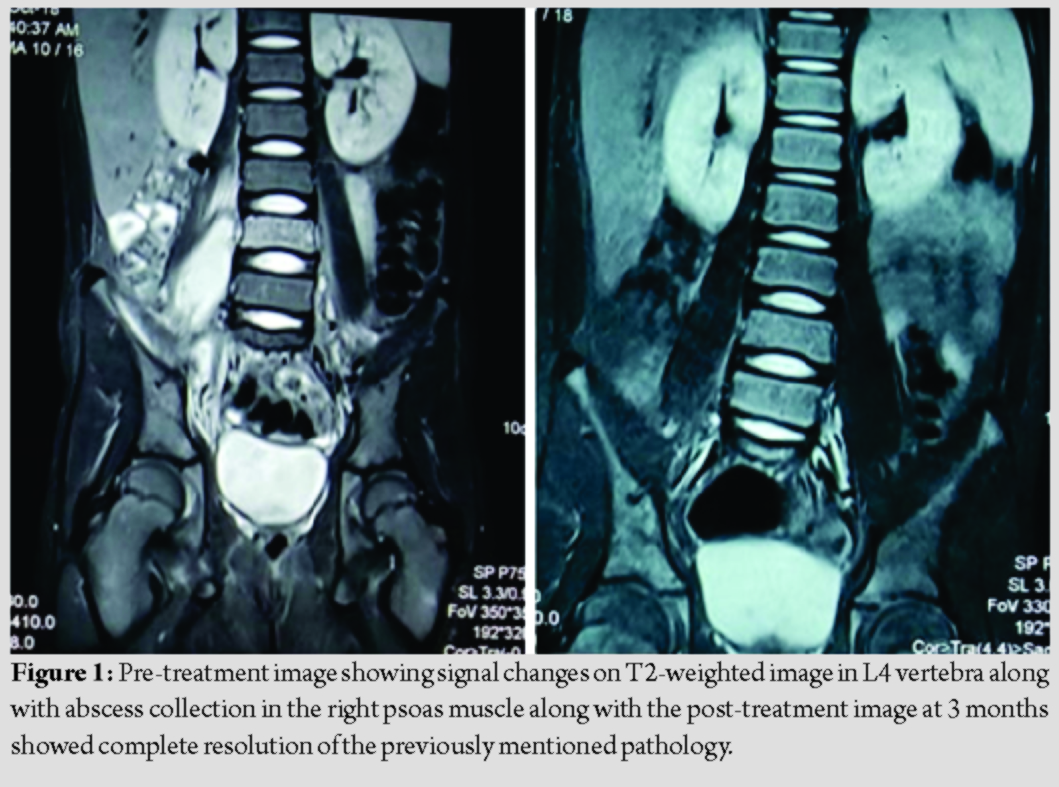
A 10-year-old child presented with a 7-day history of progressively increasing pain of insidious onset in the lower back radiating to the right hip, aggravating during night which was associated with high-grade fever and constitutional symptoms. There was an associated limp, present since the onset of pain with restriction of floor level activities. The patient was able to perform his activities of daily living before the onset of symptoms. There was no history of trauma nor any close contact with any tuberculosis patient in recent months. On general examination, no grossly evident swellings or any foci of infection were present. The gait of the child was markedly normal. Tenderness at L3, L4, and L5 level was noted with no other significant findings in the spine. Neurological status of both lower limbs was normal. A fixed flexion deformity of 20° of the right hip was present with further flexion up to 100°. Range of motion in other planes was normal in the hip joint. The movements in the right hip were associated with discomfort but not outright pain. A clinical diagnosis of an infective etiology of either hip or spine was made. The total white blood cell (WBC) count was 23,100 cells/mm3 (4000–11,000), erythrocyte sedimentation rate (ESR) 20 mm/h (up to 10 mm/h), and high-sensitivity C-reactive protein (hS-CRP) was 146.25 mg/dl (<2 mg/dl) at presentation. Ultrasonography (USG) of bilateral hip joints and abdomen showed mild effusion in the right hip with the left hip being normal and a well-defined hypoechoic area measuring 3.3*4.4*5.2 cm in the right psoas without any mobile internal contents. To further delineate the extent of abscess and the health and status of the spinal cord, magnetic resonance imaging (MRI) of lumbosacral spine was done which showed a large collection of dimensions 11.2*2.3*2.5 cm, hypointense on T1W images and hyperintense on T2W and short-tau inversion recovery (STIR) sequences were noted in the right psoas muscle, extending from the L2 vertebral body up to iliopsoas complex and further extending to the level of coccyx (Fig. 1). There was an extension of the swelling into the anterior epidural space through the right neural foramina at the level of L4-L5 vertebral body without any significant cord compression or myelopathy. L4 vertebral body and posterior elements were showing hypointensity on T1W and hyperintensity on T2W and STIR sequences. Samples were sent for blood culture and sensitivity before initiating the patient on empirical antibiotics, which came out to be positive for methicillin-sensitive Staphylococcus aureus (MSSA) sensitive to clindamycin, linezolid, tetracycline, and chloramphenicol. A trial of USG-guided aspiration of the psoas abscess was done, but the procedure was abandoned due to irritability of the child. A final diagnosis of pyogenic L4 vertebral body osteomyelitis with septicemia was made. Initially, ceftriaxone and amikacin were started empirically. Later, clindamycin was started as a definite antibiotic after obtaining the blood culture report. The general health of the child as well as blood inflammatory markers started to improve gradually after the initiation of antibiotics (Table 1). A total of 2 weeks of intravenous antibiotics followed by further 4 weeks of oral antibiotics were advised. The patient started improving clinically with complete relief of pain by 2 weeks and the patient resuming his active schooling. Repeat MRI at 3 months showed complete resolution of the lesion in psoas as well as L4 vertebral body (Fig. 1). At 12-month follow-up, the patient has no symptomatology without any affection of any activities.
Discussion
Pyogenic osteomyelitis of long bones is more common than vertebral involvement in children [1]. The rate of vertebral body involvement is 1.2–2.4% in children [5]. This rarity of vertebral body involvement in children is postulated due to adequacy of vascularity of intervertebral space. The most common source of pyogenic vertebral body osteomyelitis in children is either infection of the respiratory tract or soft tissue, whereas in adults, the urinary tract infection is the most common. Urinary tract infection has not yet been documented in children as a source for pyogenic spondylitis. Most cases in children do not have any obvious source of infection, whereas the patient in this report had a bloodstream infection. The typical symptoms of back or neck pain are usually absent in children [1]. Atypical symptoms may include dysphagia, odynophagia, chest pain, abdominal pain, constipation, and urinary symptoms [6]. The average delay in diagnosis of pyogenic vertebral body osteomyelitis in children is median of 5 weeks which is usually due to the atypical presentation [1]. Our patient presented early with symptoms of 10 days duration with complaints of inability to walk, which again is an atypical presentation in the absence of any neurological deficit. ESR is the acute inflammatory marker most consistently elevated in children and it can be used to monitor response to therapy, whereas WBC count is not a very sensitive indicator except in young infants [1]. MRI is the most sensitive and specific modality of investigation for the diagnosis of pyogenic vertebral body osteomyelitis [7]. It is so because of sensitivity of MRI to tissue hydration which helps in early diagnosis compared to other modalities of investigation. For the diagnosis of the microorganism, blood cultures usually suffice because osteomyelitis is usually monomicrobial in children. If blood cultures are negative, tissue diagnosis from the site of lesion is warranted which can be done by guidance of computed tomography imaging [8]. The most common organism, if ever isolated, in such cases is S. aureus which is also noted in the current case. One of the other commoner etiological agents is Salmonella in patients of sickle cell anemia, in whom it is a predisposing factor [9]. Due to several incidences of treatment failure, most authorities now advocate 4-week long parenteral antibiotic therapy although our patient received 2 weeks of parenteral antibiotics followed by 4 weeks of oral therapy [5]. Indications for surgical intervention in such patients include large abscess requiring drainage, spinal cord compression, and increased destruction of vertebral body, leading to collapse [10]. Our patient did not require any surgical intervention and literature suggests that early diagnosis coupled with prolonged antibiotic therapy usually prevents vertebral body destruction along with its sequelae.
Conclusion
Pyogenic vertebral body osteomyelitis is a very rare diagnosis in children which should be considered in patients who have atypical symptoms. MRI is the investigation of choice in such patients and prompt antibiotic therapy should be instituted and they usually heal without any sequelae.
Clinical Message
Pyogenic vertebral osteomyelitis is a rare entity in children with an atypical presentation and symptomatology. MRI is the investigation of choice and antibiotic therapy given for 6 weeks, these heal completely without any sequelae.
References
1. Sapico FL, Montgomerie JZ. Pyogenic vertebral osteomyelitis: Report of nine cases and review of the literature. Rev Infect Dis 1979;1:754-76.
2. Mayer L. An unusual case of infection of the spine. J Bone Joint Surg Am 1925;7:957-68.
3. Gouliouris T, Aliyu SH, Brown NM. Spondylodiscitis: Update on diagnosis and management. J Antimicrob Chemother 2010;65 Suppl 3:iii11-24.
4. Correa GA, Edwards SM, Baker JC. Vertebral osteomyelitis in children. Pediatr Infec Dis J 1993;12:228-33.
5. Dich VQ, Nelson JD, Haltalin KC. Osteomyelitis in infants and children. A review of 163 cases. Am J Dis Child 1975;129:1273-8.
6. Bolivar R, Kohl S, Pickering LK. Vertebral osteomyelitis in children: Report of four cases. Pediatrics 1978;62:549-53.
7. Meyers SP, Wiener SN. Diagnosis of hematogenous pyogenic vertebral osteomyelitis by magnetic resonance imaging. Arch Intern Med 1991;151:683-7.
8. McGahan JP, Dublin AB. Evaluation of spinal infections by plain radiographs, computed tomography, intrathecal metrizamide, and CT-guided biopsy. Diagn Imaging Clin Med 1985;54:11-20.
9. Gardner RV. Salmonella vertebral osteomyelitis and epidural abscess in a child with sickle cell anemia. Pediatr Emerg Care 1985;1:87-9.
10. Patzakis MJ, Rao S, Wilkins J, Moore TM, Harvey PJ. Analysis of 61 cases of vertebral osteomyelitis. Clin Orthop Relat Res 1991;Mar 264:178-83.
 |
 |
 |
| Dr. Sitanshu Barik | Dr. P Venkata Sudhakar | Dr. Shobha S Arora |
| How to Cite This Article: Barik S, Sudhakar PV, Arora1 SS. Pyogenic Vertebral Body Osteomyelitis in a Child: A Case Report. Journal of Orthopaedic Case Reports 2020 Mar-Apr;10(2): 70-72. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




