[box type=”bio”] Learning Point of the Article: [/box]
Intraoperative use of the wake-up test with subsequent Taylor spatial frame fixation is effective and safe for acute correction of limb deformities.
Case Report | Volume 10 | Issue 3 | JOCR May – June 2020 | Page 10-14 | Koji Nozaka, Naohisa Miyakoshi, Hidetomo Saito, Hiroaki Kijima, Yoichi Shimada. DOI: 10.13107/jocr.2020.v10.i03.1726
Authors: Koji Nozaka[1], Naohisa Miyakoshi[1], Hidetomo Saito[1], Hiroaki Kijima[1], Yoichi Shimada[1]
[1]Department of Orthopedic Surgery, Akita University Graduate School of Medicine.
Address of Correspondence:
Dr. Koji Nozaka,
Department of Orthopedic Surgery, Akita University Graduate School of Medicine, Hondo, Akita 010-8543, Japan.
E-mail: kk-nozaka@mue.biglobe.ne.jp
Abstract
Introduction: We herein report a case of idiopathic unilateral external torsion of the tibia treated with Taylor spatial frame (TSF) fixation combined with performance of the wake-up test under anesthesia. The wake-up test is performed toward the end of a surgical procedure after all corrections have been made and hardware has been placed. The patient is slowly awakened and asked to move their feet. After recovery from anesthesia, patients do not remember performing this test.
Case Report: A 17-year-old Japanese male patient complained of a gait disturbance because of external torsion of his foot. The patient was determined to have lateral tibial torsion with a pre-operative foot progression angle of 40.8°. Deformity correction using the TSF was considered to be safe. The tibia was derotated by −34.8°, and the patient had a post-operative foot progression angle of 7.0°. His symptoms and signs improved after derotation osteotomy at the low tibial portion. Two years postoperatively, the patient exhibited no leg length discrepancy or rotation malalignment of the lower extremities as measured both clinically and radiographically.
Conclusion: To the best of our knowledge, there are no reports on the combined use of the TSF and wake-up test for acute correction of idiopathic external torsion of the tibia. Intraoperative use of the wake-up test with subsequent TSF fixation is effective and safe for acute correction of limb deformities.
Keywords: Acute correction, idiopathic external torsion, Taylor spatial frame, wake-up test.
Introduction
Most rotational abnormalities resolve with normal growth. Rotational abnormalities of the lower leg in children have a tendency to improve spontaneously overtime. However, a small percentage of patients will continue to have a residual rotational deformity that may require surgical correction, such as the performance of an osteotomy. Many techniques for lower extremity osteotomy have been described. Severe complications have been reported, however, including late iatrogenic closure of the posterior portion of the tibial physis [1] and peroneal nerve palsy following derotation osteotomy for tibial torsion [2]. The incidence of peroneal nerve palsy is reportedly as high as 22% [3]. In 1969, Schrock also reported the development of peroneal nerve palsy after proximal osteotomy for the treatment of tibial torsion [2]. Compared with one-stage acute surgical correction, fewer complications have been reported when severe deformities were treated by gradual correction using external frames such as the Taylor spatial frame (TSF) (Smith and Nephew, Andover, MA) [4]. Several recent reports on use of the TSF have described good deformity correction outcomes and high reliability and convenience [5]. Although acute corrective osteotomy may be complicated by peroneal nerve palsy, an advantage of this technique is that it does not require callotasis when derotation osteotomy is performed for tibial torsion. Thus, one-stage correction is possible. However, the use of a circular frame has demonstrated the ability to gradually correct rotation, minimizing the incidence of many complications. Another advantage of acute correction is that it takes less time to complete than does gradual correction. In the present case, we performed the wake-up test intraoperatively to prevent peroneal nerve palsy during acute correction of an external tibial rotation deformity before definitive fixation using the TSF. The wake-up test is performed toward the end of a surgical procedure after all corrections have been made and hardware has been placed [6]. The patient is slowly awakened and asked to move their feet. After recovery from anesthesia, patients do not remember performing this test. They also do not appear to be uncomfortable during this procedure. The wake-up test allows the surgeon to definitively determine the patient’s neurologic function immediately after correction. We herein report a case involving the successful treatment of idiopathic unilateral external torsion of the tibia using the TSF with intraoperative performance of the wake-up test.
Case Report
A 17-year-old Japanese male patient exhibited gradual development of an idiopathic tibial torsion deformity (Fig. 1).
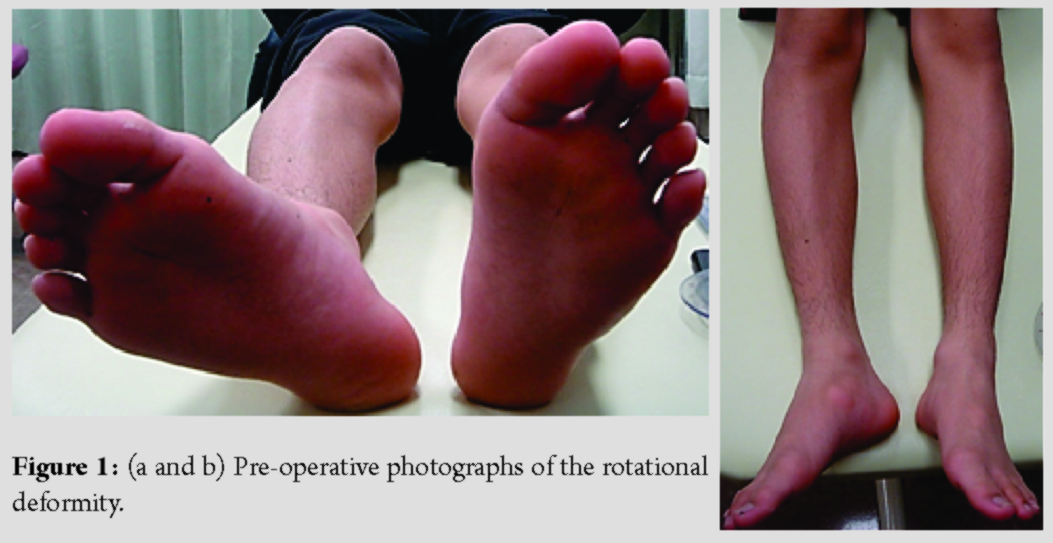
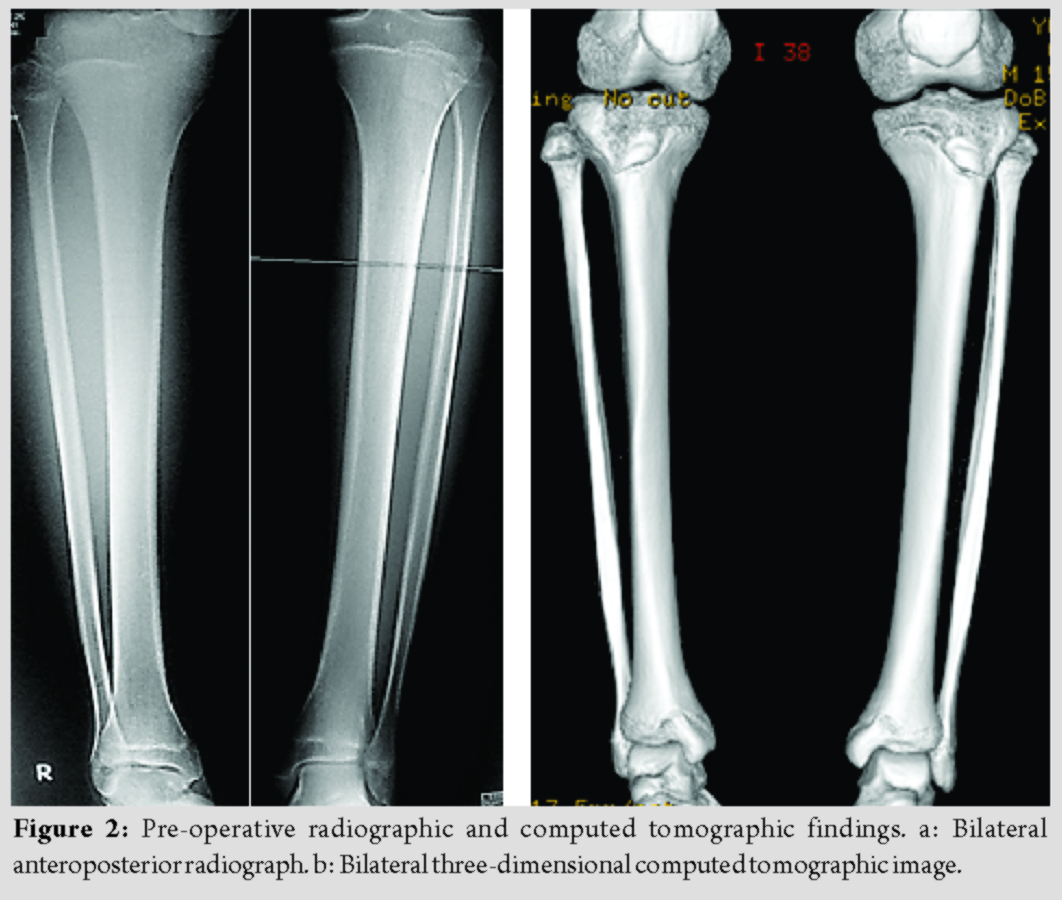
He had no leg length discrepancy at the time of surgery. His distal physis deformity as assessed by simple radiographic examination was characterized as follows: No coronal deformity, no sagittal deformity, and 31.0° external rotation. His rotational deformity as assessed by computed tomography was characterized by a tibial torsion angle of 65.6° on the right and 35.8° on the left (Fig. 2, 3).
We clinically determined the foot progression angle to indicate the amount of rotation before and after surgery.
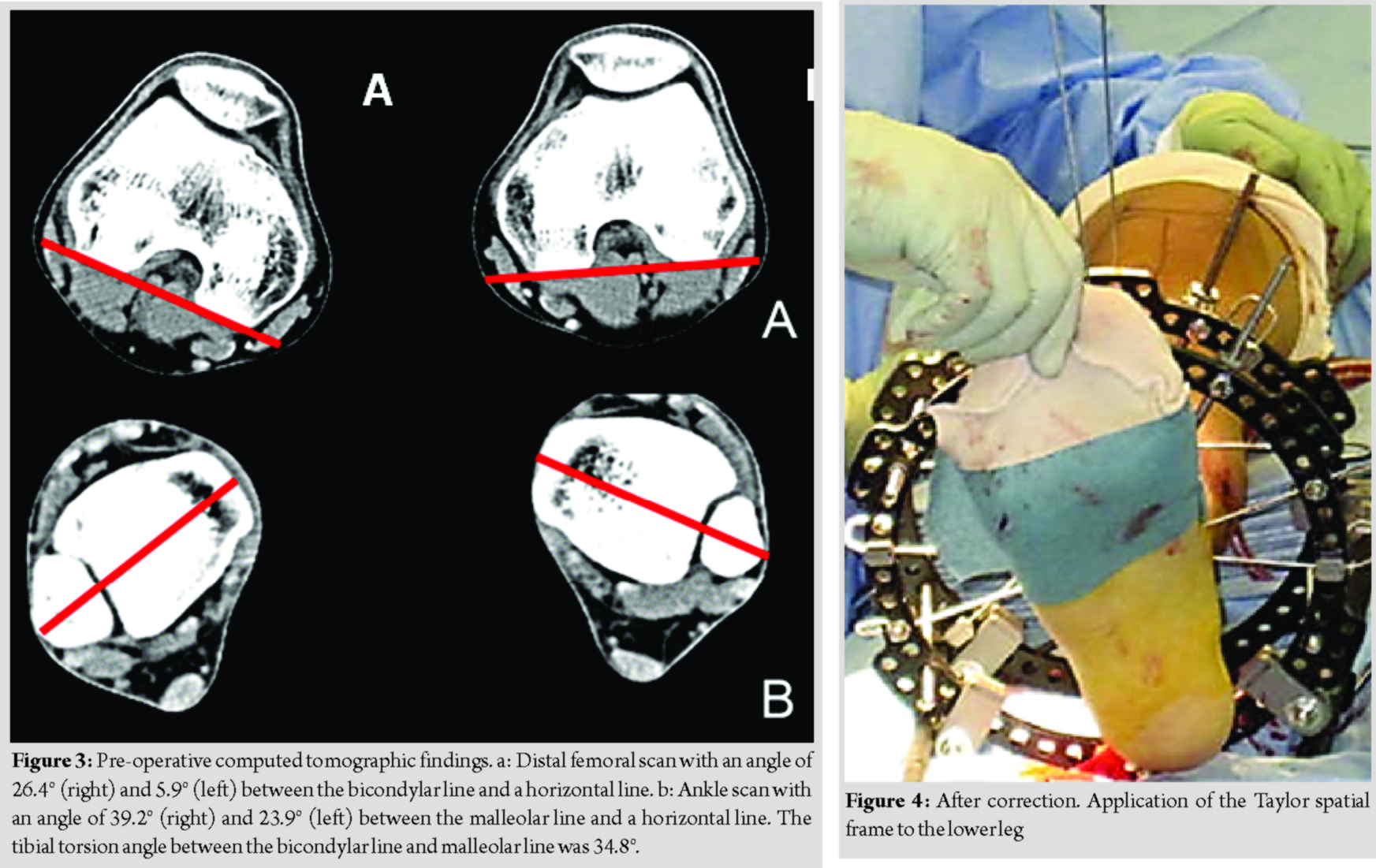
The procedure was performed under tourniquet control. The TSF was applied to the lower leg (Fig. 4). Distal tibial and fibular derotation osteotomies and a percutaneous osteotomy were performed by creating a 2 cm longitudinal incision over the distal lateral fibular shaft, exposing the fibula about 15 cm proximal to the level of the ankle joint. A small osteotome was used to create a transverse osteotomy 2 cm proximal to the physis. The distal tibia was exposed by creating a second 4 cm longitudinal incision 1 cm lateral to the anterior edge of the tibia. To achieve the exact degree of derotation indicated by pre-operative patient analysis, a 0.9 mm K-wire was inserted into the tibia 1 cm distal to the proposed osteotomy site. A second K-wire was inserted just above the proposed osteotomy site, where the bone was more easily penetrated by the K-wire (Fig. 4).This second wire was parallel to the first wire in the sagittal plane, but diverged laterally 31.0° from the original wire in the transverse plane. A transverse osteotomy was then made through the tibia 2 cm proximal to the distal tibial physis using an osteotome. We achieved the exact degree of derotation using two K-wires (Fig. 4). The frame was constructed using two 180 mm full rings and six struts. The proximal ring and second ring were fixed with one half-screw (6.5 mm diameter) and two smooth Ilizarov wires (1.8 mm diameter), the third ring was fixed with two half-screws (6.5 mm diameter) and two smooth Ilizarov wires (1.8 mm diameter), and the distal ring in the foot was fixed with two smooth Ilizarov wires (1.8 mm diameter). The wake-up test was performed toward the end of the surgical procedure after the frame had been constructed using six struts. The level of anesthesia was gradually decreased until the patient became conscious enough to respond to the command “wiggle your toes.” After we had confirmed that the patient could wiggle his toes, the frame was rigidly fixed with the six struts.

The frame fixation was stable, and the growth plate was preserved. Walking with weight-bearing on the operated leg was allowed immediately after surgery. One week later, the patient was able to walk without support. The hospital stay was 14 days long. After discharge, the patient was allowed to walk without crutches and reported a good quality of life with the TSF. Radiographs showed healing of the osteotomy at 76 days postoperatively (Fig. 5).

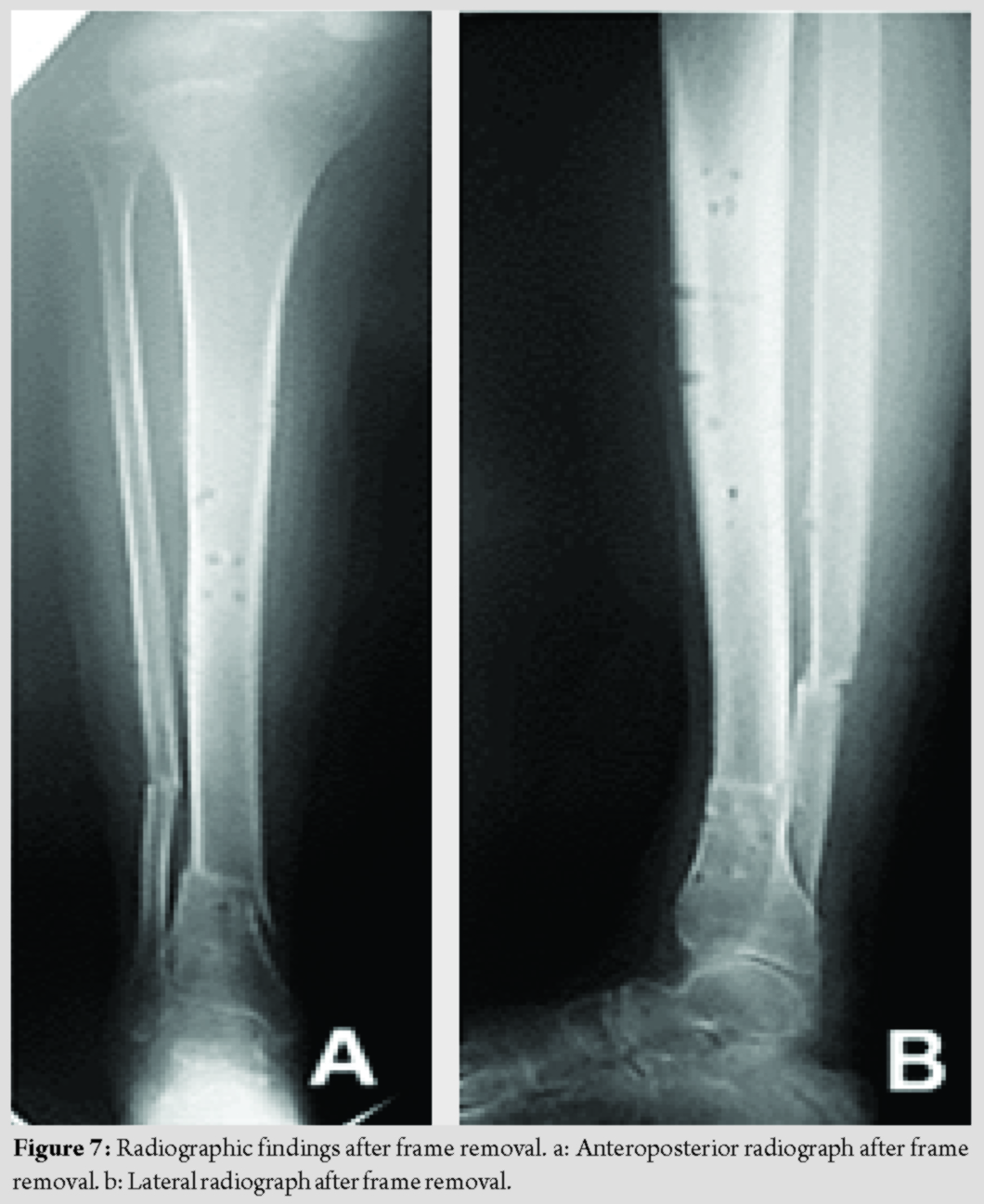
The frame was removed at 86 days postoperatively, and anatomic and functional correction was confirmed (Fig. 6). Two years postoperatively, the patient exhibited no leg length discrepancy or rotation malalignment of the lower extremities as measured both clinically and radiographically (Fig. 7).
The 2-year post-operative follow-up examination revealed preservation of the corrected torsion deformity and improvement in the limping gait.
Discussion
Surgical correction is indicated in fewer than 1% of cases of unilateral torsional deformity of the tibia. Surgical treatment is limited to patients with a progressive symptomatic deformity for which conservative treatment has failed [7]. Spontaneous correction does not occur in some cases, including idiopathic cases. There is a general agreement in the literature on the indications for surgical treatment of idiopathic tibial torsion. These indications include an age of >8 years, the presence of a significant functional or cosmetic deformity, or both [1]. Many methods of fixation derotation after corrective osteotomy have been described, including the use of staples, K-wires, Steinmann pins, and plate fixation. Some articles have reported relatively low rates of iatrogenic deformities after the performance of osteotomies supplemented by internal fixation [8]. However, Manouel and Johnson reported 10% deformity rate after the performance of distal osteotomies fixed with K-wires [9]. McNicol et al. reported 5% incidence of iatrogenic deformities after the performance of distal osteotomies fixed with staples. They suggested that creation of transverse cuts in the tibia and fibula at approximately the same level decreases the risk of iatrogenic varus or valgus deformity at the time of the rotational correction [10]. Lateral rotation can easily lead to unwanted valgus at the osteotomy site and medial varus rotation. Distal osteotomies are associated with fewer complications than are proximal osteotomies. Krengel and Staheli compared complications encountered with proximal and distal site selection. The incidence of peroneal nerve palsy was 5% in the proximal group and 0% in the distal group. Major complications occurred in 13% of patients in the proximal group and 0% of those in the distal group. They recommended using the distal site for derotation osteotomy [8]. Later reports on distally performed osteotomies reported residual deformity rates as high as 39%; however, peroneal nerve palsy was avoided [7-12]. Risk to the peroneal nerve is minimized by performing a distal tibial osteotomy. Therefore, we also performed a distal osteotomy in the present case. The use of K-wires or Steinmann pins for fixation derotation after corrective osteotomy has also been reported. One of the most severe complications involved late iatrogenic closure of the posterior portion of the distal tibial physis after the use of K-wires or Steinmann pins for fixation. Great care must be taken to stay well above the distal tibial physis (minimum of 2 cm) and to limit distal propagation of the elevated portion of the periosteum. In the present case, we performed fixation derotation after corrective osteotomy using the TSF without damaging the distal tibial physis. We also safely performed the intraoperative wake-up test to avoid peroneal nerve palsy. The wake-up test involves reducing the degree of anesthesia before definitive fixation during surgery, allowing the patient to respond to simple commands regarding ankle and toe movement. The patient does not fully awaken and has no post-operative recollection of the test. This type of test is important because the ability to move the feet indicates that the peroneal nerve has remained intact throughout the surgery. We return the frame to the original position using six struts in cases of peroneal nerve palsy development. The frame adjustments are initiated following a 31-day (1º/day) program, resulting in complete correction of the deformity based on the “total residual” program of the TSF.
Conclusion
In this case, we considered that cross-pinning fixation using K-wires would not have been rigid enough because the patient was in very late adolescence. We also considered that plates would need to be removed if peroneal nerve palsy developed. The risk of major complications that may require a secondary surgery was regarded, and deformity correction using the TSF was considered to be safe after reviewing these complications.
Clinical Message
We believe that the use of the TSF with intraoperative performance of the wake-up test allows for safe, accurate correction of unilateral torsional deformity of the tibia in patients in very late adolescence.
References
1. Dodgin DA, De Swart RJ, Stefko RM, Wenger DR, Ko JY. Distal tibial/fibular derotation osteotomy for correction of tibial torsion: Review of technique and results in 63 cases. J Pediatr Orthop 1998;18:95-101.
2. Schrock RD. Peroneal nerve palsy following derotation osteotomies for tibial torsion. Clin Orthop Relat Res 1969;62:172-7.
3. Curley P, Byres K, Brezinova V, Allen M, Chan R, Barnes M. Common peroneal nerve dysfunction after high tibial osteotomy. J Bone Joint Surg Br 1990;72:405-8.
4. Nomura I, Watanabe K, Matsubara H, Nishida H, Shirai T, Tsuchiya H. Correction of a severe poliomyelitic equinocavovarus foot using an adjustable external fixation frame. J Foot Ankle Surg 2014;53:235-8.
5. Nakase T, Ohzono K, Shimizu N, Yoshikawa H. Correction of severe post-traumatic deformities in the distal femur by distraction osteogenesis using Taylor spatial frame: A case report. Arch Orthop Trauma Surg 2006;126:66-9.
6. Ayvaz M, Alanay A, Yazici M, Acaroglu E, Akalan N, Aksoy C. Safety and efficacy of posterior instrumentation for patients with congenital scoliosis and spinal dysraphism. J Pediatr Orthop 2007;27:380-6.
7. Manouel M, Johnson LO. The role of fibular osteotomy in rotational osteotomy of the distal tibia. J Pediatr Orthop 1994;14:611-4.
8. McNicol D, Leong JC, Hsu LC. Supramalleolar derotation osteotomy for lateral tibial torsion and associated equinovarus deformity of the foot. J Bone Joint Surg Br 1983;65:166-70.
9. Krengel WF 3rd, Staheli LT. Tibial rotational osteotomy for idiopathic torsion: A comparison of the proximal and distal osteotomy levels. Clin Orthop Relat Res 1992;283:285-9.
10. Bennett IT, Bunell WP, MacEwen GD. Rotational osteotomy of the distal tibia and fibula. J Pediatr Orthop 1985;5:294-8.
11. Rattey T, Hyndman J. Rotational osteotomies of the leg: Tibia alone versus both tibia and fibula. J Pediatr Orthop 1994;14:615-8.
12. Savva N, Ramesh R, Richards RH. Supramalleolar osteotomy for unilateral tibial torsion. J Pediatr Orthop B 2006;15:190-3.
 |
 |
 |
 |
 |
| Dr. Koji Nozaka | Dr. Naohisa Miyakoshi | Dr. Hidetomo Saito | Dr. Hiroaki Kijima | Dr. Yoichi Shimada |
| How to Cite This Article: Nozaka K, Miyakoshi N, Saito H, Kijima H, Shimada Y. Combined Use of Taylor Spatial Frame and Wake-up Test for Acute Correction of Idiopathic External Torsion of the Tibia: A Case Report. Journal of Orthopaedic Case Reports 2020 May-June;10(3): 10-14. |
[Full Text HTML] [Full Text PDF][XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




