[box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Good functional results can be obtained with timely diagnosis and proper management of atypical OCD associated with OPLL and DISH.
Case Report | Volume 10 | Issue 8 | JOCR November 2020 | Page 11-14 | Bassam H. Alahmadi, Hadeel H. Alalawi, Abdullah H. Alahmadi, Abdulmuhsen N. Alshammari. DOI: 10.13107/jocr.2020.v10.i08.1836
Authors: Bassam H. Alahmadi[1], Hadeel H. Alalawi[1], Abdullah H. Alahmadi[2], Abdulmuhsen N. Alshammari[1]
[1]Department of Orthopedics, King Fahad General Hospital, Almadinah Almunawwarah, Saudi Arabia,
[2]Department of Forensic Medicine, King Fahad General Hospital, Almadinah Almunawwarah, Saudi Arabia.
Address of Correspondence:
Dr. Bassam H. Alahmadi,
Department of Orthopedics, King Fahad General Hospital, Almadinah Almunawwarah, Saudi Arabia.
E-mail: Bhreema88@gmail.com
Abstract
Introduction: Traumatic posterior occipitocervical dissociation (OCD) is a rare injury, and only a few cases have been reported in the literature. The diagnosis can be delayed or even missed because of its uncommon presentation. We present this rare case report and its management to highlight this unusual injury to increase the awareness of the existence of this pathology and prevent delayed diagnosis and treatment.
Case Report: A 76-year-old man was brought to the emergency room with complaints of neck pain. There was a history of trivial trauma before this complaint. The cervical spine images revealed an anterior subluxation of the cervical spine with Jefferson burst fracture involving bilateral fractures of anterior and posterior arches, C5-6 transdiscal fracture, underlying ossification of the posterior longitudinal ligament (OPLL), and diffuse idiopathic skeletal hyperostosis (DISH). He was managed with closed reduction, occipitocervical fourth vertebra fusion (O-C4), and C1, C2 laminectomies with a good outcome.
Conclusion: Traumatic OCD can result from low-energy trauma. We report a rare case of posterior OCD that was associated with Jefferson fracture and predisposing factors, including OPLL and DISH.
Keywords: Occipitocervical dissociation, Jefferson fracture, upper cervical injury, ossification of the posterior longitudinal ligament, diffuse idiopathic skeletal hyperostosis.
Introduction
Traumatic occipitocervical dissociation (OCD) is an uncommon and fatal injury. The most common mechanism of OCD is high-energy trauma. Patients with OCD may present with only severe neck pain without a neurological deficit in about 20% of the cases [1]. It is commonly associated with the upper cervical injuries. Missed OCD diagnosis is usually due to various causes, including low clinical suspicion, multisystem trauma, and difficulty in evaluating the radiographs of the craniocervical junction. Poor neurologic outcomes and rapid neurologic deterioration reported with missed diagnosis due to a high degree of instability of these injuries.
Case Report
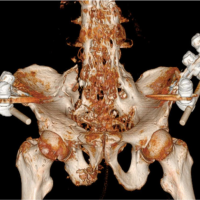
A 76-year-old Sudanese man, farmer, mobilized independently, was brought to the emergency room by his family after a given history of an un-witnessed ground fall at home. He was complaining of neck pain. Cervical collar was applied. His medical, surgical, and allergy history was unremarkable. The patient was conscious and oriented. The physical examination findings revealed left forehead swelling with overlying abrasions and tenderness over the posterior midline neck. He exhibited full strength upper and lower extremities and normal sensation to all extremities with intact perianal sensation. He denied bowel or bladder incontinence. The radiographs of the cervical spine revealed an anterior subluxation of the cervical spine (Fig. 1). Computed tomography (CT) revealed Jefferson burst fracture involving bilateral fractures of anterior and posterior arches, C5-6 transdiscal fracture, underlying ossification of the posterior longitudinal ligament (OPLL), and diffuse idiopathic skeletal hyperostosis (DISH) (Fig. 2). Magnetic resonance imaging (MRI) revealed that the cervicomedullary angle to be 144° (Fig. 3).
Regarding the surgical procedure, the condition, prognosis, and treatment discussed with the patient. The patient consented to and underwent occipitocervical fusion. After initiating awake fiber-optic intubation, Mayfield clamps inserted, and C-Coller kept in place. Then using a Jackson table-turning frame, the patient was rotated into a prone position. The patient was asked to move all upper and lower extremities and found intact. Closed reduction with minimal flexion was made under lateral fluoroscopy. The patient was reassessed for any deficit, and he expressed the same neurological function. Clamps were tightened to the table, and we proceeded for deep anesthesia. Routine posterior midline incision, occipitocervical fourth vertebra fusion (O-C4), and C1, C2 laminectomies were done. A hard C-Collar was applied after skin closure. Postoperatively, the patient was extubated. While he was in the post-anesthesia care unit, he developed airway adverse events in which an emergency re-intubation was required, and he was admitted to the intensive care unit. CT of the cervical spine was done and revealed severe laryngeal edema and airways obstruction (Fig. 4). After 6 days of intubation, otolaryngology service was consulted, and a temporary tracheostomy was performed. CT was obtained post-tracheostomy and showed patency of the airway (Fig. 5). Three weeks later, weaning off the tracheostomy was undertaken. The reason for airway complications was related to difficult intubation, laryngeal edema, and prevertebral hematoma. Post-occipitocervical fusion changes the occipitocervical angle (dOC2A) to 15 degrees (Fig. 5, 6).
The patient was shifted to the ward and stayed there for a further 2 weeks for physical therapy. After that, he exhibited tolerance to oral intake and out of bed mobilization. On discharge, his condition was stable with no neurological deficits, and a C-Collar was planned to be worn for 8 weeks. At 18 months postoperatively, the patient was mobilizing and walking with a cane as before the injury (Fig. 7, 8).
Discussion
Traumatic OCD is a rare and fatal injury. Few cases of traumatic OCD with Jefferson fracture have been reported in the literature [2]. In this report, we present a case of traumatic OCD with Jefferson fracture and underlying OPLL and DISH in the setting of low-energy trauma without neurological involvement. To the best of our knowledge, this is the first case of atypical occipitocervical dislocation to be reported in Saudi Arabia. We aim to highlight such an injury to prompt early diagnosis and allow appropriate treatment of the condition to avoid potential unnecessary morbidities. For instance, our patient presented neurologically intact and showed no deterioration. Furthermore, OCD that resulted from low-energy trauma (ground-level falls) has previously been reported in the literature [1], as in our patient. Spinal CT is more reliable in diagnosis compared to standard radiographs due to the complex osseoligamentous anatomy that is difficult to detect on radiographs. However, MRI is necessary to evaluate the integrity of the ligamentous structures of the craniocervical junction, including the tectorial membrane, occipitocervical joint capsules, alar ligaments, and transverse ligament [3]. Other factors add to the suspicion of OCD, including subarachnoid hemorrhage in the posterior fossa, cranial nerves palsy, and high spinal cord lesions. Trauma victims may have underlying spinal pathologies that predispose them to specific injuries. Two acknowledge pathologies, which lead to alteration of the spine biomechanics are OPLL and diffuse idiopathic skeletal hyperostosis (DISH). In our report, MRI showed underlying OPLL and DISH. OPLL is known to be more common in the elderly Asian population, though it is reported among the African population as well [4, 5]. It can lead to myelopathy and contributes to significant neurologic disabilities, and it is commonly associated with DISH [4, 5]. Following minor trauma, about 34% of patients with cervical spinal cord injuries have OPLL [6]. Most of the patients are not aware of their OPLL before developing neurological deficits [5]. DISH makes the spine more prone to fracture after trivial trauma as it causes ankylosis of the spinal column [7]. In our report, the patient is from east Africa, and it was associated with DISH. The treatment of OCD initially consists of rigid immobilization. As the patient at high risk for neurological deterioration, definitive treatment should be performed as soon as possible. Definitive treatment consists of surgical stabilization with an occipitocervical fusion. In our case, surgical management’s decision in the form of (O-C7) fusion was made, and the patient consented for it. Such a long fusion decision is made because the patient has underlying pathologies (OPLL, DISH). However, intraoperatively, we found that cervical five and cervical six vertebrae are ankylosed posteriorly. Based on that, the decision changed to cervical fourth vertebra fusion (O-C4). A patient has severe spinal canal stenosis secondary to OPLL; based on that, C1 and C2 laminectomies were done. Our patient was on C-collar and maintained his neurological status throughout.
Because of the underlying complex anatomic and biomechanical properties of the occipitocervical complex, management of the airway may be challenging in patients undergoing occipitocervical spine fusions. Difficult intubation, increased levels of vertebrae fused and prolonged duration of surgery are the risk factors associated with post-operative airway adverse events [8]. The rate of re-intubation following posterior cervical spine surgery is 3.9% [8]. Airway obstruction due to pharyngeal swelling, airway edema, vocal cord paralysis, retention of sputum, and aspiration pneumonia is the reasons for re-intubation [8]. In the current patient, re-intubated was due to laryngeal edema and prevertebral hematoma. The difference in the occipitocervical two angles (dOC2A) is correlated with the percentage of changes in the cross-sectional area of the oropharynx [9]. In our case, the changes in the occipitocervical angle (dOC2A) after fusion are 15 degrees (Fig. 6-8). Miyata et al. demonstrated that the airway adverse events are caused by the reduction of the oropharyngeal space, which resulted from the decrease of dOC2A, which was not compensated for by the middle or lower cervical spine [9]. The target post-operative angle should be greater than or equal to a patient’s pre-operative angle. The gray zone for the development of complications is dOC2A between −10 and 0 [9]). Following the occipitocervical fusion, the outcome is overall good. In 86% of the patients, there were no or only mild pain during follow-up [10]. It is reported that the functional disability averaged 42% utilizing the Neck Disability Index NDI, which rated them as “medium disability” [10]. At 18 months follow-up, the patient was asymptomatic, mobilizing, and walking with an assistive device. We obtained written informed consent from the patient to publish this case report and its accompanying images.
Conclusion
Traumatic OCD can result from low-energy trauma. We report a rare case of posterior OCD that was associated with Jefferson fracture and predisposing factors, including OPLL and DISH. Although unique, patients with such an injury can survive without neurological deficits if appropriately treated.
Clinical Message
Although traumatic posterior OCD is a rare and fatal injury, a good outcome can be achieved with surgical management even though if associated with other cervical injuries.
References
1. Tavolaro C, Bransford R, Yerrapragada A, Bellabarba C, Zhou H. Occipitocervical dislocation in low-energy trauma. Case Rep Orthop 2018;2018:3931525.
2. Chang DG, Park JB, Cho KH. Traumatic posterior atlantooccipital dislocation with Jefferson and occipital condyle fractures: A case report. Medicine (Baltimore) 2019;98:e16668.
3. Jung JW, Lee SG, Kim IC, Yoo CJ, Kim WK, Park CW. Traumatic atlanto-occipital dislocation (AOD). Korean J Spine 2012;9:85-91.
4. Inamasu J, Guiot BH, Sachs DC. Ossification of the posterior longitudinal ligament: An update on its biology, epidemiology, and natural history. Neurosurgery 2006;58:1027-39.
5. Adelowo O, Olatunji A. Ossification of the posterior longitudinal ligament in a Nigerian woman. BMJ Case Rep 2011;2011:bcr0220113828.
6. Lee SE, Jahng TA, Kim HJ. Adverse effect of trauma on neurologic recovery for patients with cervical ossification of the posterior longitudinal ligament. Global Spine J 2015;5:124-9.
7. Yunoki M, Kanta T, Suzuki K, Uneda A, Hirashita K, Yoshino K. The importance of recognizing diffuse idiopathic skeletal hyperostosis for neurosurgeons: A review. Neurol Med Chir (Tokyo) 2016;56:510-5.
8. Sheshadri V, Moga R, Manninen P, Goldstein CL, Rampersaud YR, Massicotte EM, et al. Airway adverse events following posterior occipito-cervical spinal fusion. J Clin Neurosci 2017;39:124-9.
9. Miyata M, Neo M, Fujibayashi S, Ito H, Takemoto M, Nakamura T. O-C2 angle as a predictor of dyspnea and/or dysphagia after occipitocervical fusion. Spine (Phila Pa 1976) 2009;34:184-8.
10. Hoffmann MF, Freund K, Schildhauer TA. Outcome of patients with occipitocervical fusion for acute craniocervical instability. Global Spine J 2017;6:36-1582714.
 |
 |
 |
| Dr. Bassam H. Alahmadi | Dr. Abdullah H. Alahmadi | Dr. Abdulmuhsen N. Alshammari |
| How to Cite This Article: Alahmadi BH, Alalawi HH, Alahmadi AH, Alshammari AN. Atypical Occipitocervical Dissociation Associated with Ossification of the Posterior Longitudinal Ligament and Diffuse Idiopathic Skeletal Hyperostosis in Low-Energy Trauma. Journal of Orthopaedic Case Reports 2020 November;10(8):11-14 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com