 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Sacral osteoid Osteoma removal Should Be Very precise due to the proximity of neural tissue. If in centres where advanced techniques like intraoperative CT scans are not available then this technique of preoperative CT localisation has a much better way to assist tumor excision in such areas.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 56-60 | Vivek Bhambhu, Pratik G Patel, Dhanish Mehendiratta, Samir Dalvie. DOI: 10.13107/jocr.2020.v10.i09.1902
Authors: Vivek Bhambhu[1], Pratik G Patel[1], Dhanish Mehendiratta[1], Samir Dalvie[1]
[1]Department of Orthopaedics, PD Hinduja Hospital and Medical Research Center, Veer Savarkar Marg, Mahim. Mumbai. Maharashtra. India.
Address of Correspondence:
Dr. Pratik G Patel,
Room No. 1408, 1st Floor, Hinduja Clinic (Old Building), PD Hinduja Hospital and Medical Research Center, Veer Savarkar Marg, Mahim. Mumbai – 400 016. Maharashtra. India.
E-mail: patel.pratik323@gmail.com
Abstract
Introduction: Osteoid osteoma is a benign bone tumor. It occurs in epiphyseal and metaphyseal regions of long tubular bones of extremities. Around 10% of osteoid osteomas present in spine. In the spine, 2% of cases involve sacrum. Here, we present an atypical case of osteoid osteoma in the sacrum.
Case Report: A 15-year-old boy presented with complaints of low back pain with a 1-year duration, radiating to the left thigh. MRI and CT-scan were suggestive of osteoid osteoma at S1-S2. Pre-operative localization of the tumor was done under CT-guidance under local anesthesia with three spinal localized osteoid osteoma was marked with methylene blue. Dissection of complete osteoid osteoma was done, along with sclerotic margin and sent for histopathological examination which was conformed osteoid osteoma. Post-operative CT-scan showed complete removal of osteoid osteoma. At 1-year follow-up, the patient was asymptomatic with no evidence of recurrence.
Conclusions: The CT-guided pre-operative localization of osteoid osteoma of the sacrum is an interesting treatment option. It decreases operative time with complete and precise excision. It minimizes soft-tissue trauma, and collateral damage allows patients a faster and complete return to normal function.
Keywords: Osteoid osteoma, sacrum, CT-guidance, pre-operative localization.
Introduction
Osteoid osteoma is a benign type of bone tumor firstly described by Jaffe in 1935 [1]. It is composed of a central zone and a peripheral zone. The central zone named nidus is an atypical bone completely enclosed by the peripheral sclerotic reaction zone, which is composed of osteoblasts, osteoclasts, and dilated capillaries [2]. The diameter of osteoid osteoma is 1.5 cm or less. Out of all benign bone tumors, osteoid osteoma constitutes 10% with a male to female ratio of 2–4:1. They are very common, between the ages of 10 and 35 [3]. They mostly occur in long tubular bones of extremities, mostly in the proximal femur. Around 10% of osteoid osteomas present in the vertebral column, mainly in the posterior elements, and out of spine cases sacrum is affected in 2% cases [4]. Here, we present an atypical case of osteoid osteoma in the sacrum, which is completely excised with pre-operative localization of lesion under CT-guidance.
Case Report
A 15-year-old boy presented with complaints of low back pain with a 1-year duration, radiating to the left thigh, exacerbated since 3 months. The pain was worse at night, partially relieved with analgesics. The patient had no previous incidence of trauma or any relevant family or medical history. On physical examination, there was no redness or swelling, but there was tenderness on the left lower gluteal region. The overlying skin was smooth and non-adherent, with no restriction of spine movement. SLR was restricted on the left side due to nerve root irritation and hamstring spasm. The patient had no neurological deficits.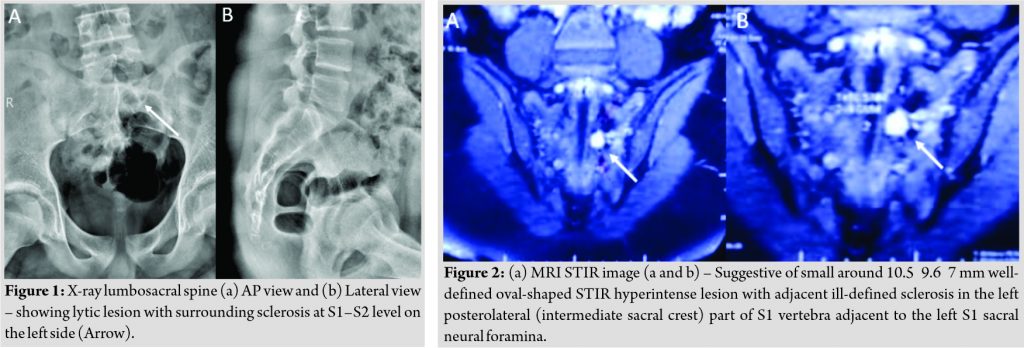
Laboratory data fall within the reference ranges. X-ray lumbosacral spine was showing lytic lesion with surrounding sclerosis at S1–S2 level on the left side (Fig. 1). MRI (Fig. 2a, b) was suggestive of small around 10.5 9.6 7 mm well-defined oval-shaped STIR hyperintense lesion with adjacent ill-defined sclerosis in the left posterolateral (intermediate sacral crest) part of S1 vertebra adjacent to the left S1 sacral neural foramina and CT-scan (Fig. 3a, b) was suggestive of osteoid osteoma at S1–S2 lamina [1.0 0.8 1.0 cm (AP LR SI)] on the left side with minute mineralization inside the lesion, which was consistent with the characteristic ring-shaped radiolucency (nidus) found in osteoid osteoma. Based on these clinical and radiological findings, a diagnosis of osteoid osteoma of the sacrum was finally made. Radiofrequency-ablation was not feasible due to the proximity of the lesion to the neural elements, so pre-operative CT-guidance localization of lesion and excision was planned for the treatment.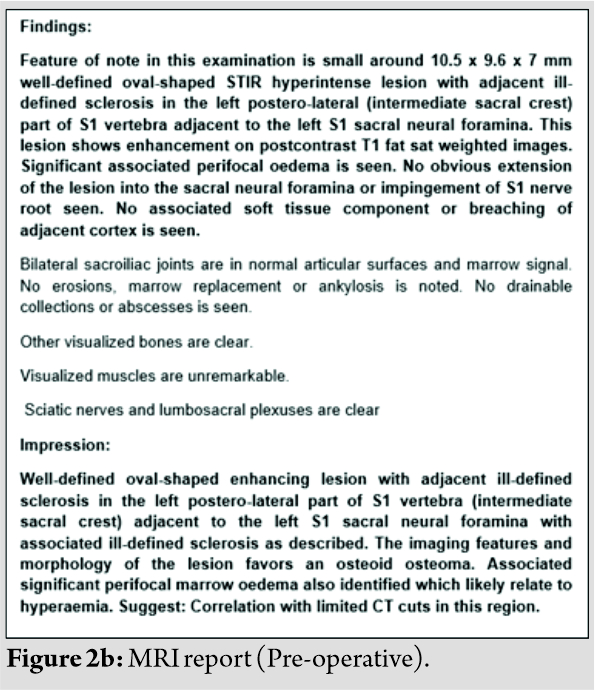
Surgical technique
Pre-operative localization of the tumor was done under CT-guidance under local anesthesia. The patient was in a prone position over the CT (Table. 3 Spinal needles (no. 22) were used for the localization of the tumor. One needle placed above and the second needle placed below the lesion under CT-guidance after the infiltration of the sacral region from local anesthesia (LOX 2%). The third and last needle placed subperiosteally over the lesion (Fig. 4). 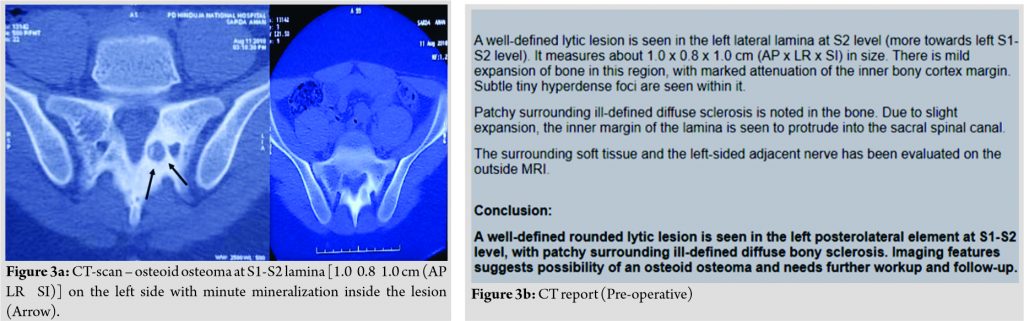 After confirmation of the position of needles, 0.1 cc of methylene blue dye was injected through the central needle. All needles were cut flush to the skin and left in situ. Sterile dressing was applied; the patient was shifted to operation-theater.
After confirmation of the position of needles, 0.1 cc of methylene blue dye was injected through the central needle. All needles were cut flush to the skin and left in situ. Sterile dressing was applied; the patient was shifted to operation-theater.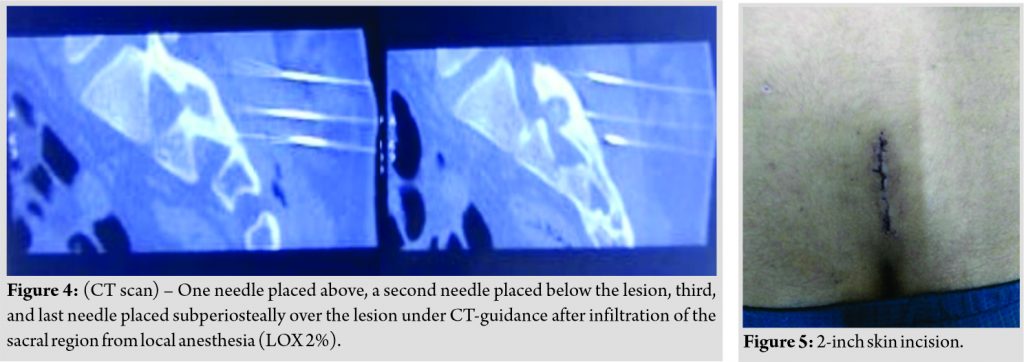
In OT, the patient was in a prone position under general anesthesia. Dissection was done along the needles marking, 2-inch skin incision (Fig. 5) was taken, fascia and muscle dissected out in the line of skin incision using unipolar cautery and needles removed along with dissection.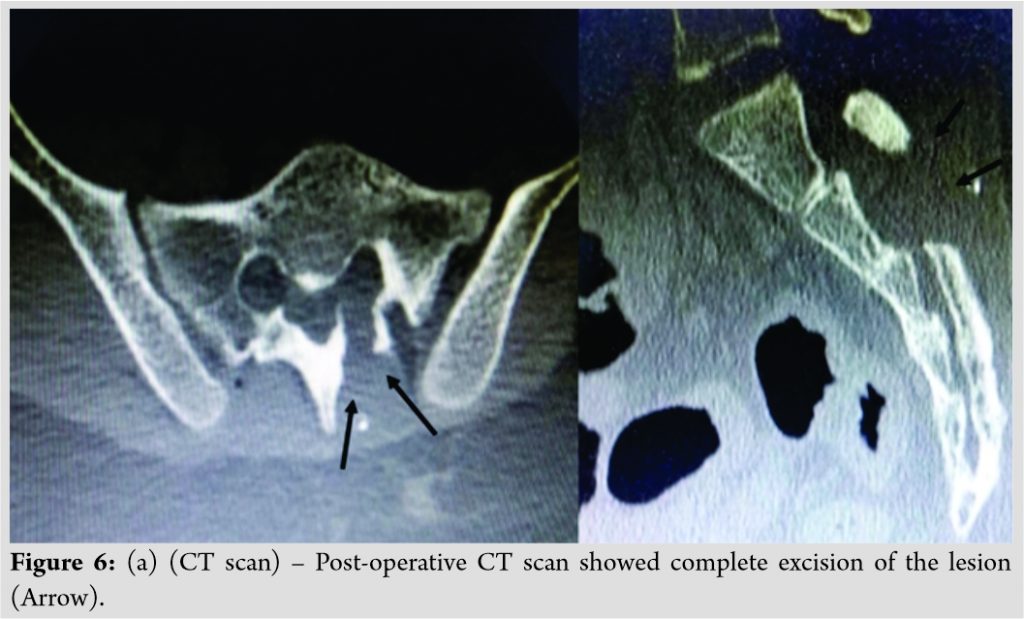 Now localized the osteoid osteoma which was well marked with methylene blue earlier through the central subperiosteal needle. Dissection of complete osteoid osteoma was done, along with sclerotic margin with use of Misonix ultrasonic cutter and microscope. Tissue sent for histopathological examination. The closure was done in layers with absorbable suture applied for the skin.
Now localized the osteoid osteoma which was well marked with methylene blue earlier through the central subperiosteal needle. Dissection of complete osteoid osteoma was done, along with sclerotic margin with use of Misonix ultrasonic cutter and microscope. Tissue sent for histopathological examination. The closure was done in layers with absorbable suture applied for the skin.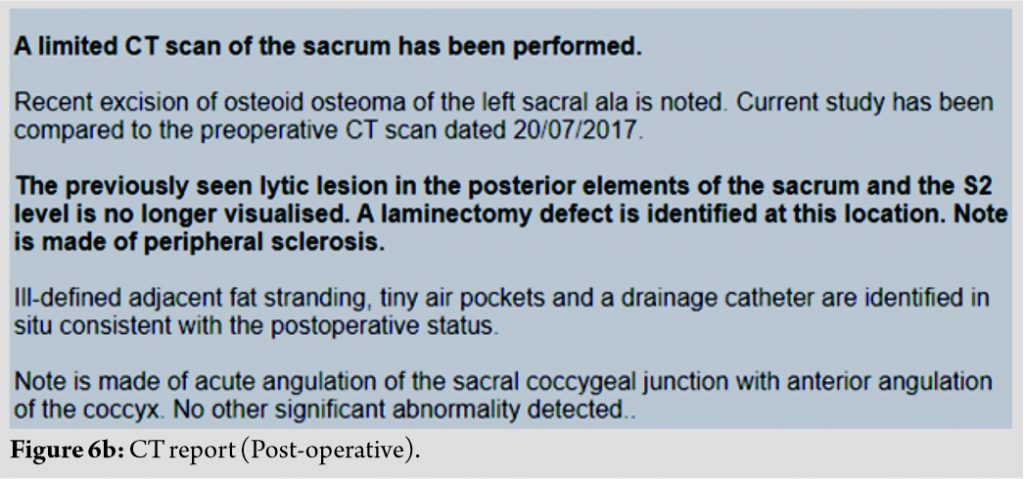
Results
The operation time was 2 h. No surgery-related complications (neurological and infections) were observed. There was no measurable intraoperative blood loss. After surgery, left side gluteal and thigh region pain disappeared. The patient was mobilizing well from 1st post-operative day. The patient only complained of mild surgical pain which was earlier managed with iv agents and later on with oral analgesic agents. The post-operative dressing was done on 2nd day, the wound was healthy. A post-operative CT scan showed complete excision of the lesion (Fig. 6a, b). Histopathological analysis of the biopsy specimens confirmed the diagnosis of osteoid osteoma. Osteoid lined with plump osteoblasts and vascularized connective tissue was found. The patient was discharged on 3rd post-operative day with oral analgesics SOS for surgical site pain. First, follow-up was done 2 weeks after surgery on an OPD basis. The dressing was removed, the wound was healed completely. On clinical examination up to 1-year follow-up, the patient was completely asymptomatic without any complaint of pain.
Discussion
Osteoid osteoma involving the sacrum is extremely rare, and it has also been reported that the diagnosis can be delayed compared with other more common skeletal sites [5]. Plain X-ray, CT, and MRI can be used in determining the exact localization, characterization, other accompanied findings like the close proximity of tumor on the adjacent neural tissues [6]. CT is the best imaging modality to show the presence of a low-attenuation nidus, the lesion’s characteristic finding [7]. For conservative management of osteoid osteoma, side effects of prolonged medication and the lack of histological diagnosis are still a major concern [8]. Hence, surgery is often favored [9]. In addition to conventional open excision, pre-operative CT-guided localization of lesion with minimally invasive surgery, percutaneous excision with large-bore hollow needles and drills, radiofrequency ablation, cryo treatment, ethanol injection, or laser photocoagulation has been used to treat osteoid osteoma [10], [11]. Complete removal or destruction of the nidus is necessary to obtain a successful outcome irrespective of the method of surgery. However, finding the exact location of the nidus is a challenge during operation. In conventional open excision, precise localization of the nidus using a fluoroscope is difficult due to extensive sclerosis around the nidus. That leads to excessive removal of bone around the tumor, leads to jeopardize bone strength, and causes fractures. Several methods, including nuclear scanning, tetracycline fluorescence, tomography, MRI, or CT, have been used to improve the accuracy of localization [12], [13]. Because CT provides a more precise location of the nidus, treating osteoid osteoma with CT-guidance gained popularity in the 1990s [14]. The location of the nidus is demonstrated by CT scan; therefore, nidus removal is possible without sacrificing too much cortical bone and without causing damage to the surrounding uninvolved and important tissues like neurovascular tissues. Cortical defects greatly weaken the bone, especially in torsional stress. It has been shown that small cortical defects with a length less than the diameter of the bone can decrease bone strength up to 60 % [15]. For a larger cortical defect with a length exceeding the bone diameter, the bone strength is decreased by as much as 90 % [15]. In our case, radiofrequency ablation was impossible to apply because the lesion is in direct proximity to the neural tissue. Hence, for this type case, the patient treated with CT-guided pre-operative localization with mini-incision surgery had a smaller bone defect with less chance of damage to neurovascular structure than those treated with conventional open excision without pre-operative localization. The surgical time was shorter for CT-guided pre-operative localization minimal invasive surgery [16]. This is probably due to a clear demonstration of the position of the nidus by CT scan, which lessens the intraoperative time needed to look for the lesion. The rate of recurrence of osteoid osteoma is reported to range from 0% to 25% [17]. The recurrence rate seems lower for the CT-guided group. Without using radiofrequency or photocoagulation, pre-operative CT-guide localization with minimally invasive surgery is more cost-effective than percutaneous procedures using this equipment. Like all types of percutaneous destruction (either by radiofrequency coagulation or laser coagulation), the major drawback of the mini-incision surgery in this study is the difficulty in confirming total excision during the operation. Minimally invasive procedures with pre-operative CT-guided localization of lesion [16] directly result in shorter hospitalization, shorter rehabilitation periods, and decreased overall costs.
Conclusions
The CT-guidance pre-operative localization of osteoid osteoma of sacrum an interesting option for the treatment of these diseases in difficult areas of the lower spine. It decreases operative time with complete and precise excision, minimizing soft-tissue trauma and collateral damage allows patients a faster and complete return to normal function. To the best of our knowledge, this is the first report of sacral spine tumor removal using this approach.
Clinical Message
Pre-operative planning with advanced imaging techniques is mandatory for complete surgical removal of the lesion along with nidus in the case of osteoid-osteoma. CT-guided pre-operative localization with mini-incision surgery had a smaller bone defect with less chance of damage to neurovascular structure than those treated with conventional open excision without pre-operative localization. However, one should carefully explore the area under magnification during the surgery, especially if the nidus is close to neurological structures, to ensure complete removal of the nidus.
References
1. Jaffe HL. Osteoid osteoma: A benign osteoblastic tumor composed of osteoid and atypical bone. Arch Surg 1935;31:709-28.
2. O’Connell JX, Nanthakumar SS, Nielsen GP, Rosenberg AE. Osteoid osteoma: The uniquely innervated bone tumor. Mod Pathol 1998;11:175-80.
3. Greenspan A, Jundt G, Remagen W. Differential Diagnosis in Orthopaedic Oncology. Philadelphia, PA: Lippincott Williams and Wilkins; 2006.
4. Unni KK, Inwards CY. Dahlin’s Bone Tumors: General Aspects and Data on 10,165 Cases. Philadelphia, PA: Lippincott Williams and Wilkins; 2009.
5. Biagini R, Orsini U, Demitri S, Bibiloni J, Ruggieri P, Mercuri M, et al. Osteoid osteoma and osteoblastoma of the sacrum. Orthopedics 2001;24:1061-4.
6. Saccomanni B. Osteoid osteoma and osteoblastoma of the spine: A review of the literature. Curr Rev Musculoskelet Med 2009;2:65-7.
7. Gamba JL, Martinez S, Apple J, Harrelson JM, Nunley JA. Computed tomography of axial skeletal osteoid osteomas. AJR Am J Roentgenol 1984;142:769-72.
8. Kneisl JS, Simon MA. Medical management compared with operative treatment for osteoid-osteoma. J Bone Joint Surg Am 1992;74:179-85.
9. Dahlin DC. Bone Tumor: General Aspects and Data on 11,087 Cases. Philadelphia, PA: Lippincott-Raven; 1996. p. 121-9.
10. Barsa P, Suchomel P, Lukas R, Taller S, Endrych L. Percutaneous CT-guided radiofrequency ablation in spinal osteoid osteoma treatment. Acta Chir Orthop Traumatol Cech 2007;74:401-5.
11. Peyser A, Applbaum Y, Simanovsky N, Safran O, Lamdan R. CT-guided radiofrequency ablation of pediatric osteoid osteoma utilizing a water-cooled tip. Ann Surg Oncol 2009;16:2856-61.
12. Allen SD, Saifuddin A. Imaging of intra-articular osteoid osteoma. Clin Radiol 2003;58:845-52.
13. Rinsky LA, Goris M, Bleck EE, Halpern A, Hirshman P. Intraoperative skeletal scintigraphy for localization of osteoid-osteoma in the spine. Case report. J Bone Joint Surg Am 1980;62:143-4.
14. Voto SJ, Cook AJ, Weiner DS, Ewing JW, Arrington LE. Treatment of osteoid osteoma by computed tomography guided excision in the pediatric patient. J Pediatr Orthop 1990;10:510-3.
15. Nordin M, Frankel VH. Basic Biomechanics of the Musculoskeletal System. 3rd ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2001.
16. Logan PM, Janzen DL, Munk PL, Connell DG. A technique for preoperative localization of osteoid osteoma. Can Assoc Radiol J 1995;46:471-4.
17. Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC, Mankin HJ. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am 1998;80:815-21.
 |
 |
 |
 |
| Dr. Vivek Bhambhu | Dr. Pratik G Patel | Dr. Dhanish Mehendiratta | Dr. Samir Dalvie |
| How to Cite This Article: Bhambhu V, Patel PG, Mehendiratta D, Dalvie S. Complete Surgical Excision with Pre-operative Localization of Lesion Under CT-Guidance of Osteoid Osteoma of the Sacrum – A Case Report. Journal of Orthopaedic Case Reports 2020 December;10(9): 56-60. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




