 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
Melorheostosis is a rare condition. This is a case report that demonstrates clinical and radiological presentation of the disease, management, and review of literature.
Case Report | Volume 10 | Issue 9 | JOCR December 2020 | Page 94-97 | M. Lokesh, Muthumanickam, Sundar Suriya Kumar, Saikrishna Gadde. DOI: 10.13107/jocr.2020.v10.i09.1918
Authors: M. Lokesh[1], Muthumanickam[1], Sundar Suriya Kumar[1], Saikrishna Gadde[2]
[1]Department of Orthopaedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India,
[2]Department of Spine Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
Address of Correspondence:
Dr. Sundar Suriyakumar,
Department of Orthopaedic Surgery, Sri Ramchandra Medical College and Research Institute, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai – 600 116. Tamil Nadu. India.
E-mail: drssundhar @gmail.com
Abstract
Introduction: Melorheostosis is a rare condition affecting the bones and has only been occasionally reported. We herein report a case of melorheostosis affecting left femur and tibia which was diagnosed based on clinical and radiological features and managed with bisphosphonates.
Case Report: A 28-year-old female patient presented with complaints of pain over left knee and thigh for the past 3 months. To evaluate the cause of pain X-ray and magnetic resonance imaging were done, which revealed characteristic candle dripping wax appearance suggestive of melorheostosis. After arriving at the diagnosis patient was started on nonsteroidal anti-inflammatory drugs and pamidronate which provided symptomatic betterment patient has now been followed up for past 1 year and is symptom free.
Conclusion: Melorheostosis is an uncommon cause of a common symptom. Positive clinical and imaging features helped us to arrive at the diagnosis. Proper work up would help in early diagnosis and management. More evidence is needed to illustrate the effectiveness of medical or surgical treatments for patients with this rare diagnosis.
Keywords: Candle dripping wax, melorheostosis, pamidronate.
Introduction
The term melorheostosis is derived from Greek words “melo” which means limb, “theos” which means flow and “ostosis” referring to bone formation. Melorheostosis affects about 0.9 in 1 million people [9]. The exact etiology of the disease is unknown. However, mutations in the MAP2K1 gene are estimated to cause about half of all cases of melorheostosis which are usually somatic. These mutations lead to the production of a version of MEK1 protein kinase that is overactive, which increases RAS/MAPK signaling in bone tissue disrupting the regulation of bone cell proliferation causing abnormal new bone formation [10]. It can occur at any age with no gender predominance. Most of the reported cases are noticed in late childhood to early adulthood. Localized pain can be the usual and sometimes the only symptom manifested. Associated cutaneous manifestations, joint contracture, and limb length discrepancy (LLD) are not uncommon. Diagnosis is usually made based on clinical and radiological features. Melorheostosis in adults has four distinct radiological appearances in the X-ray: The classic dripping wax appearance, osteoma-like lesion, myositis ossificans-(MO-)like lesion, osteopathia striata-like lesion, and mixed picture. In most cases, biopsy is not needed for the diagnosis, but it may be useful in case of uncertain radiographic appearance, certain histologic patterns commonly found in melorheostotic lesions include increased cortical density, woven bone, increased osteoid deposition, and increased vascularity. Melorheostosis is often found to overlap osteopoikilosis and Buschke-Olendroffs Syndrome. Treatment is more oriented to symptomatic relief. Bisphosphonates have been found to aid in the improvement of patient condition and physiotherapy to improve joint mobility [8, 13, 14, 15, 16, 17]. Surgical management involves correction of deformity and release of soft-tissue contracture.
Case Report
A 28-year-old home maker presented to outpatient department at Sri Ramachandra Medical Centre, Chennai, for the left knee pain for past 3 months. Pain was insidious in onset, gradually progressive which aggravates with weight bearing and walking. It is relieved partially with nonsteroidal anti-inflammatory drugs (NSAIDS). On inspection, mild shortening of the left lower limb and calf muscle wasting was noticed (Fig. 1a). On palpation, there is no localized warmth. Bony irregularity and tenderness are present over medial femoral condyle and medial aspect of the proximal tibia. Range of movements was full with moderate pain on terminal flexion (Fig. 1b). Limb measurements showed shortening of 1 cm in the affected limb. Systemic examination is normal. Blood parameters showed elevated alkaline phosphatase.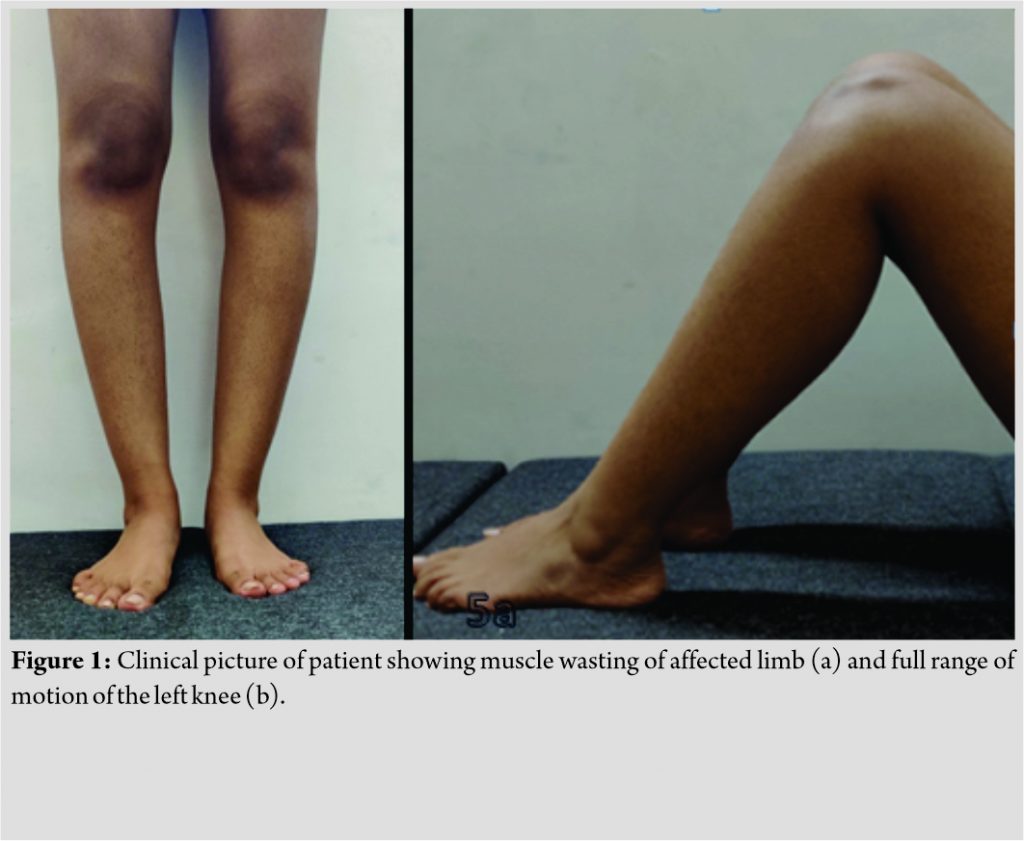
Plain radiography of the effected region showed dense, irregular, and eccentric hyperostosis of both the periosteal and endosteal surfaces of the diaphysis of tibia and characteristic candle dripping wax appearance of medial femoral condyle and proximal tibia (Fig. 2). Similar findings were noticed in the sub trochanteric region of ipsilateral femur (Fig. 3). Magnetic resonance imaging (MRI) of the left thigh (Fig. 4a, b, c) and leg (Fig. 5a, b) was done. MR imaging of thigh and knee with leg revealed decreased signal intensity of the lesion on all pulse sequences. On coronal T1, axial T2 images of the left thigh and leg show fatty infiltration and mild atrophy of the muscles of the thigh and leg compared to right thigh and leg. No marrow edema or intraosseous fluid collections were noted. The muscles showed normal signal intensities. The neurovascular bundle and subcutaneous plain were unremarkable. Based on the above clinicoradiological presentation patient was diagnosed to have melorheostosis.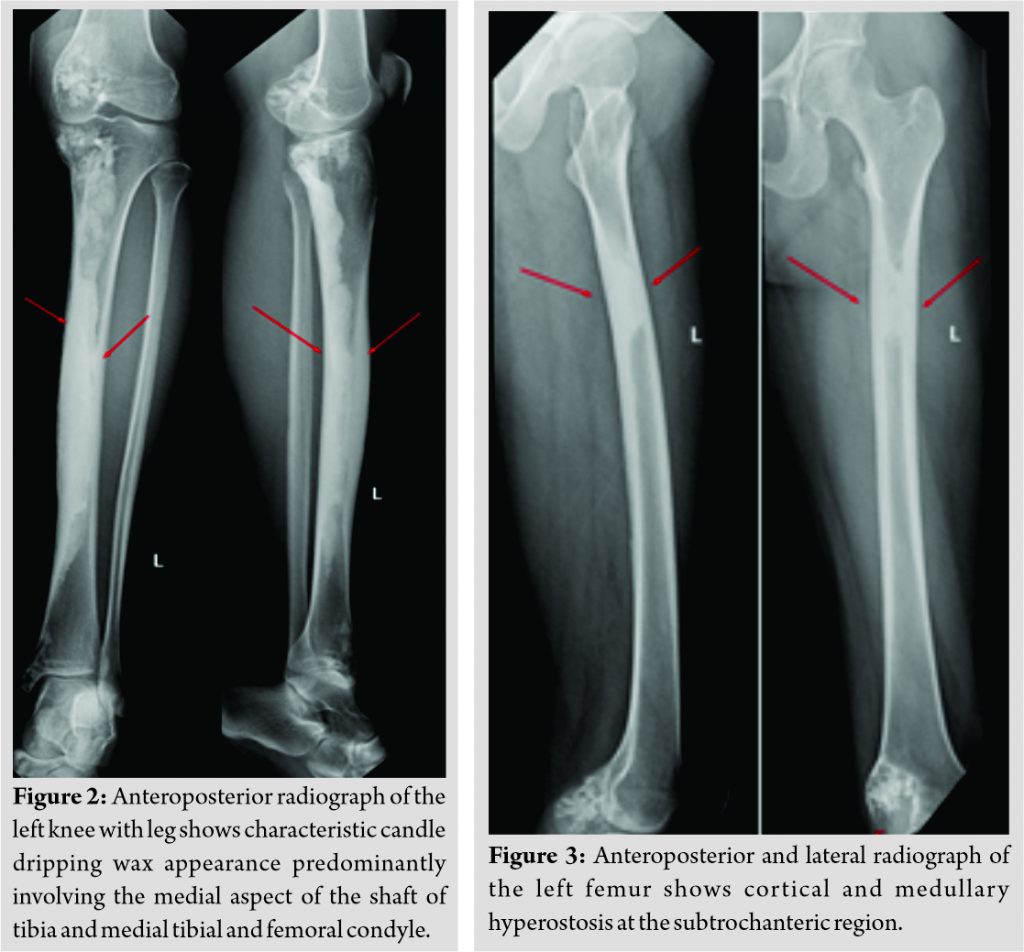
Patient was started on NSAIDS and pamidronate 30 mg/day for 6 days based on evidences. Four weeks after which all bone and joint pains decreased. Serum alkaline phosphatase levels returned to normal levels after 6 weeks. Patient also received physiotherapy in the form of muscle strengthening exercises. Patient has been followed up at 6 months interval for the past 1 years and patient is symptom free.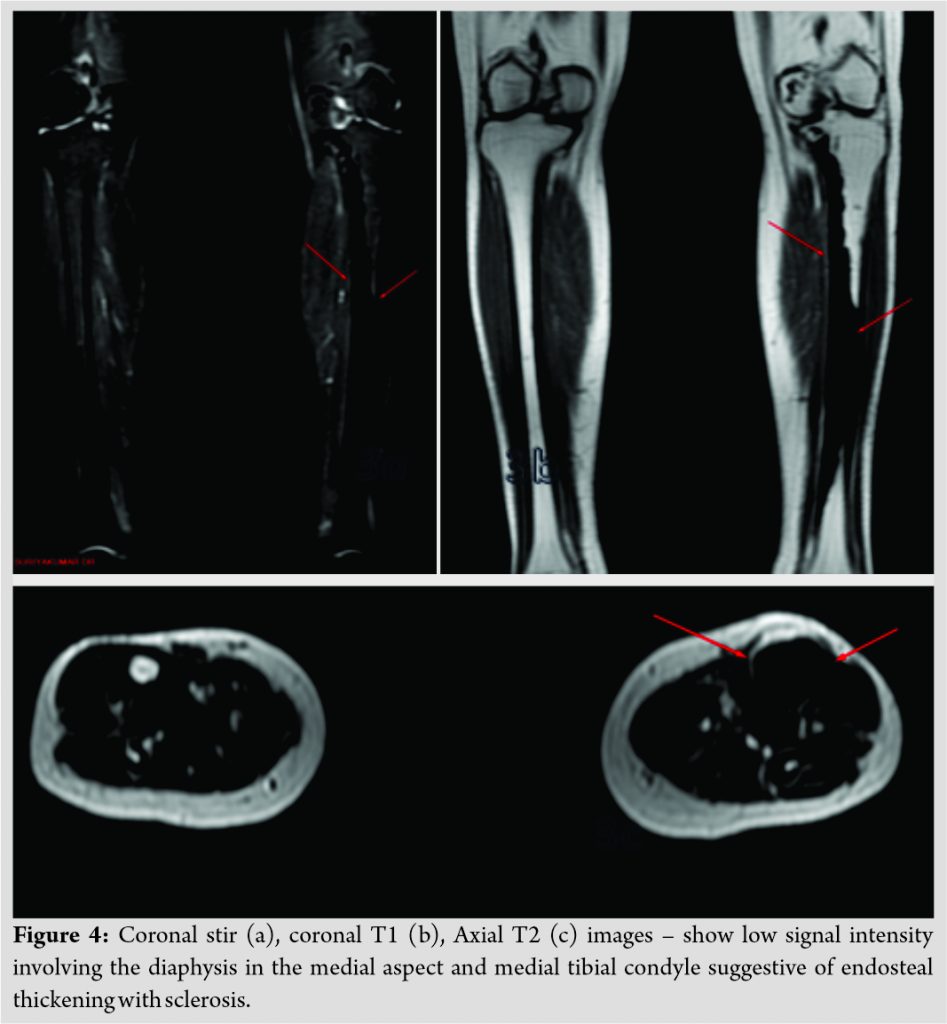
Discussion
Melorheostosis is a rare bone disorder which was first described in 1922 by Leri and Joanny [1]. It is an extremely rare sclerosing bone disease that affects both cortical bone and surrounding soft tissue. Male and female are equally affected and our patient is a female. No hereditary features have been discovered.
Melorheostosis is a disease of the peripheral skeleton, rarely involving the axial skeleton. It may present in a monostotic, polyostotic, or monomelic form. The monomelic variant is the most common presentation of this rare disease [7]. In this patient, femur and proximal tibia is involved. The onset of this rare disease is insidious, the first symptom is usually pain because of the sub periosteal bone formation and in our patient pain was the only complaint. The disease may extend along the affected cortex in a proximal to distal pattern, resembling the pathognomonic “dripping candle wax” appearance on an X-ray [12]. Soft-tissue abnormalities are common, and skin lesions resemble scleroderma [3]. Joint swelling, muscle contractures, and tendon and ligament shortening may cause pain and limitations in the range of motion, LLD can be encountered. LLD was found in 49 of 182 cases from Artner et al. (27%) and our patient had a LLD of 1 cm on measurement [5]. Serum alkaline phosphatase can be elevated [14] similar to our case. More emphasis is to be made on the biochemical investigation of this disease. The diagnosis is usually established before the age of 20 [2], in our patient, the age of diagnosis was 28 years little higher than the average age of diagnosis as reported by Artner et al. which is 24.7 years [5].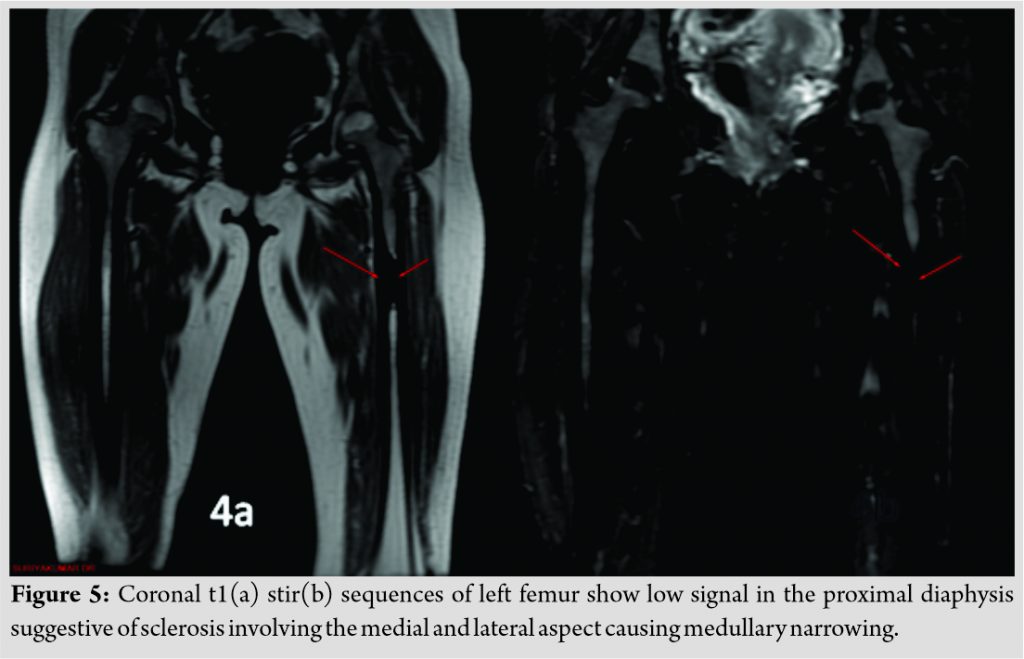
Skin changes may be seen in about 17% of cases and that may include hyperpigmentation of overlying skin and scleroderma [4]. Association of this condition is report with other conditions including neurofibromatosis, tuberous sclerosis, linear scleroderma, tricho-dento-osseous syndrome, rheumatoid arthritis, hypophosphatemic rickets, vascular malformations, and hemangioma [12] none of this features were present in our patient. Campbell (1968) described in his review of 14 cases arthrogryposis and scleroderma as the most common misdiagnosis Buschke-Ollendorff syndrome, another rare disease can include melorheostosis. Buschke-Ollendorff syndrome is characterized by skin growths called connective tissue nevi and areas of increased bone density called osteopoikilosis. A small percentage of affected individuals also has melorheostosis or other bone abnormalities these features were not consistent with our patient [10].
Treatment is mainly symptomatic. Most patients receive non-operative treatment. Bisphosphonate therapy is advocated as effective medical intervention [8, 13, 14, 15, 16, 17]. Potential causes of the bone pain in melorheostosis include increased osteoclastic bone resorption and activation of pain receptors, raised intraosseous pressure, and increased vascularity secondary to hyperosteosis and soft-tissue involvement around joints. Thus, bisphosphonate treatment through a number of mechanisms would be expected to reduce inflammatory bone pain and symptoms in melorheostosis bisphosphonates inhibit osteoclast-mediated bone resorption by direct and indirect actions on osteoblasts and macrophages and bone vascularity. Operative treatment consists of tendon lengthening, excision of hyperostotic bone, osteotomies, sympathectomy, and amputation [4].
The prognosis of a patient is variable and depends on the anatomical location, extension into the soft-tissues, and soft-tissue changes. Melorheostosis does not shorten life span. However, morbidity may be considerable. The disease exhibits a slow, chronic course, with periods of exacerbation and arrest. Recurrence can be expected even after an operative excision [6].
Conclusion
Melorheostosis is an uncommon cause of a common symptom. Positive clinical and radiological features helped us to arrive at the diagnosis. Symptomatic treatment improves the condition of the patients and bisphosphonate therapy compliments it. More evidences and reports are needed to illustrate the effectiveness of medical or surgical treatments for patients.
Clinical Message
Melorheostosis is a rare condition. The conventional radiograph acts as an important aid in diagnosing this condition, they present as characteristic candle dripping wax appearance. MRI helps in identifying adjacent soft-tissue involvement symptomatic treatment and pamidronate are helpful in alleviating pain, physiotheraphy in the form of muscle strengthening exercises and joint range of motion exercises helps in functional betterment of the affected limb.
References
1. Leri A, Joanny J. Une affection non décrite des os hyperostose “en coulée” sur toute la longeur d’un member ou “melorhéostose.” Bull Mem Soc Med Hosp Paris 1922;46:1141-5.
2. Morris JM, Samilson RL, Corely CR. Melorheostosis: Review of the literature and report of an interesting case with a 19-year follow-up. J Bone Joint Surg Am 1963;45:1191-206.
3. Waddell C, Demos TC, Lomasney L, McCarthy R. The case: Your diagnosis? Orthopedics 2005;28:720-5.
4. Waddell C, Demos TC, Lomasney L, McCarthy R. The case: Your diagnosis? Orthopedics 2005;28:720-5. Greenspan A, Azouz EM. Bone dysplasia series: Melorheostosis: Review and update. Can Assoc Radiol J 1999;50:324-30.
5. Artner J, Cakir B, Wernerus D, Reichel H, Nelitz M. Melorheostosis: Current concepts in diagnosis and treatment a review of literature. J Musculoskeletal Res 2012;15:1230002-18.
6. Goldman AB, Schneider R, Huvos AS, Lane J. Case report 778. Melorheostosis presenting as two soft-tissue masses with osseous changes limited to the axial skeleton. Skeletal Radiol 1993;22:206-10.
7. Zeiller SC, Vaccaro AR, Wimberley DW, Albert TJ, Harrop JS, Hilibrand AS. Severe myelopathy resulting from melorheostosis of the cervicothoracic spine: A case report. J Bone Joint Surg Am 2005;87:2759-62.
8. Donath J, Poor G, Kiss C, Fornet B, Genant H. Atypical form of active melorheostosis and its treatment with bisphosphonate. Skeletal Radiol 2002;31:709-13.
9. Jha S, Laucis N, Kim L, Malayeri A, Dasgupta A, Papadakis GZ, et al. CT Analysis of anatomical distribution of melorheostosis challenges the sclerotome hypothesis. Bone 2018;117:31-6.
10. National Organization for Rare Disease. Available from: https://www.rarediseases.org/rare-diseases/melorheostosis.
11. Alothman M, Alkhamees L, Al Subaie AM. Melorheostosis of the leg: A case report. J Radiol Case Rep 2018;12:12-7.
12. Sureka B, Mittal MK, Udhaya KK, Sinha M, Mittal A, Thukral BB. Melorheostosis: Two atypical cases. Indian J Radiol Imaging 2014;24:192-5.
13. Long HT, Li KH, Zhu Y. Case report: Severe Melorheostosis involving the ipsilateral extremities. Clin Orthop Relat Res 2009;467:27382743.
14. Ben Hamida KS, Ksontini I, Rahali H, Mourali S, Fejraoui N, Bouhaouala H, et al. Atypical form of melorheostosis improved by pamidronate. Tunis Med 2009;87:204206.
15. Kawabata H, Tsuyuguchi Y, Kawai H, Yasui N. Melorheostosis of the upper limb: A report of two cases. J Hand Surg 1984;9:871876.
16. Mora R, Guerreschi F, Fedeli A, Riva C. A case of melorheostosis treated with a diphosphonate. Acta Orthop Belg 1986;52:856-61.
17. Bied JC, Malsh C, Meunier P. Melorheostosis in adults. A propos of 2 cases, l of them treated with diphosphonate (EHDP). Rev Rhum Osteoartic 1976;43:193-9.
 |
 |
 |
 |
| Dr. M. Lokesh | Dr. Muthumanickam | Dr. Sundar Suriya Kumar | Dr. Saikrishna Gadde |
| How to Cite This Article: Lokesh M, Muthumanickam, Kumar SS, Gadde S. Dripping Wax Bone Disease – Melorheostosis – A Rare Case Scenario. Journal of Orthopaedic Case Reports 2020 December;10(9): 94-97. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




