 [box type=”bio”] Learning Point of the Article: [/box]
[box type=”bio”] Learning Point of the Article: [/box]
In a septic hip setting, there is a probability of spontaneous slippage of the capital femoral epiphysis. A serial radiological examination is essential to diagnose and treat the slippage early.
Case Report | Volume 11 | Issue 2 | JOCR February 2021 | Page 99-101 | Nilesh Barwar, Ankit Rai . DOI: 10.13107/jocr.2021.v11.i02.2044
Authors: Nilesh Barwar[1], Ankit Rai[1]
[1]Department of Orthopedics, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
Address of Correspondence:
Dr. Nilesh Barwar,
Department of Trauma and Emergency, Orthopedics, All India Institute of Medical Sciences, Jodhpur – 342005, Rajasthan, India.
E-mail: nileshbarwar123@gmail.com
Abstract
Introduction: Delayed slip of the capital femoral epiphysis is a rare entity in the setting of a septic hip.
Case Report: A 13-year-old male presented with an inability to walk and pain around right hip and knee region with fever. On imaging evaluation, a diagnosis of septic hip and knee arthritis was made and both the joints were drained under general anesthesia by anterior approach and an empirical antibiotic therapy was started. On the initial radiograph, there was no sign of slippage of the capital femoral epiphysis. Although the limb was kept in an immobilized position in the 1st week of the surgical debridement, yet it did not prevent the subsequent development of slipped capital femoral epiphysis (SCFE). Open reduction and screw fixation was done to stabilize the slippage. Healing took place with reduction of joint space with some restriction of the hip motion.
Conclusion: SCFE is a disastrous complication in association with septic arthritis of a hip. Routine traction and immobilization may not prevent slippage. Disproportionate amount of pain on weight bearing in a post septic hip should raise the suspicion of SCFE. Prophylactic pinning may be considered in selective cases with antibiotic coverage.
Keywords: Hip sepsis, septic sequelae, slipped capital femoral epiphysis.
Introduction
Slipped capital femoral epiphysis (SCFE) is a devastating disorder in the adolescent age group [1, 2]. If not diagnosed and treated on time, it may cripple the child for the rest of his life. The dreaded complication of an avascular necrosis of femoral head always looms on the slipped epiphysis [3]. There are many risk factors associated with the SCFE such as obesity, adolescent age group, male sex, endocrinopathies, and pelvic irradiation etc [4]. SCFE in the setting of a septic hip in a previously normal hip has been reported in the infantile age group before the advent of antibiotics [5]. When it occurs in the setting of hip sepsis, there is a high likelihood that its diagnosis would be delayed. In addition, the anticipation of slip risk cannot be done. In the infection milieu, management of SCFE is also complicated due to damage to the arterial blood supply and cartilaginous cap of the epiphysis [6]. A case of SCFE is being presented here, which happened in an infection setting of the joint, in spite of immobilization in the early postoperative period.
Case Report
A 13-year-old male presented with pain around right hip and knee region with fever with an inability to walk for 1 week. The hip and knee of the right side were warm with an increased body temperature of 39.9°C. The laboratory parameters showed leukocytosis (total leukocyte count=14,780/µl), raised erythrocyte sedimentation rate (36 mm in the 1st h), and raised C-reactive protein (198.48 mg/l) with differential counts of neutrophil – 79.4%, lymphocyte – 12.6%, monocyte – 6.9%, eosinophil – 0.4%, and platelet – 372,000/microliter. Radiograph and ultrasound showed collection in both the joints (Fig. 1). The hip and knee were drained under general anesthesia and purulent nature of pus was evacuated from both the sites. An empirical antibiotic therapy was started and the entire limb was put on rest with skin traction in a Thomas splint. The culture report showed Staphylococcus aureus (Methicillin-resistant Staphylococcus aureus), sensitive only to clindamycin, cotrimoxazole, and levofloxacin antibiotics. As per sensitivity, an intravenous antibiotic therapy was started. The intensity of fever declined with each passing day and the child started having improved outlook with improvement in his general well-being. On the 5th day of the drainage, a new X-ray was made and it was fine. After some days of tractions, gradual mobilization of the hip and knee was started with a skating board. The wounds were healed. Gradually, he was allowed to bear partial weight on the limb with the help of a walker and discharged to home with continuous oral antibiotics.
After 3 weeks, he again presented with increasing pain in the hip with difficulty in bearing weight on the same limb with formation of a sinus at the drainage site. A fresh radiograph showed SCFE (Fig. 2). The boy was again taken for the surgery and gentle open reduction under general anesthesia and internal fixation was done with three partially threaded cancellous screws along with debridement of the joint (Fig. 3). The limb was put on rest and gradual mobilization with skating again started once pain was in control. The boy was restrained from full weight-bearing until following 2 months with gradual introduction of partial to full weight-bearing. In the subsequent radiographs, the epiphysis healed to the metaphysis with reduction of joint space and some collapse (Fig. 4). Because of decrease in joint space, external rotation was restricted to 20° and flexion was of 0°–100° range. The rest of the hip motions were normal. The knee range of motion was restored to normal. At last follow-up at 18 months, the screws were in position with reduction of hip joint space and some collapse of the epiphysis due to an avascular necrosis. The patient was fully ambulatory with occasional pain; hence, the implant was kept in situ till further necessity.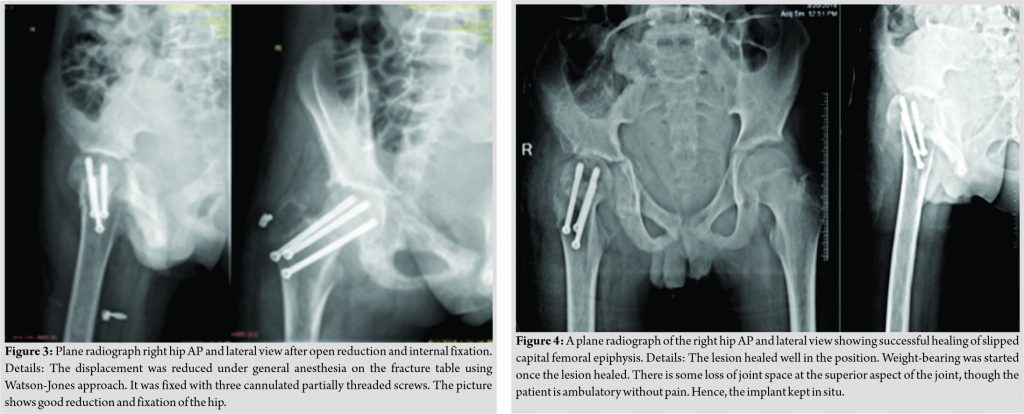
Discussion
SCFE is a disorder of school-going age group. Many etiologies have been incriminated for the SCFE. Some of them are endocrine abnormalities, increased body weight, and steeper orientation of proximal femoral physis [1, 2, 4, 7]. Epiphysiolysis, although it is a potential complication of a septic hip, yet it is comparatively a rare entity [8]. With prompt medical and surgical management of a septic hip, there is an overall decline in the complication rate; cases of SCFE associated with septic hip have been reported mainly in pre-antibiotic era [5]. In our case, an adolescent patient presented a week after developing symptoms with multifocal joint involvement. The culture showed S. aureus. The patient developed SCFE of affected hip after 3 weeks of initial treatment. Except for an adolescent age group, no other factors such as obesity (body mass index 19.1 kg/m2), endocrine abnormalities, or trauma could be incriminated in our case. As the patient was normal and walking before the incidence, it seems the infective process in the joint may have triggered the epiphyseal separation. Infective processes and inflammatory cascade may weaken the junction of epiphysis and metaphysis and lead to epiphyseal slip, which is the probable explanation in the present case. Similar observations were made in a study by Marx and Wright, where an adolescent patient developed SCFE after delayed treatment of septic hip [9]. Diagnosis of the SCFE is delayed because of coexisting infection. Furthermore, prediction of slip cannot be made in an infected milieu. The present case report highlights that even immobilization of a hip in neutral position may not prevent the slippage. It is advisable to have a good quality radiograph of the septic hip before allowing bearing body weight, to discern any subtle signs of physical separation. Although the literature does not support the prophylactic fixation of the epiphysis in the setting of infection, it might be worthwhile to do so in suspected cases. Subsequently, such a fixation can be removed once the infection is subsided. Furthermore, the more severe the sepsis, greater the accumulation of pus in the joint with inflammatory cytokines and proteolytic enzymes, the higher could be the chances of slippage in association with weight-bearing. The authors think that in such cases with delayed presentation, frank abscess in the joint and specifically multifocal involvement of joints may have triggered the slippage. Debridement and pin fixation are advisable treatment once the slippage occurs, but an avascular necrosis of the hip and loss of range of motion are the expected complications even with the best of treatment.
Conclusion
SCFE is a disastrous complication in association with septic arthritis of the hip. Routine traction and immobilization may not prevent slippage. A regular periodic radiographic examination is needed for an early diagnosis. A disproportionate amount of pain in a post septic hip on weight-bearing should raise the suspicion of SCFE. Prophylactic pinnings may be considered in selective cases where intra-articular abscess is voluminous with considerable duration of disease.
Clinical Message
Traditionally, sepsis of a hip promotes dislocation and hence traction and immobilization is recommended, however it may not prevent an SCFE. A high index of suspicion should be kept in such cases. Periodical radiographic examination and being watchful for extreme pain on bearing weight after septic hip are important tools to reveal the underlying SCFE, and further investigations are warranted to make a timely diagnosis and swift management.
References
1. Fishkin Z, Armstrong DG, Shah H, Patra A, Mihalko WM. Proximal femoral physis shear in slipped capital femoral epiphysis–a finite element study. J Pediatr Orthop 2006;26:291-4.
2. Litchman HM, Duffy J. Slipped capital femoral epiphysis: Factors affecting shear forces on the epiphyseal plate. J Pediatr Orthop 1984;4:745-8.
3. Loder RT. What is the cause of avascular necrosis in unstable slipped capital femoral epiphysis and what can be done to lower the rate? J Pediatr Orthop 2013;33 Suppl 1:S88-91.
4. Castillo C, Mendez M. Slipped capital femoral epiphysis: A review for pediatricians. Pediatr Ann 2018;47:e377-80.
5. Green W. Osteomyelitis in infancy. J Am Med Assoc 1935;105:1835-9.
6. Eyre-Brook A. Septic arthritis of the hip and osteomyelitis of the upper end of the femur in infants. J Bone Joint Surg Br 1960;42-B:11-20.
7. Bhatia NN, Pirpiris M, Otsuka NY. Body mass index in patients with slipped capital femoral epiphysis. J Pediatr Orthop 2006;26:197-9.
8. Monga P, Jagannath CS, Verma R, Sharma VK. Complete slipping of the capital femoral epiphysis after hematogenous osteomyelitis. Can J Surg 2003;46:59-60.
9. Marx RG, Wright JG. Slipped capital femoral epiphysis after septic arthritis of the hip in an adolescent: Report of a case. Can J Surg 1999;42:145-8.
 |
 |
| Dr. Nilesh Barwar | Dr. Ankit Rai |
| How to Cite This Article: Barwar N, Rai A. Delayed Slipped Capital Femoral Epiphysis Following Septic Arthritis of Hip: A Case Report. Journal of Orthopaedic Case Reports 2021 February;11(2): 99-101. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




