The management of bilateral asymmetric hip dislocation with posterior wall fracture is early reduction of hip dislocation and anatomical fracture fixation as early as possible so as to restore the normal joint biomechanics, prevent femoral head osteonecrosis and provide good functional outcome.
Dr. Pinaki Das,
B 1512 Sector 6 CDA, Abhinav Bidanasi, Markat Nagar, Cuttack – 753 014. Odisha, India.,
E-mail: docpinakidas@outlook.com
Introduction: Asymmetric bilateral hip dislocations are very rarely reported in literature. We report a unique case of asymmetric traumatic bilateral hip dislocation in a 34-year-old male, describing the management and post-operative complications.
Case Report:A 34-year-old truck driver sustained injury to both his hips in a head on collision between two trucks while seated in the passenger seat. There was a delay in presentation at our institution as he was referred after 17 h of the trauma. After evaluation, he underwent closed reduction of both hips under intravenous anesthesia on the same day. The post-reduction assessment revealed a left-sided posterior wall fracture which was suspected due to the instability after reduction. Fixation of the fracture was done using two spring plates. The patient was followed up throughout his rehabilitation and thereafter when he resumed his occupation. Six months after the incident, the patient had pain-free, full range of motion of both hips. Three years after the surgery radiological investigations revealed changes suggestive of early avascular necrosis (AVN), however, the patient did not have any functional restriction.
Conclusion: This is a case of bilateral asymmetric hip dislocation with left side posterior wall fracture. It is important to reduce the hip and also address the fracture as early as possible to prevent AVN.
Keywords: Bilateral asymmetric hip dislocation, posterior wall fracture, Kocher-Langenbeck, avascular necrosis.
Bilateral asymmetrical traumatic hip dislocation is one of the most rarely reported injury patterns that are usually caused by very high-energy trauma. It represents 1.35% of all the hip dislocations reported [1]. In the literature, asymmetrical hip dislocations constitute only 0.01–0.02 of all the joint dislocations [2]. Bilateral hip dislocations are usually associated with acetabular or proximal femur fractures [3]. As the hip joint has an intrinsic stability, dislocations of both the joints are usually rare [4]. The stability of the hip joint is determined by the depth of the acetabulum, thickness of the labrum, capsular integrity, and strong muscles working concurrently. Simultaneously, there may be femoral, obturator, or sciatic nerve injury. Post-traumatic osteoarthritis, avascular necrosis (AVN) of femoral head, and heterotopic ossification are some of the most common complications usually seen in this scenario [5]. We here present a case of bilateral hip dislocation, presented to us 17 h after trauma. Bilateral closed reduction under sedation was done in the operating theatre on the day of admission followed by open reduction and internal fixation of the left-sided posterior wall fracture. The patients’ outcome through 3 years of follow-up was documented.
A 34-year-old man presented to our institution 17 h after sustaining injury to both the hips in a road traffic accident. The patient was sitting in the passenger seat of a loaded truck. It had a head-on-collision with another truck. He was not under the influence of any drugs or alcohol during the accident. As per history, at the time of the collision, he was seated in the passenger seat with his right hip flexed and the right foot resting on the dashboard of the truck and the left leg abutting the dashboard. The delay in the presentation was due to the patient being attended at a primary care center and subsequently referred to our center for further management. On initial examination, he was hemodynamically stable with a Glasgow Coma Scale of 15. There was no open injury of lower limb but multiple small abrasions all over the body were present. There was no associated injury to the chest or abdomen. The initial management was done as per the Advanced Trauma Life Support (ATLS) protocol. The right lower limb had an attitude of flexion, abduction, and external rotation, the left limb was in flexion, internal rotation, and adduction. Distal to the level of injury the motor function, sensation, and pulse were normal. The patient was then subjected to standard trauma series X-rays. The pelvis X-ray showed bilateral hip dislocation – left-sided posterior and right-sided anterior (obturator type) (Fig. 1).
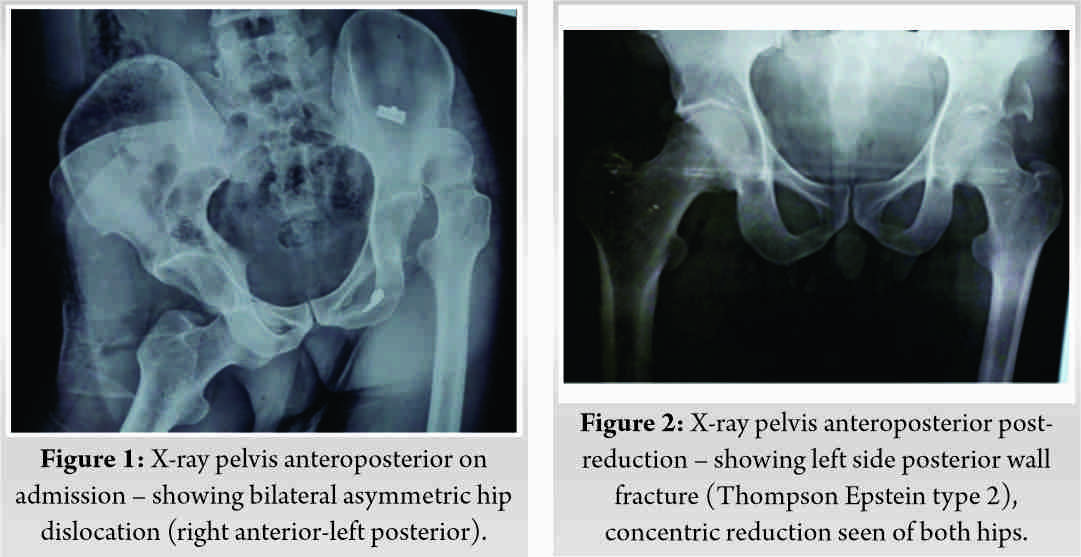
Under total intravenous anesthesia and fluoroscopy guidance, closed reduction was attempted with the patient supine on the operating table. Posterior dislocation was reduced with Allis maneuver and anterior dislocation was reduced using a similar maneuver, but with the application of longitudinal traction and the assistant applying lateral traction on the proximal thigh with a towel. There was no change in the distal neurovascular status. Both reductions were confirmed under fluoroscopy. The right hip which had dislocated anteriorly was found to be stable. The left hip, which had a posterior dislocation posteriorly, was found to subluxate on application of moderate posteriorly directed force in flexed position. Fracture of the posterior wall was suspected on the left side with fluoroscopy which was not discernible in the pre-operative radiograph. The patient was then subjected to distal femur skeletal traction bilaterally with 3 mm Steinman pin with a weight of 15 pounds.
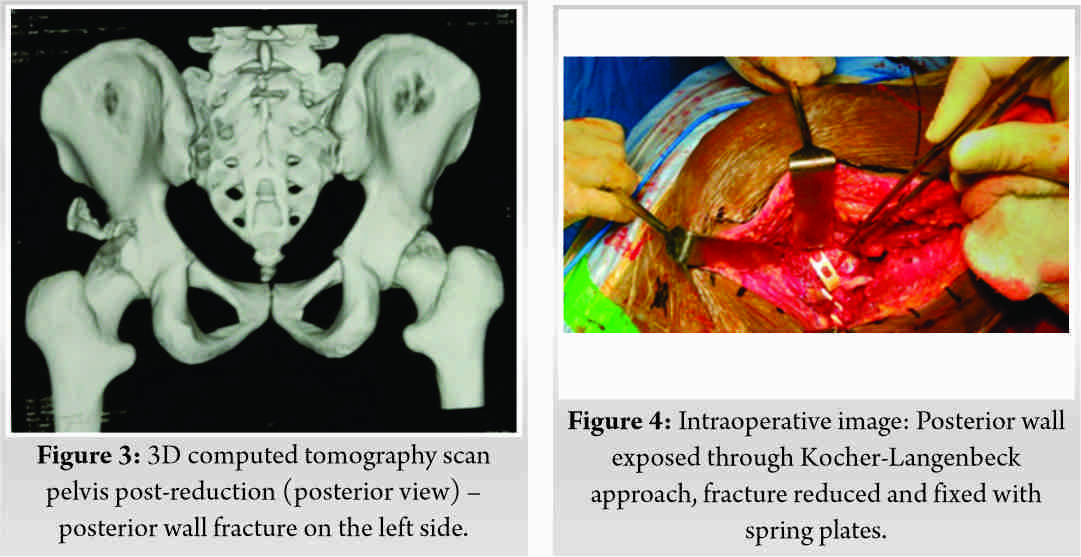
He underwent post-reduction radiograph and computed tomography (CT) scan of bilateral hips to detect any occult or impacted fractures and to plan further management (Fig. 2, 3). He was diagnosed with Thompson Epstein fracture type 2 with posterior wall fragment on the left side.
The patient was subjected to regular pre-anesthetic workup and underwent surgery on the 14th day following trauma under general anesthesia. The left hip joint was exposed using the Kocher-Langenbeck approach. Piriformis and external rotators were found to be intact. Stay sutures were applied before their division. The intra-articular osteochondral fragments that interposed between the articular surfaces were removed. The fracture fragments were reduced and provisionally fixed with K-wires. Fixation was done with two spring plates (two holes and three holes). After application of these two spring plates, dynamic stress test was done and the fracture was found to be stable (Fig. 4)
.
After confirming the stability of the fracture to avoid extensive soft-tissue dissection, we decided not put at any secondary stabilizing plate in this case. Wound was closed after achieving hemostasis over a suction drain. Post-operative X-ray is shown in (Fig. 5).
The post-operative period was uneventful. Antibiotics were given up to 3 days post-surgery. The patient was discharged after 5 days. Intermittent left hip passive range of motion (ROM) exercises were started on the 5th post-operative day as tolerated by the patient, while maintaining the traction. Stitch removal was done 14 days after surgery. Bilateral skeletal traction pins were removed after 3 weeks and the patient was started on the right hip ROM exercises. The patient was started on partial weight-bearing with walker from 6 weeks after trauma. Complete weight-bearing was allowed 14 weeks after surgery. Serial radiographs were obtained at every visit till union was evident.
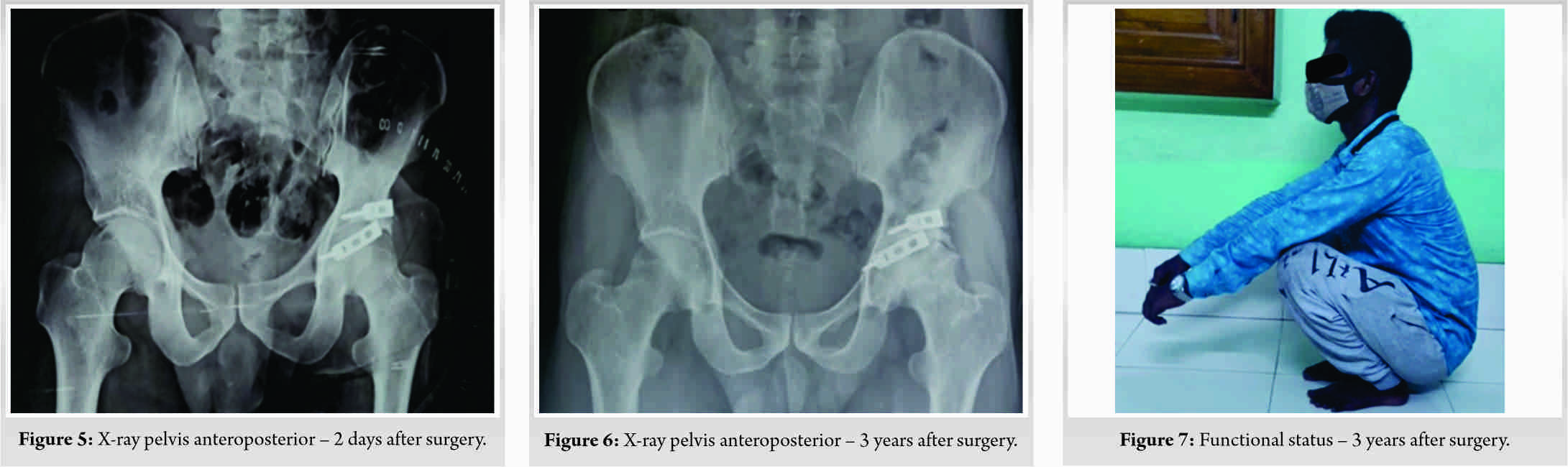
At 6 months post-surgery, the patient had excellent and pain-free ROM. He was able to squat without difficulty and commute on a bicycle. He had no complaints resuming his occupation as a truck driver. At 3 years after the surgery, radiologically, there appeared to be some deformity of the left femoral head with early AVN changes (Fig. 6). The patient did not report any restriction in performing his activities or daily living or occupation (Fig. 7).
Due to the initial delay in diagnosis and treatment of the patient, the patient had been counseled about the high probability of complications. The patient is planned for strict monitoring every 3 months to detect any further deterioration.
Hip dislocation and acetabular fractures are typically the result of high-energy trauma. The most common mechanism of injury is motor vehicle accident, during a severe deceleration force to a flexed knee [6]. Dashboard injuries are usually responsible for such peculiar pattern of bilateral dislocation [7]. In this case, the right hip was in an abducted and flexed position resulting in anterior dislocation. The left hip suffered a classical dashboard injury leading to a posterior dislocation. The typical “windswept deformity” of the legs at the time of impact has been considered an attributing factor for the bilateral asymmetrical dislocation [8].
Buckwalter et al. reviewed 104 cases with asymmetric bilateral hip dislocations, reported associated fractures in 44% of patients. Fracture of the acetabulum of the posteriorly dislocated hip constituted 75% of those fractures [2]. There was an associated posterior wall fracture in the posteriorly dislocated hip in this case. In the initial evaluation, the patients should be screened with trauma series X-rays and astute clinical examination. Any life-threatening injuries should be addressed first according to ATLS principles. Posterior hip dislocations with concomitant posterior wall fractures are usually missed in the preliminary radiological study. Prompt post-reduction evaluation and recognition of the pattern of injury helps in early and appropriate reconstruction of the hip joint [9]. CT if performed before attempting the closed reduction may result in delay and is unnecessary for the initial management. However, the planning of definitive surgery for complex acetabular fractures with intra-articular or impacted fragments relies on the detailed CT analysis [10].
Prompt diagnosis and early reduction of hip dislocation is of paramount importance to avoid the dreaded complication of AVN. Reduction within 6 h is associated with best prognosis in the literature [1]. Even if early reduction is attempted, damage to the blood supply of the femoral head, traumatic ligamentum teres injury, and ischemia during the dislocation can also lead to AVN and post-traumatic arthritis [11]. In our case, there was a delay in presentation leading to late primary intervention. Hence, the risk of AVN was high. Post-traumatic arthritis is a frequent complaint found in 16% of uncomplicated hip dislocations and in 88% of the cases with fractures [12].
Asymmetrical bilateral hip dislocation is a rare injury pattern documented here. Prompt diagnosis, high suspicion for other commonly associated injuries, immediate reduction of the dislocation, and stringent adherence to follow-up are the key determinants of an excellent outcome.
Any joint dislocation necessitates prompt reduction to avoid future complications. Hip dislocations when not reduced in a timely manner lead to AVN in most cases as seen here.
References
- 1.Phillips AM, Konchwalla A. The pathologic features and mechanism of traumatic dislocation of the hip. Clin Orthop Relat Res 2000;377:7-10. [Google Scholar]
- 2.Buckwalter J, Westerlind B, Karam M. Asymmetric bilateral hip dislocations: A Case report and historical review of the literature. Iowa Orthop J 2015;35:70-91. [Google Scholar]
- 3.Sener M, Sener U, Yildiz M, Baki C. Bilateral traumatic hip dislocation with bilateral sciatic nerve injury. Arch Orthop Trauma Surg 1997;116:225-6. [Google Scholar]
- 4.Azar F, Beaty J. Fractures and dislocations in adults. In: Campbell’s Operative Orthopaedics. 14th ed., Ch. 55. Philadelphia, PA: Elsevier; 2021. p. 2943. [Google Scholar]
- 5.Shannak AO. Bilateral traumatic dislocation of the hips with ipsilateral femoral fracture. Clin Orthop Relat Res 1987;215:126-9. [Google Scholar]
- 6.Onyemaechi NO, Eyichukwu GO. Traumatic hip dislocation at a regional trauma centre in Nigeria. Niger J Med 2011;20:124-30. [Google Scholar]
- 7.Epstein HC, Wiss DA, Cozen L. Posterior fracture-dislocation of the hip with fracture of the femoral head. Clin Orthop 1985;201:9-17. [Google Scholar]
- 8.Lam F, Walczak J, Franklin A. Traumatic asymmetrical bilateral hip dislocation in an adult. Emerg Med J 2001;18:506-7. [Google Scholar]
- 9.Adam P, Labbe JL, Alberge Y, Austry P, Delcroix P, Ficat RP. The role of computed tomography in the assessment and treatment of acetabular fractures. Clin Radiol 1985;36:13-8. [Google Scholar]
- 10.Brooks RA, Ribbans WJ. Diagnosis and imaging studies of traumatic hip dislocation in the adult. Clin Orthop Rel Res 2000;377:15-23. [Google Scholar]
- 11.Shim SS. Circulatory and vascular changes in the hip following traumatic hip dislocation. Clin Orthop Relat Res 1979;140:255-61. [Google Scholar]
- 12.Uslu M, Arican M, Saritas A, Buyukkaya R, Kandis H. Combined bilateral asymmetric hip dislocation and anterior shoulder dislocation. World J Emerg Med 2012;3:311-3. [Google Scholar]








