[box type=”bio”] What to Learn from this Article?[/box]
Unique case of an overload related chronic tendonopathy causing non traumatic tendon rupture understating the fact that chronic tendonopathy should be promptly recognized and adequately treated
Case Report | Volume 5 | Issue 1 | JOCR Jan-March 2015 | Page 58-61 | Tony Mangano, Paola Cerruti, Ilaria Repetto, Roberto Trentini, Marcello Giovale, Francesco Franchin. DOI: 10.13107/jocr.2250-0685.257
Authors: Tony Mangano[1], Paola Cerruti[1], Ilaria Repetto[1], Roberto Trentini[1], Marcello Giovale[1], Francesco Franchin[1].
[1] Department of Orthopedics and Traumatology, University of Genova, School of Medicine; Largo Rosanna Benzi 10, Padiglione 40, 16132 Genova, Italy
Address of Correspondence:
Dr Tony Mangano, MD, Department of Orthopaedics and Traumatology, University of Genova, School of Medicine, Padiglione 40, Largo Rosanna Benzi 10, 16132 Genova, Italy. E-mail address: twmangano@gmail.com
Abstract
Introduction: Distal triceps tendon rupture is an uncommon lesion rarely due to a non–traumatic mechanism. In these cases, the majority of patients show predisposing factors for tendon degeneration: underlying medical co-morbidities, previous systemic and locally injected corticosteroids and systemic anabolic steroids. A clear evidence for an etiopathogenetic role for chronic tendonopathy in triceps tendon rupture is still lacking.
Case Report: We report the case of a rare non-traumatic complete rupture of the triceps tendon, at the olecranon insertion, occurring in a healthy male middle-aged non-professional bodybuilder. He presented to our attention with a five days history of weakness, swelling and pain at the left elbow, started after a snapping sound during a single arm triceps extension exercise. He was a healthy sportsman, no smoker and no drinker. He had suffered, in the two months before, of mild bilateral exercise-related elbow discomfort, never limiting his sport and daily activities. The man was treated by an early surgical repair. Histological analysis was conducted on intraoperative samples. The treatment allowed complete remission and return to sport practice without functional deficit.
Conclusion: An overload-related chronic tendonopathy was identified as the unique factor with causal role in the determinism of the above described lesion. This case highlights, for the first time in literature, that just a chronic tendonopathy, in absence of any other predisposing condition, can lead to a non-traumatic complete triceps tendon rupture.
Keywords: triceps, tendon rupture, chronic tendonopathy, tendon surgery.
Introduction
Triceps tendon rupture is a very rare lesion. Diagnosis is often complicated, delayed or completely missed [1,2,3]. The most common mechanism of injury is a fall or a direct blow to the posterior aspect of the elbow [2,4]. Few cases are described of non traumatic complete triceps tendon rupture, and most of them presented with underlying medical comorbidities known to determine pathologic changes and finally weaken the tendon structure: rheumatoid arthritis, systemic lupus erythematosus, chronic renal failure, hyperparathyroidism [5], xanthoma, hemangioendothelioma, diabetes mellitus [6]. Systemic and locally injected corticosteroids, as well as systemic anabolic steroids, are broadly accepted to have a causal role in tendon degeneration, and to be a contributory cause in tendon rupture, especially in otherwise healthy sportive people [7,8,9,10]. Because of a limited number of reported cases of such lesion, and the frequent contemporary presence of known predisposing conditions, a clear evidence for an etiopathogenetic role for chronic tendonopathy in triceps tendon rupture is still lacking [8,10].
Case report
A 52-year-old businessman and enthusiastic bodybuilder since the age of 25 presented to our attention with a five days history of weakness, swelling and pain at the left elbow. He referred of a sudden origin of the symptoms, associated with a snapping sound in the posterior aspect of the elbow, during a single arm triceps extension exercise. There were no systemic disorders at present, or in the medical history of the patient. He was a healthy sportsman, no smoker and no drinker. He did never sustain any pharmacological treatment till now, with particular respect to systemic and local corticosteroids and anabolic steroids. For approximately two months upon presentation, the patient had suffered for mild bilateral exercise-related elbow discomfort, never limiting his sport activity.
At the time of hospitalization, blood tests resulted normal, as well as electrocardiographic analysis, arterial pressure and general physical parameters.
Examination revealed a swelling of moderate degree in the posterior aspect of the elbow, with a palpable defect just upon the triceps tendon olecranic insertion site. No ecchymosis was present. The patient had no limitation in elbow flexion, but showed an extension lag of approximately 25 degrees. Resistive extension was impossible and painful. Strength testing of the injured triceps was 2/5 with respect to contralateral side. X-rays showed a small bony cortical avulsion of the posterior olecranon (Fig. 1a). Ultrasounds and Magnetic Resonance imaging both confirmed the complete triceps rupture at the tendo-osseous junction (Fig. 1b).
Surgical exploration revealed a complete rupture of the triceps tendon distal insertion, with avulsion of a small flack of cortical bone and partial conservation of lateral expansions to the forearm fascia (Fig. 1c). Triceps tendon showed altered color and consistence suggesting chronic tendonopathy. After surgical debridement triceps tendon was reinserted on the posterior aspect of the olecranon (Fig. 1d). We used non-absorbable Krakow-like sutures (Ethibond No.2, Ethicon, Sommerville, NJ), and these were brought through two holes drilled in the olecranon, from proximal to distal. A third hole was drilled transversely into the olecranon, to pass a further wire used for cerclage. The arm was held in approximately 40 degrees of flexion for tensioning.
Histological analysis was conducted on intraoperative samples. It reported fibrous connective tissue with sclerohyalinosis, chronic microtraumatism-attributable chondrocalcinosis-like degeneration, mixoid degeneration and chronic inflammation foci with neoangiogenesis (Fig. 2a-d).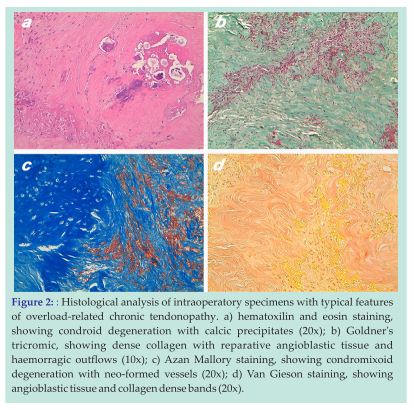
At discharge from the hospital, the day following surgery, the arm was immobilized in a long articulated splint, blocked at 30 degrees of flexion. One week after surgery, a weight free range of motion of 15-45 degrees was allowed. Complete extension was allowed from the second week after surgery. Flexion was increased of 15 degrees every week. After reaching 90 degrees, free flexion was allowed. One month after surgery the patient began physical therapy with isokinetic exercises and at two months he already showed a near complete functional recovery. No complications were reported during the entire 24 months follow up period.
Discussion
Distal triceps tendon ruptures are uncommon injuries. In an historical survey, among 1014 tendon injuries, Anzel et al. [1] reported that only 8 were triceps injuries. The most common site for rupture is at the insertion into the olecranon, with an avulsion mechanism of lesion, but intramuscular and musculotendineous rupture have been reported too [2,4,8]. Low frequency, little information, and clinical appearance with generally low degree of suspicion, are fundamental factors that reported diagnostic delays and missed diagnoses must be accounted to [6,11].
Most patients with triceps tendon ruptures present to the clinician with an acute injury, complaining of sudden pain in the posterior aspect of the elbow after trauma. Swelling, ecchymosis, pain and painful limitation on elbow extension, with or without weakness, are hallmarks of the examination. A palpable gap at the triceps distal insertion site is frequently reported (gap sign) [3,8]. Radiographic findings are usually minimal, but strongly suggestive, when present. Avulsion of a small flack of cortical bone from the olecranon (flake sign) could be quite useful in clarifying the diagnosis [3,4]. Ultrasounds and/or magnetic resonance imaging could help in defining localization and extension of the tear and showing whether rupture is complete or partial: these are fundamental informations while planning the treatment [12,13]. It is of note that active elbow extension may be preserved with a 10 to 90% or more tear, because of lateral triceps expansions to forearm fascia [11]. Extensive tears, however, are recommended to receive a prompt operative repair, while a non-operative approach, with splint protection for some weeks, is the gold standard treatment for partial tears [3,4,11,14]. In our patient, no ecchymosis was found, but all of the other clinical signs were present, with painful partially conserved extensor function. Ultrasounds and magnetic resonance imaging confirmed the complete triceps rupture from the tendo-osseous junction with triceps retraction.
Indirect trauma with fall on the outstretched hand as well as direct trauma to the posterior aspect of the elbow is the most common mechanisms of injury. However, when the structural integrity of the tendon has been altered, spontaneous rupture can occur following minimal to moderate force [3,4]. Known predisposing conditions to triceps tendon rupture involve rheumatoid arthritis, systemic lupus erythematosus, chronic renal failure, hyperparathyroidism, diabetes mellitus, systemic corticosteroids intake and treatments with quinolones [2,3,4,5,6]. Furthermore, some non-systemic factors, such as local steroid injections and olecranic bursitis, have been correlated with triceps injury as well [10].
Many cases reported in the scientific literature deal with triceps tendon complete ruptures that occurred in bodybuilders or weightlifters during a competition or an exercise. In the majority of them a substantial role for tendon degeneration and rupture was ascribed to histories of anabolic steroid intake or local corticosteroids injections [10]. Several experimental evidences agree in demonstrating changes and deleterious effects anabolic steroids exert on biochemistry, ultrastructure and finally on the biomechanical properties of tendons [7]. In a recent work, Sierra et al. [8] described a complete traumatic triceps tendon rupture in a 36-year-old weightlifter with history of anabolic steroid intake and of intrinsic asthma treated with inhaled corticosteroids. In the same work, authors reviewed 16 similar cases of triceps tendon injuries: only 3 were non traumatic, and 2 of these had a history of olecranic bursitis at the injured elbow. Sollender et al. [10] reported on four middle-aged healthy bodybuilders who sustained a triceps tendon complete rupture while weight-lifting or hitting a ball in a baseball match. The three patients who sustained the injury while weight-lifting complained a history of chronic elbow pain and two out of three had been previously treated with local corticosteroids injections. Furthermore, all of the four patients acknowledged a past or still on going systemic anabolic steroid intake. Authors pointed out the difficulties in defining a causal role for chronic tendonopathy in the determinism of the lesion. In the English literature, we found only one case report with strong similarities to the case described in this work [9]. However, in their work, Louis and Peck described the case of a injury occurred while notable weight-lifting, without mention of previous history of elbow pain. Because of the frequent coexistence of multiple known risk factors for tendon degeneration and rupture, a clear definition of the eventual causal or contributory role of every single one of these is still lacking.
The case we reported presents some peculiar features making it interesting from several points of view. Because of personal choice, our patient is a health conscious. He doesn’t smoke and he rarely drinks alcoholics. His business mainly deals with public relations and he spends in sport practices almost all of the leisure. He never used anabolic steroids nor systemic or local corticosteroids or quinolones. He is completely free of any of the known risk factors for tendon pathology. Since approximately two months before the injury, he complained a mild pain at the posterior aspect of both the elbows. Such pain aroused insidiously and was sharpened by repetitive movements of extension against resistance. Despite a subchronic pattern, pain always remained at a mild extent and never needed NSAIDs intake to be blunted. It did not limit the activities of daily living of the patient and sport practices as well.
It could be difficult to demonstrate whether the patient had sustained a partial rupture of the triceps tendon before its complete rupture, or if the tendon was already partially damaged because of repetitive exercises and microtraumatims and to what extent: we only know the patient did not complained any prodromic symptoms since two months before the accident occurred. We do not have any instrumental data prior of the injury, nor we could carry out an objective preoperative and postoperative muscle testing and these could be points of limitation of this study. However, we think that elbow pain with insidious arising, without any functional limitation or weakness at resistive extension, could be bona fide ascribed to chronic insertional triceps tendonopathy. Furthermore, histologic analysis of intraoperative samples from the ruptured tendon confirmed the presence of degeneration and chronic inflammatory foci. All of these features are known to characterize a tendon pathology strictly related to repetitive microtraumatism and chronic flogosis.
It is broadly accepted that the tendon-bone insertion site is a highly specialized microenvironment, with peculiar biochemical and histological properties. It is important to note, as well, that in the postnatal organism, a normal tendon-bone insertion site is not regenerated after tendon to bone repair, and this will lead to healing with reactive scar formation. The overall structure, composition and organization of a normal insertion site do not regenerate, and its biomechanical properties too [15]. Furthermore, several experimental works stated that a congruent immobilization period during tendon healing represents a necessary condition in order to grant a sufficient degree of organization of the new-produced collagen fibers, and a partial recovery of the mechanical and resistive properties of the injured site [15]. We hypothesize that in our patient the biologically imperfect mechanism of tendon healing further suffered the non-stopped sport practices. This finally resulted in a poor quality scar tissue with lower resistive properties, unable to bear what till that moment was considered a normal weight. We are aware the presence of a small bony avulsion could drive some doubts about the nature of the lesion. However, neither direct nor indirect trauma determined the tendon rupture, which happened during a moderate weight triceps extension exercise. One could only hypothesize that when the degenerated part of the tendon gave away, the remnant healthy insertional area resulted no more able to sustain weight and gave away in turn, with avulsion of the bone flake being justifiable by mean of a strict tendon-to-bone link at the same residual healthy tendosseous junction.
We hope the case we reported, when considered together with previously published similar cases, will contribute in clarifying the role an overload-related chronic insertional tendonopathy could have in the determinism of a complete non traumatic triceps tendon rupture.
Conclusion
Triceps tendon rupture is an uncommon tendon injury. Despite acute trauma represents the main etiological mechanism, several reports in the literature describe cases of non-traumatic ruptures, often in bodybuilders and weightlifters, often associated with multiple known risk factors for tendon degeneration. The case described in this work lead us to confirm that the bodybuilders and weightlifters category represent per se an at risk category for this kind of lesion. Furthermore, we reported a case of non traumatic complete triceps tendon rupture at the level of the tendo-osseous junction in an otherwise healthy patient, free of any of the known risk factors. The underlying overload-related chronic tendonopathy was identified as the unique cause the lesion is attributable to. The overall relevance of the here presented case relies in the fact that, for the first time, we describe in scientific literature as just a chronic tendonopathy, in absence of any other predisposing condition, can lead to non-traumatic complete triceps tendon rupture.
Clinical Message
Triceps tendon rupture is a rare injury, often misdiagnosed or diagnosed with delay. Overload-related chronic tendonopathy could represent a causal factor for this kind of lesion, also in a patient free of any of the known risk factors for tendon injury. This condition should be carefully identified and adequately treated in order to low the risk of spontaneous tendon subcutaneous rupture.
Reference
1. Anzel SH, Covey KW, Weiner AD, Lipscomb PR. Disruption of muscles and tendons, an analysis of 1014 cases. Surgery 1959;45:406-14
2. Rineer CA, Ruch DS. Elbow tendinopathy and tendon ruptures: epicondylitis, biceps and triceps ruptures. J Hand Surg 2009;34A:576-566
3. van Riet RP, Morrey BF, Ho E, O’Driscoll SW. Surgical treatment of distal triceps ruptures. J Bone Joint Surg 2003; 85A:1967-1961
4. Vidal AF, Drakos MC, Allen AA. Biceps tendon and triceps tendon injuries. Clin Sports Med 2004; 23:722-707
5. Tsourvakas S, Gouvalas K, Gimtsas C, Tsianas N, Founta P, Ameridis N. Bilateral and simultaneous rupture of the triceps tendons in chronic renal failure and secondary hyperparathyroidism. Arch Orthop Trauma Surg 2004;124: 280-278
6. Chan APH, Lo CK, Lam HY, Fung KY. Unusual traumatic triceps tendon avulsion rupture: a word of caution. Hong Kong Med J 2009; 15(4):296-294
7. Kennedy JC, Willis RB. The effects of local steroid injections on tendons: a biomechanical and microscopic correlative study. Am J Sports Med 1976; 4(1):21-11
8. Sierra RJ, Weiss NG, Shrader MW, Steinmann SP. Acute triceps ruptures: case report and retrospective chart review. J Shoulder Elbow Surg 2006; 15(1):134-130
9. Louis DS, Peck D. Triceps avulsion fracture in a weightlifter. Orthopedics 1992; 15(2):208-207
10.Sollender JL, Rayan GM, Barden GA. Triceps tendon rupture in weight lifters. J Shoulder Elbow Surg 1998; 7:153-151
11.Sharma SC, Singh R, Goel T, Singh H. Missed diagnosis of triceps tendon rupture: a case report and review of literature. J Orthop Surg (Hong Kong) 2005;13: 309-307
12.Kaempffe FA, Lerner RM. Ultrasound diagnosis of triceps tendon rupture. A report of 2 cases. Clin Orthop 1996; 332:142-138
13.Gaines ST, Durbin RA, Marsalka DS. The use of magnetic resonance imaging in the diagnosis of triceps tendon ruptures. Contemp Orthop 1990; 20:611-607
14.Levy M. Repair of triceps tendon avulsions or ruptures. J Bone Joint Surg Br 1987;69:115
15.Rodeo SA (2007). Biologic augmentation of rotator cuff tendon repair. J Shoulder Elbow Surg 2007;16:197S-191S
| How to Cite This Article: Mangano T, Cerruti P, Repetto I, Trentini R, Giovale M, Franchin F. Chronic Tendonopathy as a Unique Cause of Non Traumatic Triceps Tendon Rupture in a (Risk Factors Free) Bodybuilder: a Case Report. Journal of Orthopaedic Case Reports 2015 Jan-March;5(1): 58-61. Available from: https://www.jocr.co.in/wp/2015/01/28/2250-0685-257-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com





