[box type=”bio”] What to Learn from this Article?[/box]
MO can effect individual muscle in a group of muscles. If conservative treatment fails intoto excision of the mass and aggressive physiotherapy decreases chances of recurrence.
Case Report | Volume 5 | Issue 3 | JOCR July-Sep 2015 | Page 92-94| I Muni Srikanth, Amar Vishal, K Ravi Kiran. DOI: 10.13107/jocr.2250-0685.321.
Authors: I Muni Srikanth[1], Amar Vishal[1], K Ravi Kiran[1].
[1] Department of Orthopaedics, ASRAM Medical College, Eluru, Godavari District, Andhra Pradesh, India.
Address of Correspondence
Dr. I Muni Srikanth
54-20/2-14A, SF 302, Surya Residency, Bharati Nagar 7, Vijayawada – 520 008, Andhra Pradesh, India.
Email: iythamunisrikanth@gmail.com
Abstract
Introduction: Myositis ossificans (MO), heterotopic ossification, occurs in muscles and soft tissue. This lesion contains actively proliferating fibroblasts and osteoblasts. It commonly affects vigorous young men and more so among athletes. It occurs as a result of trauma, either acute or chronic and can also arise near joints in neurological disorders. By time of presentation, ossification is extensive and the benign nature of the lesion is usually evident on radiological studies. Most common muscles involved in MO are the flexor muscles of the arm, the hamstrings and quadriceps femoris.
Case Report: We present a case of MO with isolated involvement of rectus femoris in mid-thigh and sparing of other three muscles of quadriceps femoris, with no improvement following physiotherapy and medical management requiring surgical excision for better prognosis with no recurrence.
Conclusion: MO, a benign lesion, is known to affect the flexors of the arm, the hamstrings, and quadriceps femoris; it must be noted that even individual muscle can also be affected as shown in the above case presentation without involving whole group of muscles. Surgical excision is indicated if non-operative measures are not successful.
Keywords: Myositis ossificans, benign, rectus femoris, non-neoplastic.
Introduction
Synonyms for myositis ossificans (MO) are florid ossification, heterotopic ossification, ectopic ossification, neurogenic ossifying fibro myopathy, traumatic MO [1,2]. It is a rare non-neoplastic condition of unknown pathogenesis causing progressive ossification of muscles and other soft tissues [1,3,4]. The pathologic bone formed in soft tissues do not normally ossify [1]. The new bone often abuts existing skeletal structure; it does not interfere with the configuration of the periosteum [5]. The lesion contains actively proliferating fibroblasts and osteoblasts. Early in its development it may be confused with a malignant tumor [3]. MO occurs as a result of trauma, either acute or chronic and can also arise near joints in neurological disorders [6]. Vigorous young adults and adolescents, predominantly males, who may or may not have had significant trauma are affected most frequently [1,3,4]. MO is a common condition that occurs among athletes in association with muscle and/or tendon strain or contusion [7]. Causes that have been cited are sports injuries, such as American football, and repetitive occupational trauma, such as in cavalrymen and shoemakers [6]. MO is thought to be transmitted as an autosomal dominant trait with variable expressivity, however, most cases are sporadic [1,4]. There are both localized form and widespread syndrome. Localized form is usually posttraumatic and well-circumscribed lesion that frequently complicates hematoma formation of the muscles, particularly of the proximal extremities, and widespread syndrome occurs in fibrodysplasia ossificans progressive [1]. Connective tissues involuntary muscles, aponeuroses, tendons, fascia, and ligaments are the sites of ectopic bone formation [4]. Most often involved are the flexor muscles of the arm and the quadriceps femoris. Non-typically a mass develops rather rapidly [3]. The lesions comprise a wide range of histologic features from osteoma-like to osteosarcoma-like appearances [3,7]. The diagnosis of MO containing highly cellular areas with islands of osteoid is often difficult [7]. Any roentgenograms made early may reveal no mineralization, but by the time the lesion is observed clinically, at least some ossification is usually seen [3]. Our paper presents a rare case of MO in rectus femoris alone, sparing of other muscles of quadriceps femoris.
Case Report
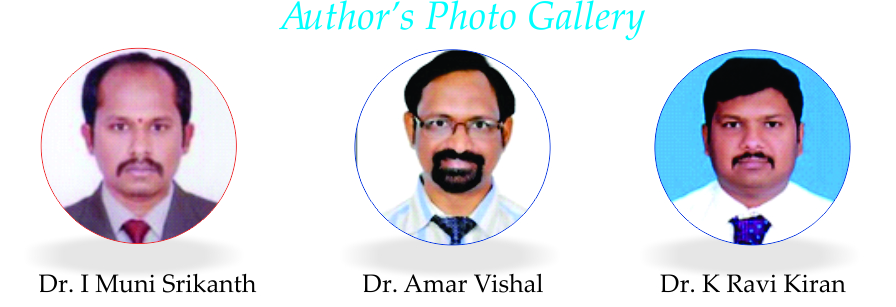
We present a 24-year-old male presents to our outpatient department with pain and swelling in the right upper thigh for 4 months. Swelling associated with mild pain, was insidious in onset and gradually progressive. There was a history of blunt injury to the right thigh without any bony fracture 6 months back associated with loss of consciousness. Patient recovered well with conservative treatment for closed head injury. There was history of massage to the right thigh. Clinical examination revealed a single, large, oval swelling of about 12 cm × 6 cm noted in the anterior aspect of left thigh. Swelling was hard consistency and it was mobile and pinchable skin over. The patient had a normal range of movement at hip. Range of motion (ROM) at knee was 0-60°. After being investigated blood parameters such as alkaline phosphatase, serum calcium, and phosphate are within normal limits. An x-ray revealed a well circumscribed peripherally calcified mass with a radiolucent center and a radiolucent cleft that separates the ossified mass from cortex of adjacent femur bone (Fig. 1). We subjected the patient to physiotherapy and tablet indomethacin (50 mg BD) for 3 weeks. As he had no functional improvement with non-operative measures planned for surgical excision of the calcified mass into. Per-operative findings include, a well-defined mass appears to be arising from rectus femoris muscle and its size measures about 15 cm × 6 cm and other muscles in quadriceps femoris are normal (Fig. 2). A clear zone is present between femur and mass. Histopathology confirmed our diagnosis as MO. Active assisted physiotherapy including hamstrings and quadriceps exercises were encouraged. Continuous passive motion of the knee was done under physiotherapist guidance. The patient was followed up once in 6 weeks. On discharge at 2 weeks knee ROM was 0-100°. At 6 months follow-up knee ROM was 0-130° and by 1 year full ROM of the left knee was achieved with no signs of recurrence on follow-up X-rays.
Discussion
MO traumatica (MOT) is defined as a non-neoplastic proliferation of cartilage and bone in an area of muscle that has been exposed to trauma. The most common sites for MOT formation are the anterior thigh and the brachialis muscle [8-10]. Factors associated with development of MO include the severity of a contusion, continuing exercise after injury, massaging the injured area, applying local heat, and head injury [11]. Our patient had more than one factor associated with blunt injury triggering the pathology. Isolated involvement of rectus femoris with sparing of other muscles in quadriceps is a rare phenomenon and has not been documented in the literature to our knowledge. A decrease in ROM adjacent to the site of trauma is the most reliable predictor of MOT formation [10]. A heightened suspicion in patients who have had major direct trauma to muscle and who have not responded to no operative treatment after a period of 5 days or have worsened symptoms after 2 weeks from the inciting event will help in making diagnosis. Three different types of MOT have been described in the literature: Flat bone formation adjacent to the shaft of bone with damage to the periosteum (periosteal); bone formation that remains attached to the shaft of bone with damage to the periosteum (stalk); and intramuscular bone formation without disruption of the periosteal sleeve (intramuscular or disseminated) [12,13]. Our patient had intramuscular type of MO confirmed both radiologically and intraoperatively. The common clinical presentation is presence of a painful mass in the muscle, pain, and tenderness persisting in the area of large hematoma and usually with a 1-4 weeks history of trauma [14]. And on general examination, if large, a bony mass is palpable, and a differential diagnosis of bone tumor (often misdiagnosed as) osteogenic sarcoma is made [2,3]. Our patient came late to us with established radiological features of maturing MO thereby excluding osteogenic sarcoma (Fig. 1). Although indomethacin is widely used for prevention of heterotrophic ossification, its efficacy in MOT has not been clearly established [9,12,15,16]. Fisher et al. [17] studied the effect of systemic inhibition of prostaglandin synthesis on muscle protein balance after contusion injury in the rat and reported prostaglandin inhibition reduced the catabolic loss of muscle protein seen locally and peripheral to the injury site. However, Mishra et al. [18] observed rabbit muscles subjected to contusion injury had a deficit in torque and force generation at 28 days if treated with non-steroidal anti-inflammatory drugs when compared with the control group. The use of bisphosphonates has been bolstered by recent case reports that point to its effectiveness [1]. It is more effective at the initial period of treatment, with the gradual decline in its effectiveness later on [4]. Our patient had no improvement with physiotherapy or medical management. Surgery often is recommended when the patient is left with a limited ROM, functional limitation, and a prominent mass or enduring pain. Surgery is performed when the bone has fully matured as judged by the presence of a cortex on radiographs typically 6-12 months after the inciting event [9,12]. As our patient showed no improvement with non-operative measures, hence, we have planned surgical excision (Fig. 2). On 1-year follow-up, the patient didn’t have recurrence and achieved full ROM of knee joint.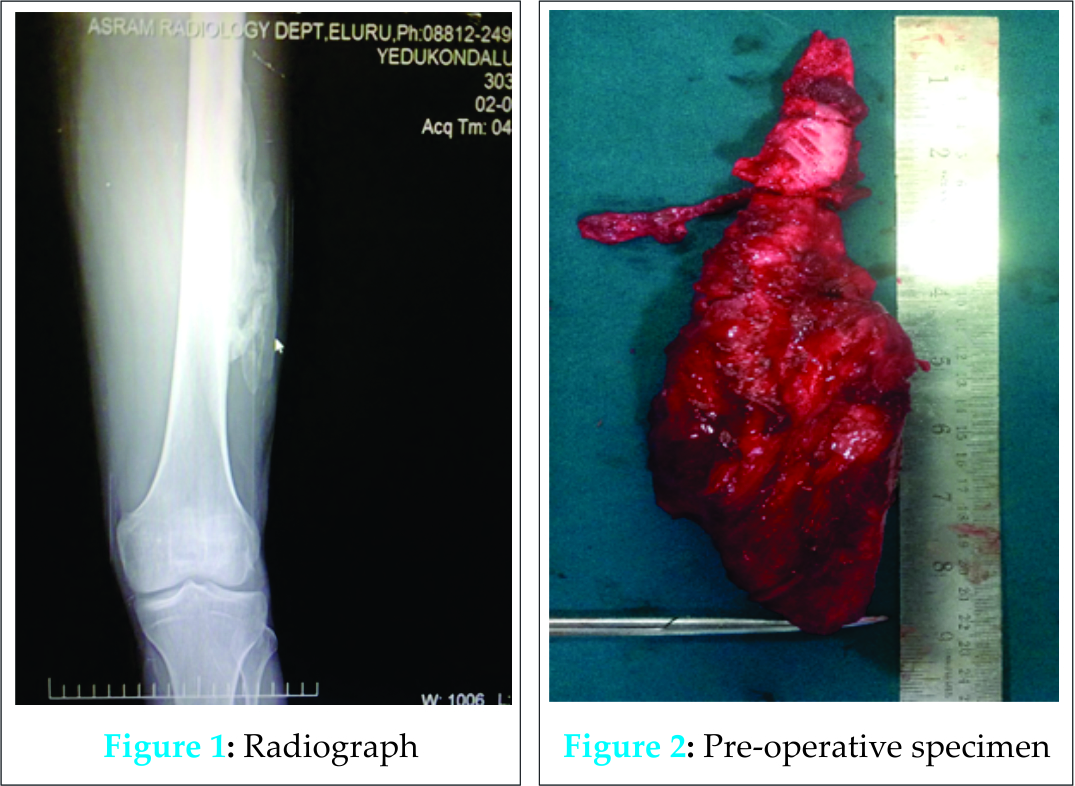
Conclusion
MO, a benign lesion, is known to affect the flexors of the arm, the hamstrings and quadriceps femoris, it must be noted that even individual muscle can also be affected as shown in the above case presentation without involving whole group of muscles. Surgical excision is indicated if non-operative measures are not successful.
Clinical Message
MO can effect even a single muscle without involving whole group of muscles. When MO doesn’t resolves with medical measures and physiotherapy, then complete surgical excision is to be done to avoid recurrence.
Reference
1. Hendifar AE, Johnson D, Arkfeld DG. Myositis ossificans: A case report. Arthritis Rheum 2005;53(5):793-5.
2. Myositis ossificans – DynaMed Ipswich (MA): EBSCO Publishing; 1995. Record No. 114671. Available from: http://www.search.ebscohost.com/login.aspx?direct=true&site=dynamed&id=AN+114671.Registration and login required. [Last updated on 2010 Jun 09; Last cited on 2010 Oct 11].
3. Pitcock JA. Tumours and tumour like lesions of somatic tissue. In: Crenshaw AH, editor. Campbell’s Operative Orthopaedics. 5th ed., Vol. 1. St. Louis: C.V. Mosby Co.; 1971. p. 1366.
4. Bar Oz B, Boneh A. Myositis ossificans progressiva: A 10-year follow-up on a patient treated with etidronate disodium. Acta Paediatr 1994;83(12):1332-4.
5. Baird EO, Kang QK. Prophylaxis of heterotopic ossification – an updated review. J Orthop Surg Res 2009;4:12.
6. Mann EG. Short report myositis ossificans in medieval London. Int J Osteoarchaeol 1993;3:223-6.
7. Sumiyoshi K, Tsuneyoshi M, Enjoji M. Myositis ossificans. A clinicopathologic study of 21 cases. Acta Pathol Jpn 1985;35(5):1109-22.
8. Huss CD, Puhl JJ. Myositis ossificans of the upper arm. Am J Sports Med 1980;8(6):419-24.
9. King JB. Post-traumatic ectopic calcification in the muscles of athletes: A review. Br J Sports Med 1998;32(4):287-90.
10. Ryan JB, Wheeler JH, Hopkinson WJ, Arciero RA, Kolakowski KR. Quadriceps contusions. West Point update. Am J Sports Med 1991;19(3):299-304.
11. Rothwell AG. Quadriceps Hematoma. A prospective clinical study. Clin Orthop Relat Res 1982;(171):97-103.
12. Beiner JM, Jokl P. Muscle contusion injury and myositis ossificans traumatica. Clin Orthop Relat Res 2002;403 Suppl:S110-9.
13. Ehara S, Shiraishi H, Abe M, Mizutani H. Reactive heterotopic ossification. Its patterns on MRI. Clin Imaging 1998;22(4):292-6.
14. Booth DW, Westers BM. The management of athletes with myositis ossificans traumatica. Can J Sport Sci 1989;14(1):10-6.
15. Iorio R, Healy WL. Heterotopic ossification after hip and knee arthroplasty: Risk factors, prevention, and treatment. J Am Acad Orthop Surg 2002;10(6):409-16.
16. Thorsson O, Lilja B, Nilsson P, Westlin N. Immediate external compression in the management of an acute muscle injury. Scand J Med Sci Sports 1997;7(3):182-90.
17. Fisher BD, Baracos VE, Reid DC. Effect of systemic inhibition of prostaglandin synthesis on muscle protein balance after trauma in the rat. Can J Physiol Pharmacol 1991;69(6):831-6.
18. Mishra DK, Fridén J, Schmitz MC, Lieber RL. Anti-inflammatory medication after muscle injury. A treatment resulting in short-term improvement but subsequent loss of muscle function. J Bone Joint Surg Am 1995;77(10):1510-9.
| How to Cite This Article: Srikanth IM, Vishal A, Kiran KR. Myositis Ossificans of Rectus Femoris: A Rare Case Report. Journal of Orthopaedic Case Reports 2015 July – Sep;5(3): 92-94 . Available from: https://www.jocr.co.in/wp/2015/07/10/2250-0685-321-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com