[box type=”bio”] Learning Points for this Article: [/box]
Complete femur replacement is a rare procedure, and this case report tries to provide a guideline about the correct procedure to be followed during this complicated procedure.
Case Report | Volume 7 | Issue 4 | JOCR July – August 2017 | Page 49-51| Raviprasad Kattimani, Jamie McConnell, Jon Waite. DOI: 10.13107/jocr.2250-0685.846
Authors: Raviprasad Kattimani[1], Jamie McConnell[1], Jon Waite[1]
[1] Department of Trauma and Orthopaedics, Warwick Hospital, Warwick, CV34 5BW, United Kingdom.
Address of Correspondence
Dr. Raviprasad Kattimani,
Flat 36, Remburn Garden, Warwick, CV34 5BH, United Kingdom.
E-mail: raviprasad.kattimani@gmail.com
Abstract
Introduction: Pyomyositis is an acute intramuscular bacterial infection of the skeletal muscle. It is rare in temperate climate countries. We report a case of Pyomyositis of gluteus medius with review of literature.
Case report: We present a case of 12 year old boy presented with right hip pain, fever and antalgic gait. Inflammatory markers were raised at presentation. The pelvic radiograph and ultra sound scan of right hip joint did not detect any abnormality. The Magnetic Resonance Imaging (MRI) scans revealed inflammatory oedema in the right gluteus medius muscle. He was treated with intravenous Flucloxacillin for 10 days and later 6 weeks of oral Flucloxacillin. At the 6 weeks follow up patient was asymptomatic with normal gait. MRI at 6 weeks did not show any fluid collection in gluteus medius.
Conclusion: Pyomyositis is rare in temperate countries. It must be considered as one of the differential diagnosis in a child presenting with hip pain, fever and raised inflammatory markers.
Key words: Gluteus medius, hip, Pyomyositis.
Introduction
Pyomyositis is an acute intramuscular bacterial infection of the skeletal muscle, secondary to haematogenous spread of a microorganism, which is neither secondary infection of adjacent skin, soft tissue, or bone, nor due to penetrating trauma [1,2]. The incidence is higher in warmer climates, hence the alternative nomenclature ‘‘tropical pyomyositis’’. It commonly affects the muscles around the hip joints and can mimic a range of acute paediatric disorders such as septic arthritis or appendicitis [3]. Diagnosis is often delayed as a result of ambiguous presentation, non-specific differential diagnosis, a variety of clinical presentations, its relative rarity, and the unfamiliarity of physicians with the disease [4].
Case Report
12 year old Caucasian male was referred by his general practitioner to the orthopaedic department with a suspected septic arthritis of hip. He had a 2 day history of right hip pain, pyrexia, and difficulty in weight bearing during this period. There was no history of trauma or any infection in the preceding 3 months.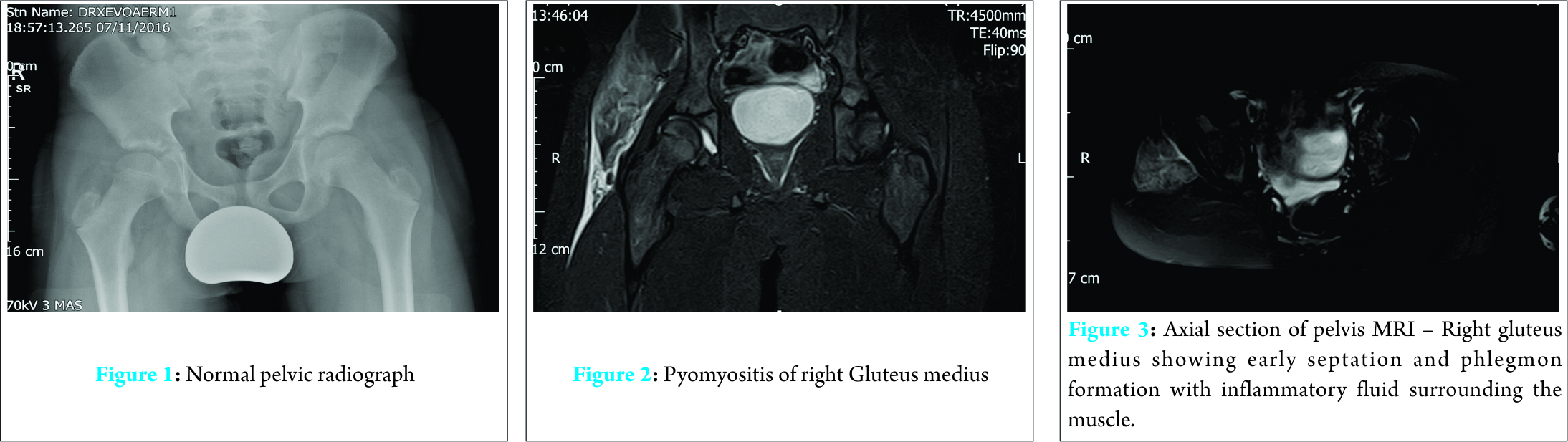
On examination, he had an antalgic gait. His core temperature was elevated at 38.0 ° C. There was no erythema, swelling or localized temperature change at the thigh or gluteal region. His hip was non-tender to passive rotation or flexion, but he reported pain on active hip flexion beyond 90 °. Laboratory investigations revealed white cell count of 9.20×109/L and C reactive protein (CRP) of 93 mg/L. Blood culture revealed staphylococcus organism sensitive to Flucloxacillin. Immunocompromised state had been ruled out by the Pediatric team of doctors. Radiograph of pelvis (Fig.1) and ultrasound scan of the left hip showed no abnormality but subsequent magnetic resonance imaging (MRI) scan of pelvis showed septation and phlegmon formation along with inflammatory fluid and edema in the right gluteus medius muscle. (Figs 2 and 3). Patient was allowed to mobilize partial weight-bearing with crutches for a week and later mobilized with full weight bearing at discharge. No splints were used to immobilize the affected limb. The patient was treated with intravenous Flucloxacillin 25 mg/kg every 6 hourly for 10 days. By this stage, CRP had fallen to 5 mg/L, and he was discharged on oral Flucloxacillin 500mg QDS for 4 weeks, with subsequent outpatient review at 2 weeks and 4 weeks. 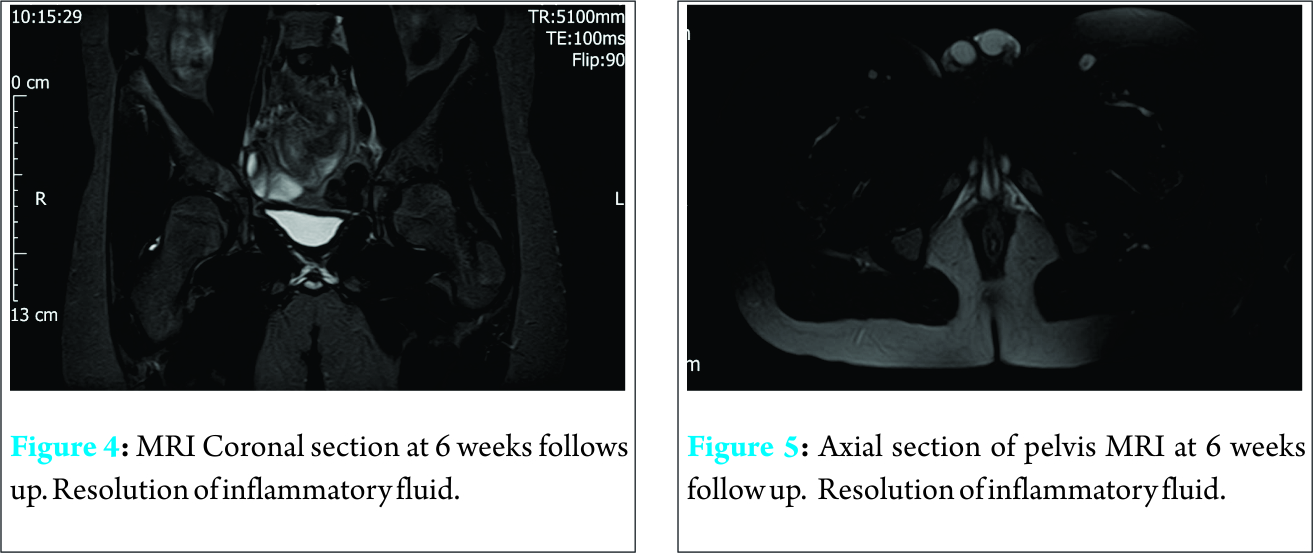
At 2 weeks, his hip pain had fully resolved, and he demonstrated a full range of painless active hip movement, although he continued to use crutches when walking. There was no tenderness over the gluteal or trochanteric region. At 4 weeks, he was permitted full weight bearing without any support. His CRP was < 3 mg/L. A repeat MRI scan at 6 weeks showed no evidence of any oedema or fluid collection in and around right gluteus musculature ( Figs 4 and 5).
Discussion
Scriba first described Pyomyositis in 1885 [5]. It is an endemic disease in tropical regions especially in parts of Africa and South Pacific, hence the alternative name tropical pyomyositis. It is rare in countries with a temperate climate [6]. The first case in the UK was reported in 2010 [7].
Etiology
Staphylococcus aureus is the responsible organism in up to 95% of cases [7, 8]. Other rare bacterial causes of pyomyositis include group A ß-hemolytic streptococci, a-hemolytic streptococci and non-hemolytic streptococci Streptococcus pneumoniae, Staphylococcus epidermidis, Staphylococcus pyogenes, Streptococcus pyogenes, coliform, Fusobacterium, Haemophilus influenzae, Escherichia coli, Neisseria gonorrhoeae,, Klebsiella, Yersinia enterocolitica, Pasteurella species and Pseudomonas species [9,10,11,12,13,14,15]. Predisposing factors include Diabetes [8, 16], Hematological disorders [17, 18], AIDS [10, 19] and connective tissue disorders [20, 21].
Stages of Pyomyositis
Pyomyositis has three discrete stages of presentation. The early ‘‘invasive’’ stage is characterized by pain and swelling of the involved muscle, with or without fever. The second ‘‘suppurative’’ stage occurs 10-21 days after the onset. This stage is characterised by abscess formation. Symptoms of fever and malaise are commonly noted. It may be possible to palpate a fluctuant muscle swelling, and there will be a marked leukocytosis and elevated sedimentation rate. About 90% of patients will present during this stage. The third ‘‘septiceamic’’ stage is associated with multiple metastatic abscesses formation. Lower limb and trunk are the most common sites involved [10].
Investigations
The laboratory findings in Pyomyositis are non-specific. A rise in Erythrocyte sedimentation rate [ESR] is commonly found, and a leucocyte left shift (an increase in the number of immature leukocytes) may be suggestive [23]. Blood cultures were positive in only < 5% of cases in reported tropical climates [9].
Plain radiograph may be rarely helpful in the diagnosis but it helps to exclude any bony pathology [24]. Cross-sectional imaging may be the most valuable investigation. Ultrasound scan of the hip can exclude septic arthritis (an important differential diagnosis). MRI is preferred over computed tomography (CT), as the former is better in identifying soft tissue abnormalities. MRI will classically show diffuse fluid collection in the muscle with a rim enhancement if an abscess is present [7].
Differential Diagnosis
Pyomyositis must be differentiated from septic arthritis, osteomyelitis, Perthes disease, juvenile rheumatoid arthritis, discitis, appendicitis, deep vein thrombosis, synovitis, perinephric abscess and soft tissue sarcomas [3]. Diagnosis of pyomyositis is often delayed as the patients usually present late, the condition is rare and many physicians are unaware of the entity [9, 24].
Treatment
In the early stages or pre suppurative phase intravenous antibiotics are the treatment of choice. Variable recommendations have been given regarding the choice of antibiotics [7]. Bickles et al. recommend cloxacillin with the addition of aminoglycoside in an immuno compromised patient and in sepsis [25]. Zimbelman et al. advised clindamycin with or without penicillin [26]. If an abscess is present, it may be necessary to consider either open incision and drainage or percutaneous catheter drainage under CT or Ultra-sonographic guidance [7].
Results
If the condition is recognized early and managed aggressively, the majority of patients show complete recovery with no long-term complications [9, 26]. If the disease is allowed to enter the later stages, complications may include cause extended hospital stay, local extension into adjacent bone or joint, compartment syndrome, remote infection such as pericarditis, endocarditis, myocarditis, lung and brain abscesses, renal failure, septicemia and death [9, 27, 28, 29]. Mortality rates between 0.9% and 10% have been reported [27, 28, 29].
Conclusion
Early recognition is a key to the management of this rare condition. Appropriate intravenous antibiotics should be given at an early stage. Incision and drainage or guided percutaneous drainage will be required if an abscess has formed. The vast majority of patients show excellent recovery without any long term sequelae, but complications may result from delayed presentation and failure to make appropriate diagnosis.
Clinical message
Pyomyositis is uncommon in temperate climates. It must be considered as one of the differential diagnosis if a child presents with a fever, muscle pain, elevated CRP, ESR and leukocytosis. Early diagnosis is crucial to prevent morbidity and mortality. MRI is the investigation of choice.
References
1. Crum-Cianflone NF (2008) Bacterial, fungal, parasitic, and viral myositis. Clinical Microbiology Review 21: 473-494.
2. Crum-Cianflone NF (2006) Infection and musculoskeletal conditions: Infectious myositis. Best Practice & Research Clinical Rheumatology 20: 1083-1097.
3. Brown JD, Wheeler B (1984) Pyomyositis. Report of 18 cases in Hawaii. Arch Intern Med 144:1749–1751
4. Fowler A and Mackay A (2006) Community acquired methicillin-resistant Staphylococcus aureus pyomyositis in an intravenous drug user. Journal of Medical Microbiology 55: 123-125.
5. Ali, I, Rashdan, I ; Pyomyositis: A case report and literature review. Hospital Physician. 1999; 39–41.
6.Primary Pyomyositis J. Bickels, MD; L. Ben-Sira, MD; A. Kessler, MD; S. Wientroub, MD Journal of Bone and Joint Surgery Am, 2002 Dec; 84 (12): 2277 -2286 .
7. Unnikrishnan PN, Perry DC, George H, Bassi R, Bruce CE (2010) Tropical primary pyomyositis in children of the UK: an emerging medical challenge. International Orthopaedics 34: 109-113.
8. Goldberg JS, London WL, Nagel DM: Tropical pyomyositis: a case report and review. Pediatrics 1979; 63:298–300.
9. Chiedozi LC: Pyomyositis. Review of 205 cases in 112 patients. American Journal of Surgery 1979;137:255–259.
10. Rodgers WB, Yodlowski ML, Mintzer CM: Pyomyositis in patients who have the human immunodeficiency virus. Case report and review of the literature. Journal of Bone and Joint Surgery [Am] 1993;75:588–592.
11. Moore DL, Delage G, Labelle H, Gauthier M: Peracute streptococcal pyomyositis: report of two cases and review of the literature. Journal of Pediatric Orthopaedics 1986;6:232–235.
12. Swarts RL, Martinez LA, Robson HG: Gonococcal pyomyositis. Journal of American Medical Association 1981;246:246.
13. Schwab R, Panwalker AP: Klebsiellapyomyositis. American Journal of Medicine 1986;81:1116–1117.
14.Brennessel DJ, Robbins N, Hindman S: Pyomyositis caused by Yersinia enterocolitica. Journal of Clinical Microbiology 1984;20:293–294.
15. Gaut P, Wong PK, Meyer RD: Pyomyositis in a patient with the acquired immunodeficiency syndrome. Archives of Internal Medicine 1988;148:1608–1610.
16.Caldwell DS, Kernodle GW Jr, Siegler HF: Pectoralis pyomyositis: an unusual cause of chest wall pain in a patient with diabetes mellitus and rheumatoid arthritis. Journal of Rheumatology 1986;13:434–436.
17. Mitsuyasu R, Gale RP: Bacterial pyomyositis in a patient with aplastic anaemia. Postgradatuate Medical Journal 1980; 56:61–62.
18. Peller JS, Bennett RM: Bacterial pyomyositis in a patient with preleukemia. Journal of Rheumatology 1985;12:185–186.
19. Watts RA, Hoffbrand BI, Paton DF, Davis JC: Pyomyositis associated with human immunodeficiency virus infection. British Medical Journal 1987;294:1524–1525.
20.Blatt J, Reaman G, Pizzo PA: Pyomyositis in acute lymphocytic leukemia heralded by cutaneous vasculitis: brief communication. Medical Pediatric Oncology 1979;7: 237–239.
21. Minor RL Jr, Baum S, Schulze-Delrieu KS: Pyomyositis in a patient with progressive systemic sclerosis. Case report and review of the literature. Archives of Internal Medicine 1988;148: 1453–1455.
22. Adams EM, Gudmundsson S, Yocum DE, et al: Streptococcal myositis. Archives of Internal Medicine 1985;145:1020–1023.
23. Hall R ,Callaghan JJ, Moloney E, et al Pyomyositis in a temperate climate . Presentation, diagnosis and treatment. Journal of Bone and Joint Surgery [Am] 1990; 72:1240-1244.
24.Brickels J, Ben–Sira L, Kessler A, Wientroub S (2002) Primary pyomyositis. Journal of Bone and Joint Surgery Am 84-A: 2277–2286.
25. Zimbelman J, Palmer A, Todd J (1999) Improved outcome of clindamycin compared with beta–lactam antibiotic treatment for invasive Streptococcus pyogenes infection. Pediatric Infectious Disease Journal 18:1096–1100.
26. Hossain A, Reis ED, Soundararajan K Nontropical pyomyositis : analysis of eight patients in an urban center. American Journal of Surgery 2000 ; 66 : 1064-1066.
27.Levin MJ, Gardner P, Waldvogel FA. An unusual infection due to staphylococcus aureus New England Journal of Medicine 1971 ;284 : 196-198.
28. Malhotra P, Singh S, Sud A, Kumari S. Tropical pyomyositis : experience of a tertiary care hospital innorth-west India. J Assoc Physicians India 2000; 48 :1057-1059.
29. Patel SR, Olenginski TP, Perruquet JL, Harrington TM. Pyomyositis : clinical features and predisposing conditions. Journal of Rheumatology 1997; 24 : 1734-1738.
 |
 |
 |
| Dr. Raviprasad Kattimani | Dr. Jamie McConnell | Dr. Jon Waite |
| How to Cite This Article: Kattimani R, McConnell J, Waite J. Pyomyositis of Gluteus medius: A case report and review of the literature. Journal of Orthopaedic Case Reports 2017 Jul-Aug: 7(4): 49-51 |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com








