[box type=”bio”] Learning Point of the Article: [/box]
Resection arthroplasty is one of the last few treatment options for a patient with repeated, inadequately managed periprosthetic hip joint infection.
Case Report | Volume 9 | Issue 4 | JOCR July-August 2019 | Page 54-57 | Andris Dzerins, Matiss Zolmanis, Peteris Studers. DOI: 10.13107/jocr.2019.v09i04.1478
Authors: Andris Dzerins[1], Matiss Zolmanis[2], Peteris Studers[1],[2]
[1]Joint Laboratory of Traumatology and Orthopaedics, Riga Stradins University, 1007 Riga, Latvia,
[2]Department of Spine and Joint Surgery,Hospital of Traumatology and Orthopaedics, 1005 Riga, Latvia.
Address of Correspondence:
Dr. Andris Dzerins,
Joint Laboratory of Traumatology and Orthopaedics, Riga Stradins University, Dzirciema Street 16, 1007 Riga, Latvia.
E-mail: andris.dzerins93@gmail.com
Abstract
Introduction: Fibrous dysplasia (FD) is a rare congenital abnormality, in which parts of bone are replaced with fibrous stroma and woven bone, making it susceptible to pathological fractures. Osteomyelitis following intramedullary nailing of such fractures of the femur and periprosthetic joint infection (PJI) after hip arthroplasty is one of the most devastating complications and a true challenge for the orthopedic surgeon. To the best of our knowledge, this is the 1st time, such complications are reported in a patient with monostotic FD.
Case Report: We present a 30-year-old male patient with FD of the left femur, chronic osteomyelitis, recurrent periprosthetic hip joint infection after multiple revision arthroplasties, and two episodes of axillary vein thrombosis. Due to the severe structural changes and a large medial wall defect in the proximal femur with impairment of a large soft tissue zone, it was decided during operation not to put any other implants in the hip joint and perform only a resection hip arthroplasty procedure.
Conclusion: Managing a recurrent PJI in a patient with poor bone quality, severe bone defects, soft tissue compromise, and thromboembolic events is challenging even for the most experienced orthopedic surgeon. Resection arthroplasty is a salvage treatment option that should be considered in such complex cases.
Keywords: Fibrous dysplasia, osteomyelitis, periprosthetic joint infection
Introduction
Fibrous dysplasia (FD) is an uncommon congenital abnormality, in which parts of bone are replaced with fibrous stroma and woven bone due to altered osteogenesis, making the affected area more susceptible to pathological fractures[1]. FD can affect a single bone (monostotic form) or multiple bones (polyostotic form) in the body. The monostotic form is the most frequent, accounting for80% of FD cases [2]. As in our shown case, the patient had a monostotic FD form affecting the left femur. These patients may present with pathologic fracture with minor inciting trauma as the first presentation [3]. Internal fixation is usually the treatment of choice in such patients [4]. We present a 30-year-old male patient with multiple pathological fractures of the left femur due to FD which were internally fixated. The patient developed septic arthritis of the left hip joint, chronic osteomyelitis of the femur with soft tissue involvement. Later on, he over went total hip arthroplasty and developed recurrent periprosthetic joint infection (PJI) which was treated with six hip revision operations. The patient also had two episodes of the right axillary vein thrombosis. To the best of our knowledge, such a case has not been reported in the English literature.
Case Report
A 30-year-old male patient presented to our hospital with pain in the left hip region, reduced leg mobility due to theleft hip PJI with two fistulas in the upper lateral and anterior thigh region. Collecting anamnesis, the patient had a left distal femoral metaphyseal fracture due to a fall at the age of 10. At that time, X-rays showed dysplastic bone lesions of the left femur and the patient was diagnosed with monostotic FD. The patient had distal femoral osteosynthesis with a dynamic compression plate. The fracture healed without any complications. The plate was evacuated 1 year later and the dysplastic bone lesions were sealed with a bone allotransplant. Ten years later, the patient had a pathological left femoral neck fracture without any trauma.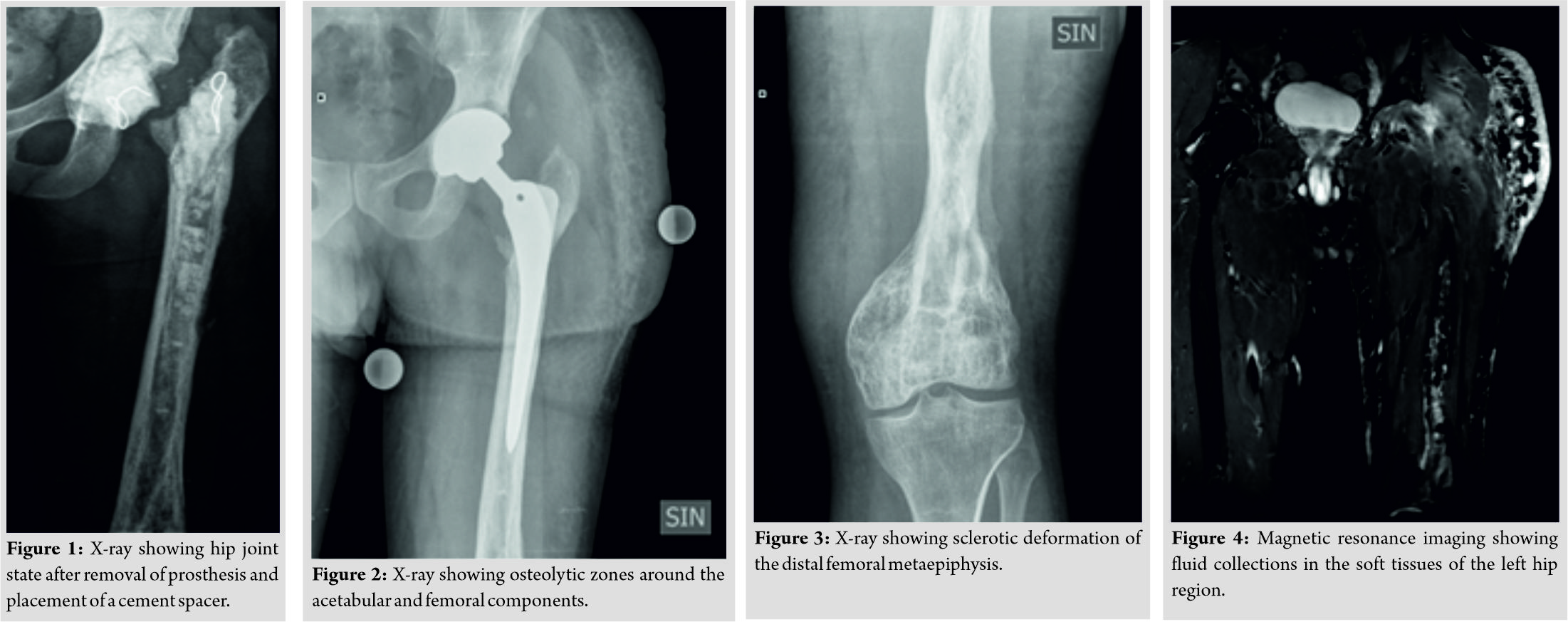 Osteosynthesis with intramedullary femoral nail was performed in another hospital. Six weeks after the operation, the patient developed growing pain and swelling in the left hip and distal thigh region. Septic arthritis of the left hip joint was diagnosed. The intramedullary nail was removed, femoral head resected, and the patient received systemic antibiotic therapy for 6 weeks. Afterward, debridement of the distal femoral metaphysis was performed, and bony cavities were sealed with bone graft substitute made of calcium sulfate. After 8 weeks, there were no signs of active infection and the patient over went total left hip arthroplasty with anuncemented prosthesis. Three years later, the patient developed a PJI. Local debridement, removal of the prosthesis, and placement of cement spacer incorporating gentamicin (Fig. 1) were performed in combination with systemic antibiotic therapy. Six weeks later, the spacer was removed and these conduncemented total hip arthroplasty was performed. As a complication, the patient developed lymphedema of the left leg. One year later, the patient had a repeated PJI which was treated with debridement, retention of the prosthesis, and systemic antibiotic therapy. Six months later, the patient developed deep vein thrombosis of the right axillary vein, which was treated with anticoagulant therapy. He was diagnosed with antiphospholipid syndrome and thoracic outlet syndrome. One year later, the patient developed posterior displacement of the femoral component in the left hip joint twice with a 1-month interval and both were reduced in a closed manner. One month later, he developed a repeated PJI which was treated with debridement, drainage, and systemic antibiotic therapy. Two fistulas opened in the left thigh region and the patient was transferred to our hospital. The patient had pain during motion in the left hip and moderate decrease in the range of motion. Routine analyses showed leukocytosis (15.90 × 109L) and increased C-reactive protein (67.1mg/L). Radiographs of the left hip showed osteolytic zones around the acetabular and femoral components with sclerotic deformation of the distal femoral metaepiphysis (Fig. 2 and 3). Our plan was a two-stage exchange hip revision arthroplasty by performing removal of the prosthesis, implantation of an antibiotic-impregnated articulating cement spacer, and after 6 weeks of systemic antibiotic therapy– implantation of a distally-interlocked modular femoral reconstruction prosthesis due to the severe bone defects in the left femur. The operative approach was through the previous operation scar of anterolateral approach– the third fistula was found underneath the scar tissue which was connected to the greater trochanter region. Tissue samples were taken for microbiological examination. Debridement, resection of the three fistulas, removal of the femoral and acetabular componentswith the use of an osteotome,and irrigation using the pulse lavage system with physiological sodium chloride solution wereperformed.Due to the severestructural changes and a large medial wall defect in the proximal femur withimpairment of a large soft tissue zone, it was decided during operation not to put any other implants in the hip joint. All cultures from soft tissue samples collected from the hip joint region grew Staphylococcus aureus (resistant only to trimethoprim-sulfamethoxazole). The patient received antibiotic therapy with oxacillin for 16 days. On the 1stpost-operative day, the patient started physiotherapy– learned to sit in the bed and began passive exercises of the left hip joint. On the 2ndday,the patient began to stand and gradually learned to walk with crutch assistance. He was allowed touch-down weight-bearinguntil full wound healing. A soft left hip orthosis was applied to maintain muscle tone and decreaseedema. The surgical wound healed without any signs of infection and the skin clips were removed on the 14th post-operative day. The patient was discharged from the hospital and continuedantibiotic therapy with ciprofloxacin for 4 weeks. After 5 months, magnetic resonance imaging of the pelvic region showed fluid collections in the soft tissues of the left hip joint region (Fig. 4). The patient had an ultrasound-guidedleft hip joint fluid aspiration, but the acquired samples did not grow any microorganisms. After 1 year from the last surgery, the patient is relatively satisfied–he is walking with two crutches and can apply 10% of body weight on the left leg when standing. The patient has acceptable clinical results without antibiotic suppression therapy –edema in the left leg has decrease; there is no pain in the left hip region during movement and no active fistulas. C-reactive protein is 2.0mg/L.
Osteosynthesis with intramedullary femoral nail was performed in another hospital. Six weeks after the operation, the patient developed growing pain and swelling in the left hip and distal thigh region. Septic arthritis of the left hip joint was diagnosed. The intramedullary nail was removed, femoral head resected, and the patient received systemic antibiotic therapy for 6 weeks. Afterward, debridement of the distal femoral metaphysis was performed, and bony cavities were sealed with bone graft substitute made of calcium sulfate. After 8 weeks, there were no signs of active infection and the patient over went total left hip arthroplasty with anuncemented prosthesis. Three years later, the patient developed a PJI. Local debridement, removal of the prosthesis, and placement of cement spacer incorporating gentamicin (Fig. 1) were performed in combination with systemic antibiotic therapy. Six weeks later, the spacer was removed and these conduncemented total hip arthroplasty was performed. As a complication, the patient developed lymphedema of the left leg. One year later, the patient had a repeated PJI which was treated with debridement, retention of the prosthesis, and systemic antibiotic therapy. Six months later, the patient developed deep vein thrombosis of the right axillary vein, which was treated with anticoagulant therapy. He was diagnosed with antiphospholipid syndrome and thoracic outlet syndrome. One year later, the patient developed posterior displacement of the femoral component in the left hip joint twice with a 1-month interval and both were reduced in a closed manner. One month later, he developed a repeated PJI which was treated with debridement, drainage, and systemic antibiotic therapy. Two fistulas opened in the left thigh region and the patient was transferred to our hospital. The patient had pain during motion in the left hip and moderate decrease in the range of motion. Routine analyses showed leukocytosis (15.90 × 109L) and increased C-reactive protein (67.1mg/L). Radiographs of the left hip showed osteolytic zones around the acetabular and femoral components with sclerotic deformation of the distal femoral metaepiphysis (Fig. 2 and 3). Our plan was a two-stage exchange hip revision arthroplasty by performing removal of the prosthesis, implantation of an antibiotic-impregnated articulating cement spacer, and after 6 weeks of systemic antibiotic therapy– implantation of a distally-interlocked modular femoral reconstruction prosthesis due to the severe bone defects in the left femur. The operative approach was through the previous operation scar of anterolateral approach– the third fistula was found underneath the scar tissue which was connected to the greater trochanter region. Tissue samples were taken for microbiological examination. Debridement, resection of the three fistulas, removal of the femoral and acetabular componentswith the use of an osteotome,and irrigation using the pulse lavage system with physiological sodium chloride solution wereperformed.Due to the severestructural changes and a large medial wall defect in the proximal femur withimpairment of a large soft tissue zone, it was decided during operation not to put any other implants in the hip joint. All cultures from soft tissue samples collected from the hip joint region grew Staphylococcus aureus (resistant only to trimethoprim-sulfamethoxazole). The patient received antibiotic therapy with oxacillin for 16 days. On the 1stpost-operative day, the patient started physiotherapy– learned to sit in the bed and began passive exercises of the left hip joint. On the 2ndday,the patient began to stand and gradually learned to walk with crutch assistance. He was allowed touch-down weight-bearinguntil full wound healing. A soft left hip orthosis was applied to maintain muscle tone and decreaseedema. The surgical wound healed without any signs of infection and the skin clips were removed on the 14th post-operative day. The patient was discharged from the hospital and continuedantibiotic therapy with ciprofloxacin for 4 weeks. After 5 months, magnetic resonance imaging of the pelvic region showed fluid collections in the soft tissues of the left hip joint region (Fig. 4). The patient had an ultrasound-guidedleft hip joint fluid aspiration, but the acquired samples did not grow any microorganisms. After 1 year from the last surgery, the patient is relatively satisfied–he is walking with two crutches and can apply 10% of body weight on the left leg when standing. The patient has acceptable clinical results without antibiotic suppression therapy –edema in the left leg has decrease; there is no pain in the left hip region during movement and no active fistulas. C-reactive protein is 2.0mg/L.
Discussion
FD is an uncommon congenital bone disorder, in which fibrous tissue weakens the bone structure, increasing the risk of pathologic fracture, and the need for osteosynthesis. The incidence of infection following osteosynthesis of closed long bone fractures is 1–2% [5]. PJI is also a serious complication after arthroplasty associated with pain, multiple surgeries, functional incapacitation, and mortality with an incidence of 1–2% [6]. Due to the rare incidence of FD, there have not been any studies showing the overall infection rates in FD patients following osteosynthesis and arthroplasty. Increased amount of fibrous tissue and vascularity could have contributed to the rapid spread of infection through the whole bone in combination with several ineffective PJI treatment episodes.Standard goals of PJI treatment are to eliminate infection, reduce pain, and restore the normal joint function[6]. As this was a late PJI case, three options of treatment existed–one-stage implant replacement with debridement of surrounding infected soft tissues, removal of the infected, and implantation of a new prosthesis (success rates 85–90% [7]), two-stage implant replacement with debridement, removal of the prosthesis, inserting an antibiotic-impregnated cement spacer, and delayed implantation of a prosthesis (success rate more than 90% [8]), and three-stage exchange. In our hospital, two-stage exchange is the most commonly used treatment algorithm of PJI. Unfortunately, revision arthroplasty is not always successful and reinfection is a possibility that should be kept in mind. The incidence of reinfection in one- and two-stage exchange arthroplasties according to literature is 8.2% and 7.9% [9]. Another factor to be considered is the bone quality–fibrotic remodeling, osteomyelitis, repeated bone debridement, implant removal, and reimplantation had severely impaired the bone quality of the femur. Paprosky classification is based on femoral bone loss location and proposes a treatment algorithm for surgical reconstruction based on this factor [10]. By evaluating the bone quality of the left femur, this patient had a Paprosky Type IV femoral bone loss (Fig. 5a and b) that is why a distally-interlocked modular femoral reconstruction prosthesis or a proximal femoral megaprosthesis could be the appropriate solution for this case. However, these kinds of implants have poor to satisfactory functional results with increased infection rates up to 25% [11]. Since the local soft tissue and bone status were poor, the risks of impaired wound healing and infection in our opinion would outweigh the possibility of a satisfactory result. Hip arthrodesis could be an alternative option for revision arthroplasty; however, this treatment method was not acceptable for the patient since he has sedentary work and did not want to lose the mobility of the hip joint. Therefore, resection arthroplasty was a salvage procedure in this case. Nevertheless, the patient’s clinical condition has considerably improved and the infection has gone to remission. The risk of a new infection exacerbation, possible hip disarticulation, and mortality is so great that it was decided with the patient not to carry out any further operations and to continue physical activation to the possible extent.
Conclusion
Managing a recurrent PJI in a patient with poor bone quality, severe bone defects, soft tissue compromise, and thromboembolic events is challenging even for the most experienced orthopedic surgeon. Paprosky classification system can guide the surgeon in implant choice for revision hip arthroplasty. However, the final evaluation of femoral bone and soft tissue status can only be made intraoperatively after debridement and removal of the prosthesis. Therefore, treatment tactics can change. The surgeon should always consider the benefits, risks, expected results of each treatment method, and discuss them with the patient.
Clinical Message
The most important goal in PJI management is to eliminate the site of infection. If not enough radical measures are used to reduce the local bacterial count, infection will persist and result in a widespread bone and soft tissue damage. Thus, decreasing the possibilities to restore normal joint function and achieve a good result in the future. Resection arthroplasty can be a salvage treatment option in such complex cases.
References
1. Schoenau E, Rauch F. Fibrous dysplasia. Horm Res 2002;57:79-82.
2. Riddle ND, Bui MM. Fibrous dysplasia. Arch Pathol Lab Med 2013;137:134-8.
3. Chapurlat RD, Gensburger D, Jimenez-Andrade JM, Ghilardi JR, Kelly M, Mantyh P, et al. Pathophysiology and medical treatment of pain in fibrous dysplasia of bone. Orphanet J Rare Dis 2012;7 Suppl 1:S3.
4. Gupta S, Jain S, Newaskar V, Ali M. Craniofacial fibrous dysplasia with facial asymmetry, canted occlusion and open bite: A case report with 2 years follow-up. J Contemp Dent Pract2014;15:636-45.
5. Duan X, Al-Qwbani M, Zeng Y, Zhang W, Xiang Z. Intramedullary nailing for tibial shaft fractures in adults. Cochrane Database Syst Rev 2012;1:CD008241.
6. Li C, Renz N, Trampuz A. Management of periprosthetic joint infection. Hip Pelvis 2018;30:138-46.
7. Zahar A, Webb J, Gehrke T, Kendoff D. One-stage exchange for prosthetic joint infection of the hip. Hip Int 2015;25:301-7.
8. Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med 2004;351:1645-54.
9. Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD, INFORM Team. Re-infection outcomes following one- and two-stage surgical revision of infected hip prosthesis: A systematic review and meta-analysis. PLoS One 2015;10:e0139166.
10. Ibrahim DA, Fernando ND. Classifications in brief: The paprosky classification of femoral bone loss. Clin OrthopRelat Res 2017;475:917-21.
11. Racano A, Pazionis T, Farrokhyar F, Deheshi B, Ghert M. High infection rate outcomes in long-bone tumor surgery with endoprosthetic reconstruction in adults: A systematic review. Clin OrthopRelat Res 2013;471:2017-27.
 |
 |
 |
| Dr. Andris Dzerins | Dr. Matiss Zolmanis | Dr. Peteris Studers |
| How to Cite This Article: Dzerins A, Zolmanis M, Studers P. Resection Arthroplasty Treatment Possibility for a Patient with Fibrous Dysplasia, Chronic Osteomyelitis, and Recurrent Periprosthetic Hip Joint Infection: A Case Report. Journal of Orthopaedic Case Reports 2019 Jul-Aug; 9(4): 54-57. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com








