[box type=”bio”] Learning Point of the Article: [/box]
Lack of progression in rehabilitation after functional treatment of acute tendo-achilles rupture needs further clinical evaluation and investigation for rare sequalae.
Case Report | Volume 10 | Issue 2 | JOCR March – April 2020 | Page 88-91 | Sara Venturini, Marie Garbett, Linzy Houchen-Wolloff, Jitendra Mangwani. DOI: 10.13107/jocr.2020.v10.i02.1712
Authors: Sara Venturini[1], Marie Garbett[1], Linzy Houchen-Wolloff[2],[3], Jitendra Mangwani[4]
[1]Leicester Medical School, University of Leicester, Leicester, UK,
[2]Department of Physiotherapy, University Hospitals of Leicester NHS Trust, Leicester, UK,
[3]Department of Respiratory Sciences, University of Leicester, Leicester, UK,
[4]Department of Orthopaedic surgery Academic Team of Musculoskeletal Surgery, University Hospitals of Leicester NHS Trust, Leicester, UK.
Address of Correspondence:
Dr. Linzy Houchen-Wolloff,
Department of Physiotherapy, University Hospitals of Leicester NHS Trust, Glenfield Hospital, Groby Road, Leicester, LE3 9QP. UK.
E-mail: linzy.houchen@uhl-tr.nhs.uk
Abstract
Introduction: Achilles tendon rupture is common and most cases heal with appropriate treatment. However, complications in the treatment of this condition can be debilitating, especially for young, active individuals.
Case Report: We present the case of a 37-year-old man who presented with ongoing pain on weight-bearing and swelling in the left Achilles tendon area 8 months after acute rupture treated with functional bracing and early rehabilitation. Magnetic resonance imaging showed intrasubstance thickening of the tendon with a large swelling. Successful decompression of the swelling was achieved using an arthroscopic technique and the patient returned to normal activities.
Conclusion: Physiotherapy and return to normal activities were limited in our patient due to high levels of discomfort and pain. Prolonged immobility following tendon rupture has been shown to cause increased scar tissue proliferation. This may have hindered functional rehabilitation progress and negatively impacted on the reparative process.
Keywords: Orthopedics, arthroscopy, Achilles tendon.
Introduction
A rupture of the Achilles tendon is a common injury mostly affecting active people and caused by repetitive strain from running, jumping, and sudden acceleration or deceleration. Male recreational athletes in their third and fourth decades of life are the most at risk group [1]. Tears result in disruption of the conjoined tendon of the gastrocnemius and soleus muscle usually about 2–6 cm proximal to its insertion into the calcaneus [2]. Treatment for Achilles tendon rupture includes both conservative and surgical options, each with their risks and benefits. Conservative management may result in longer rehabilitation periods and potentially higher rerupture rates; however, surgical treatment carries more local complications such as infection and adhesions [1, 3, 4, 5]. Successful treatment usually results in patients returning to pre-injury levels of activity. A swelling or hematoma is fairly common at the initial presentation of a complete tendon rupture and has been described in one case of partial tendon rupture [6]. This case describes the unusual presentation of a large swelling several months following an acute complete rupture of the Achilles tendon treated with a functional rehabilitation regimen. To the best of our knowledge, this is the first case report of this complication.
Case Report
A 37-year-old man was referred due to ongoing pain in his left ankle on weight-bearing. Eight months previously, he had suffered a complete rupture of the left Achilles tendon during a martial arts session. The initial injury was treated conservatively with a VACOpedTM boot for 8 weeks and subsequent physiotherapy, following the non-operative Leicester Achilles Management Protocol functional rehabilitation regime. Physiotherapy (intrinsic muscle strengthening and range of movement exercises) was limited by significant pain. Following two physiotherapy sessions, he presented to his general practitioner with ongoing pain on the posterior aspect of the left ankle and shooting pains radiating up his calf after prolonged periods of standing. The patient reported posterior left ankle pain when weight-bearing and walking. He also complained of nighttime rest pain and morning ankle stiffness. The patient was otherwise well with a medical history of mild asthma only and no history of coagulopathies, bleeding disorders, or steroid use.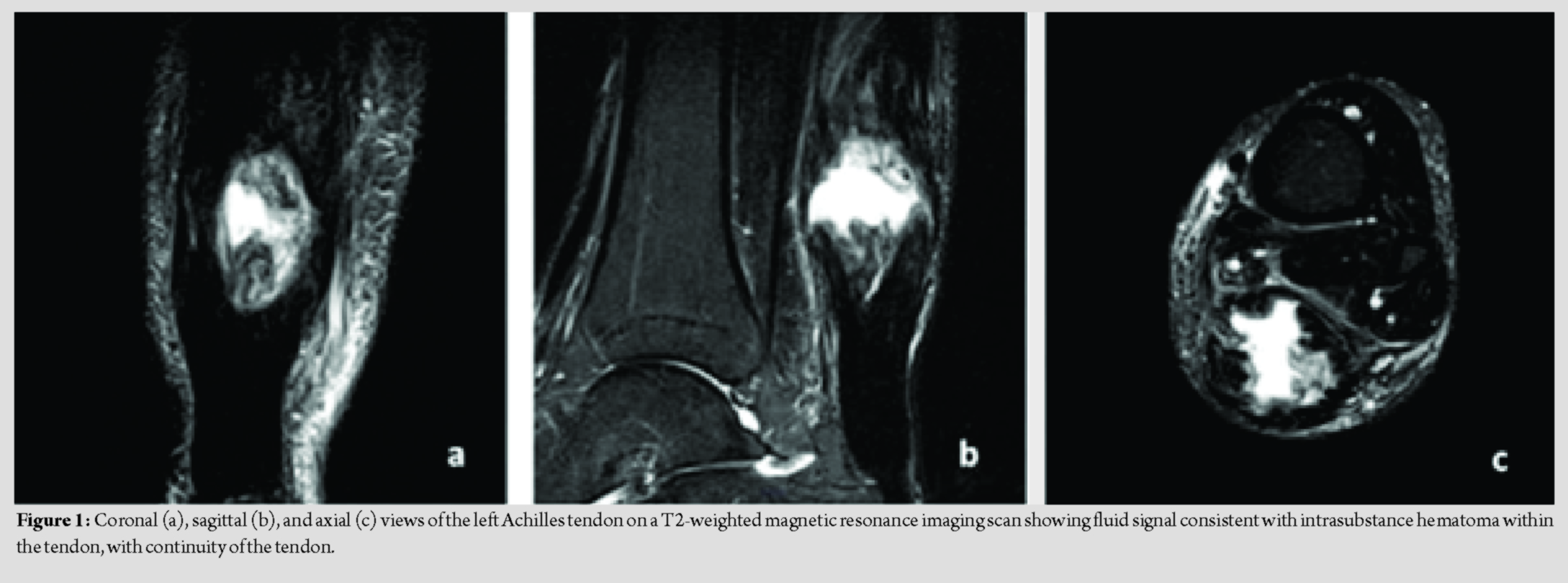
On examination, a large fusiform swelling was noted on the posterior aspect of the left ankle within his Achilles tendon. This was thought to be an organized hematoma which allowed continuity between the two ends of the tendon; continuity was demonstrated with plantar flexion elicited by performing Simmonds’ test. On palpation, a slight increase in local temperature and tenderness was noted. Dorsiflexion of the left ankle was increased by 5°compared to the right side.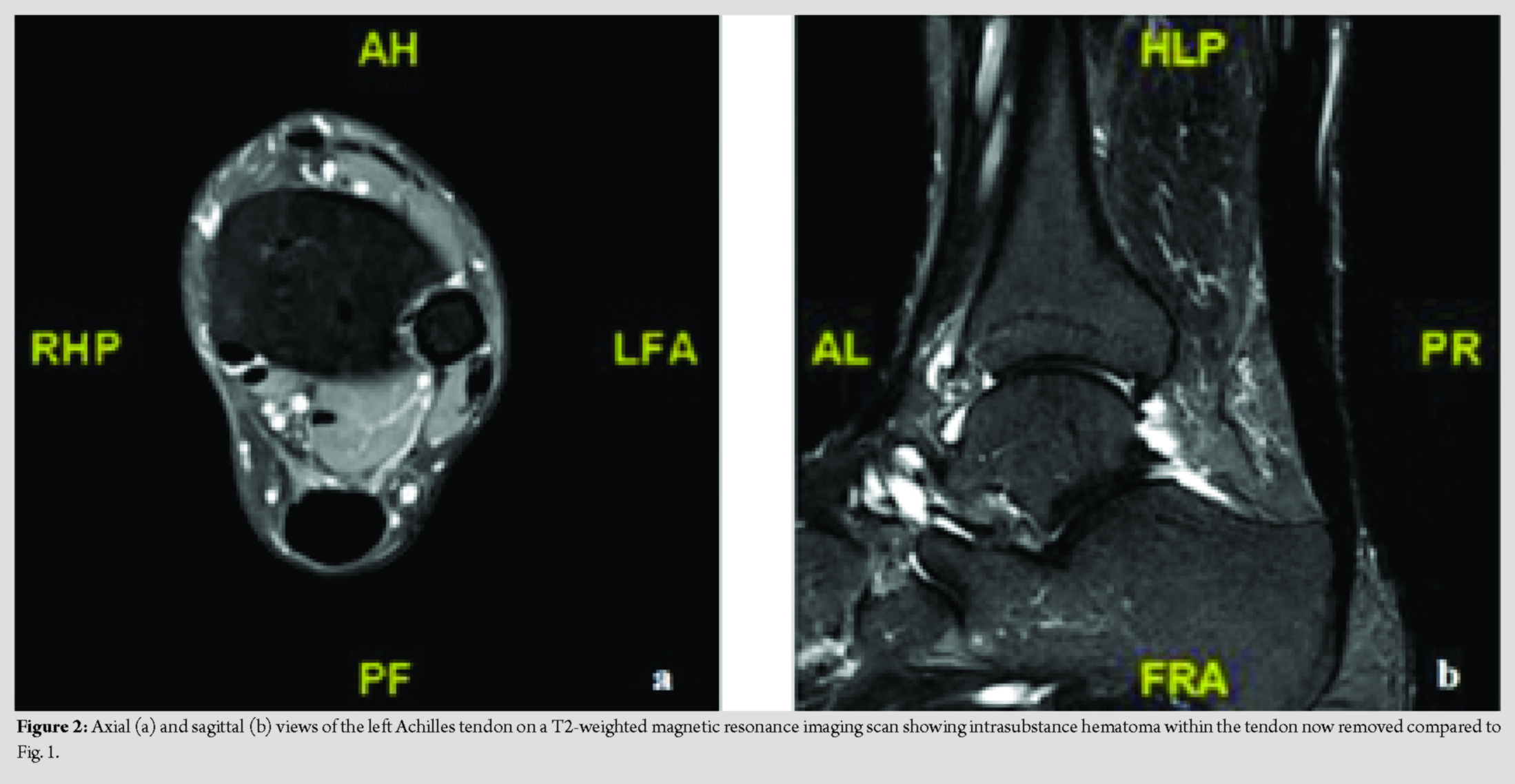
Urgent magnetic resonance imaging (MRI) was arranged due to the lack of a definitive diagnosis and to exclude infective or neoplastic causes of the swelling. The MRI scan showed a large fluid collection/hematoma intrasubstance in the Achilles tendon, located approximately 6 cm proximal from its insertion at the calcaneus, (Fig. 1). The unusual appearance of the scan prompted discussion of the case at a multidisciplinary team (MDT) meeting to guide the choice of treatment. The MDT suggested an organized hematoma or scar tissue as the most likely diagnosis; however, infection still had to be definitively excluded. The recommendation was to proceed with surgical exploration of the swelling with the aim of obtaining tissue samples for definitive diagnosis. Treatment options were discussed with the patient, including conservative treatment through to surgical intervention including synthetic options for tendon reconstruction. Following this, the decision was made to proceed with surgical arthroscopic debridement of the tendon. Needle aspiration of the swelling was performed and did not reveal a fresh hematoma. Two portals, one proximal and one distal to the swelling, were created in the left Achilles tendon. Decompression of the swelling was achieved using an arthroscopic technique. Tissue biopsies were taken for histology and microbiology. A gel-like material with scar tissue and abnormal tissue architecture was seen in this affected area of the tendon. Normal tendon tissue was visualized adjacent to the abnormal area. The histology report confirmed the specimen corresponded to tendon scar tissue with mild degenerate changes; fibro-fatty tissue was seen macroscopically. On microscopic examination, small fragments of connective tissue with mild degenerate myxoid change but no significant inflammation were noted. Postoperatively, the patient was discharged home on the same day and was advised to mobilize touch weight-bearing with crutches for 2 weeks. No external immobilization was required. Post-operative MRI views are shown in Fig. 2 with the intrasubstance hematoma now removed. At the 2-week follow-up, he was pleased with the progress, the wound was healing well and sutures were removed. Physiotherapy was started at this stage without loading exercises. At 7 weeks postoperatively, the patient was doing well with no pain, was talking no analgesia and the swelling was significantly reduced compared to preoperatively levels. He was pleased with the results of the surgery and was discharged from surgery and physiotherapy.
Discussion
Achilles tendon rupture most often occurs in the third and fourth decade of life, in athletes and in those who take part in athletic activities as a recreational pursuit. Men are affected more than women [7, 8]. If unrecognized, this common injury can be debilitating due to the associated loss of function; however, if promptly treated self-reported functional outcomes are very positive. The incidence of Achilles tendon injuries is quoted at between 5 and 10 per 100,000 of the general population and appears to be increasing [8, 9, 10, 11]. Despite this increase, the number of surgical interventions is decreasing due to increasingly availability of successful conservative management options [1, 5]. The evidence around this shift in the approach to management and the associated outcomes is varied and a definitive answer on the optimal treatment still remains a controversy. Conservative treatment options are either cast immobilization or functional bracing with early rehabilitation. Functional bracing, achieved through use of a boot with gradual reduction of plantarflexion over an 8 week period, is now preferred as it has been shown to produce better outcomes due to early mobilization and more rapid return to daily activities [12]. This functional rehabilitation protocol, encouraging early weight-bearing and mobilization, followed by physiotherapy, shows low rerupture rates [13]. Similarly, the comprehensive Swansea Morriston Achilles Rupture Treatment program, including a dedicated Achilles clinic, ultrasound examination, and the use of orthoses, early weight-bearing and an accelerated exercise regime, results in a low rate of rerupture and satisfactory outcomes with a reduced rate of surgical intervention [14]. Surgical management varies from open to minimally invasive. Recent systematic reviews suggest that surgery has a lower rerupture rate but does carry an increase drisk of complications, such as wound breakdown and infection [1]. Due to the similar outcomes in surgical and conservative approaches, surgery is usually reserved for a select group of patients with high physical demand. Pre-injury functional levels can be achieved with both treatment methods, particularly when emphasis is placed on early functional rehabilitation [15]. The common theme of physiotherapy guiding early mobility and leading to better patient outcomes is echoed throughout the literature. In this instance, conservative management of the acute rupture was chosen. Physiotherapy and return to normal activities were limited in our patient due to high levels of discomfort and pain. Prolonged immobility following tendon rupture has been shown to cause increased scar tissue proliferation [9]. This may have hindered functional rehabilitation progress and negatively impacted on the reparative process.
Conclusion
Persistent localized swelling after functional treatment of acute tendo-achilles rupture may represent an organized hematoma. MRI is the investigation modality of choice to detect this. Minimally invasive arthroscopic debridement leads to a good outcome.
Clinical Message
In this instance, physiotherapy and return to normal activities were limited in this patient due to high levels of discomfort and pain. The MDT suggested an organized hematoma or scar tissue as the most likely diagnosis; therefore, decompression of the swelling was achieved using an arthroscopic technique and normal function was resumed.
References
1. Erickson BJ, Mascarenhas R, Saltzman BM, Walton D, Lee S, Cole BJ, et al. Is operative treatment of achilles tendon ruptures superior to nonoperative treatment? A systematic review of overlapping meta-analyses. Orthop J Sports Med2015;3:232596711557918.
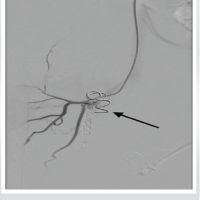
2. Lagergren C, Lindholm A. Vascular distribution in the Achilles tendon; an angiographic and microangiographic study. Acta Chir Scand 1959;116:491-5.
3. Zhang H, Tang H, He Q, Wei Q, Tong D, Wang C, et al. Surgical versus conservative intervention for acute achilles tendon rupture: A PRISMA-compliant systematic review of overlapping meta-analyses. Medicine (Baltimore) 2015;94:e1951.
4. Gulati V, Jaggard M, Al-Nammari SS, Uzoigwe C, Gulati P, Ismail N, et al. Management of achilles tendon injury: A current concepts systematic review. World J Orthop 2015;6:380-6.
5. Egger AC, Berkowitz MJ. Achilles tendon injuries. Curr Rev Musculoskelet Med 2017;10:72-80.
6. Sarsilmaz A, Varer M, Coskun G, Apaydın M, Oyar O. Partial achilles tendon rupture presenting with giant hematoma; MRI findings of 4 year follow up. Foot (Edinb)2011;21:204-6.
7. Möller A, Astron M, Westlin N. Increasing incidence of Achilles tendon rupture. Acta Orthop Scand 1996;67:479-81.
8. Leppilahti J, Puranen J, Orava S. Incidence of Achilles tendon rupture. Acta Orthop Scand 1996;67:277-9.
9. Asplund CA, Best TM. Achilles tendon disorders. BMJ 2013;346:f1262.
10. Sheth U, Wasserstein D, Jenkinson R, Moineddin R, Kreder H, Jaglal SB. The epidemiology and trends in management of acute Achilles tendon ruptures in Ontario, Canada: A population-based study of 27 607 patients. Bone Joint J 2017;99-B:78-86.
11. Huttunen TT, Kannus P, Rolf C, Felländer-Tsai L, Mattila VM. Acute Achilles tendon ruptures: Incidence of injury and surgery in Sweden Between 2001 and 2012. Am J Sports Med 2014;42:2419-23.
12. Saleh M, Marshall PD, Senior R, MacFarlane A. The Sheffield splint for controlled early mobilisation after rupture of the calcaneal tendon. A prospective, randomised comparison with plaster treatment. J Bone Joint Surg Br 1992;74:206-9.
13. Porter MD, Shadbolt B. Randomized controlled trial of accelerated rehabilitation versus standard protocol following surgical repair of ruptured Achilles tendon. ANZ J Surg 2015;85:373-7.
14. Hutchison AM, Topliss C, Beard D, Evans RM, Williams P. The treatment of a rupture of the Achilles tendon using a dedicated management programme. Bone Joint J 2015;97-B:510-5.
15. Singh D. Acute Achilles tendon rupture. BMJ 2015;351:h4722.
 |
 |
 |
 |
| Dr. Sara Venturini | Dr. Marie Garbett | Dr. Linzy Houchen-Wolloff | Dr. Jitendra Mangwani |
| How to Cite This Article: Venturini S, Garbett M, Houchen-Wolloff L, Mangwani J. Unusual Presentation of a Swelling in the Achilles Tendon After an Acute Rupture: A Case Report. Journal of Orthopaedic Case Reports 2020 Mar-Apr;10(2): 88-91. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com