[box type=”bio”] Learning Point of the Article: [/box]
Possibility of Giant cell tumor Ulna should be entertained in patients with swellings about distal forearm. Keeping in view its high recurrence rate , resection and stump stabilisation goes a long way in achieving disease free status and excellent function.
Case Report | Volume 10 | Issue 4 | JOCR July 2020 | Page 45-48 | Vipin Sharma, Kavya Sharma, Seema Sharma, Sachin Kanwar, Ravi K Soni, Punit Katoch. DOI: 10.13107/jocr.2020.v10.i04.1796
Authors: Vipin Sharma[1], Kavya Sharma[2], Seema Sharma[1], Sachin Kanwar[1], Ravi K Soni[1], Punit Katoch[1]
[1]Department of Orthopaedics, Dr. Rajendra Prasad Government Medical College, Kangra, Himachal Pradesh, India,
[2]MM Medical College, Solan, Himachal Pradesh, India
Address of Correspondence:
Dr. Vipin Sharma,
Department of Orthopaedics, Dr. Rajendra Prasad Government Medical College, Kangra, Himachal Pradesh, India.
E-mail: vipinsh_hp@rediffmail.com
Abstract
Introduction: Giant cell tumors (GCTs) of distal ulna are extremely rare accounting for 0.45%–3.2% of all the cases of GCTs. These are locally aggressive and have a higher rate of recurrence of up to 40% with conservative modality of treatment. Proximity to carpus and diminished range of motion makes their treatment a challenge.
Case Report: A 27-year-old male presented to us with swelling right distal ulna. X-ray and MRI were suggestive of GCT. The diagnosis was confirmed by core needle biopsy. The patient was managed by wide resection ulna with extensor carpi ulnaris tenodesis.
Conclusion: GCT ulna although very rare in presentation is a possible diagnosis. Wide resection of ulna is a viable treatment option to achieve disease free status. Extensor carpi ulnaris tenodesis helps stabilization of ulnar stump.
Keywords: Distal ulna, wide resection, ECU tenodesis.
Introduction
Giant cell tumor (GCT) of the bone is a rare, benign, and locally aggressive tumor of skeletally mature person, peaking in the third decade of life [1]. It accounts for 3–5% of all primary bone tumors [2] and is epimetaphyseal in location in long bones. It is accounting for about 3–5% of all primary bone tumors [2]. GCT distal ulna is very rare in incidence (0.45–3.2%) and only few cases have been reported in literature [3]. This paper described a young male who had GCT distal ulna and was managed by wide resection and ulnar stump stabilization with extensor carpi ulnaris tendon.
Case Report
A 27-year-old male, a hotel manager by profession, presented to us with a painful swelling over right distal ulna and inability to have pain free movements at wrist for the past 6 months. For initial 3 months, the swelling was peanut sized but progressed slowly thereafter. At the time of presentation, it was a walnut size swelling (3 × 2 cm) associated with dull aching pain aggravated on exertion (Fig. 1a). There was no history of trauma, fever, loss of weight, or swelling elsewhere in body. The swelling was diffusely tender and uniformly elastically hard and non-adherent to overlying skin. Movements at wrist (dorsiflexion and palmar flexion) and radioulnar joints (pronosupination) were painful and restricted. Plain X-ray of the left ulna in distal 3rd showed an expansile, multilobular, and radiolucent lesion with a clear margin. There was no periosteal reaction, but pathological fracture could be appreciated anteromedially (Fig. 1b). Other X-rays including chest and blood investigations were found to be normal. MRI revealed a lobulated expansile lesion 33 × 21 mm in dimensions, located in distal third ulna, iso to hyperintense on T1, hyperintense on T2, and STIR with thin cortices and a breach on anteromedial surface with surrounding soft-tissue enhancement (Fig. 1c and d). Core needle biopsy confirmed the lesion as GCT. Histopathology revealed multinucleate tumor giant cells with a background of mononuclear stroma. On the basis of clinical and radiographic evaluations, the lesion was found to be Campanacci Grade III lesion.
Operative steps
The patient was taken for surgery under regional anesthesia. Lateral incision was made over distal 3rd ulna subcutaneous border islanding the biopsy scar.Based on pre-operative planning based on MRI, level of osteotomy of ulna was decided at 8 cm from head of ulna (Fig. 2a). Gradually, all around dissection of tumor and distal ulna was done taking care not to injure the capsule and with a 1 cm cuff of healthy soft tissue. Care was taken to isolate and retract dorsal sensory branch of ulnar nerve. The ECU tendon was dissected free from the tumor mass and longitudinally split just proximal to the cut end of the ulna. The tendon was passed through a drill hole, 5 mm above the end of the ulnar stump in a dorsal to volar direction with the forearm held in supination. The tendon was then directed to the ulnar side and sutured back on itself, thus stabilizing ulnar stump (Fig. 2b and c). Postoperatively, the forearm and wrist were immobilized in slab for a period of 2 weeks following which gentle wrist and forearm exercises were started (Fig. 2d and e). Resected specimen was sent for histopathology and confirmed the diagnosis of GCT (Fig. 2f). At 1 year follow-up, no complications, for example, recurrence of tumor and carpus translation, were noted. The patient had a pain-free full range of dorsiflexion, palmar flexion, and pronosupination (Fig. 3).
Discussion
GCT is essentially a benign but locally aggressive tumor, located in epiphyseal region of long bones, and has the potential to metastasize to lungs [4]. A very low incidence of 0.45–3.2% but highly aggressive nature (higher than GCT radius) has been noted for GCT distal ulna [3].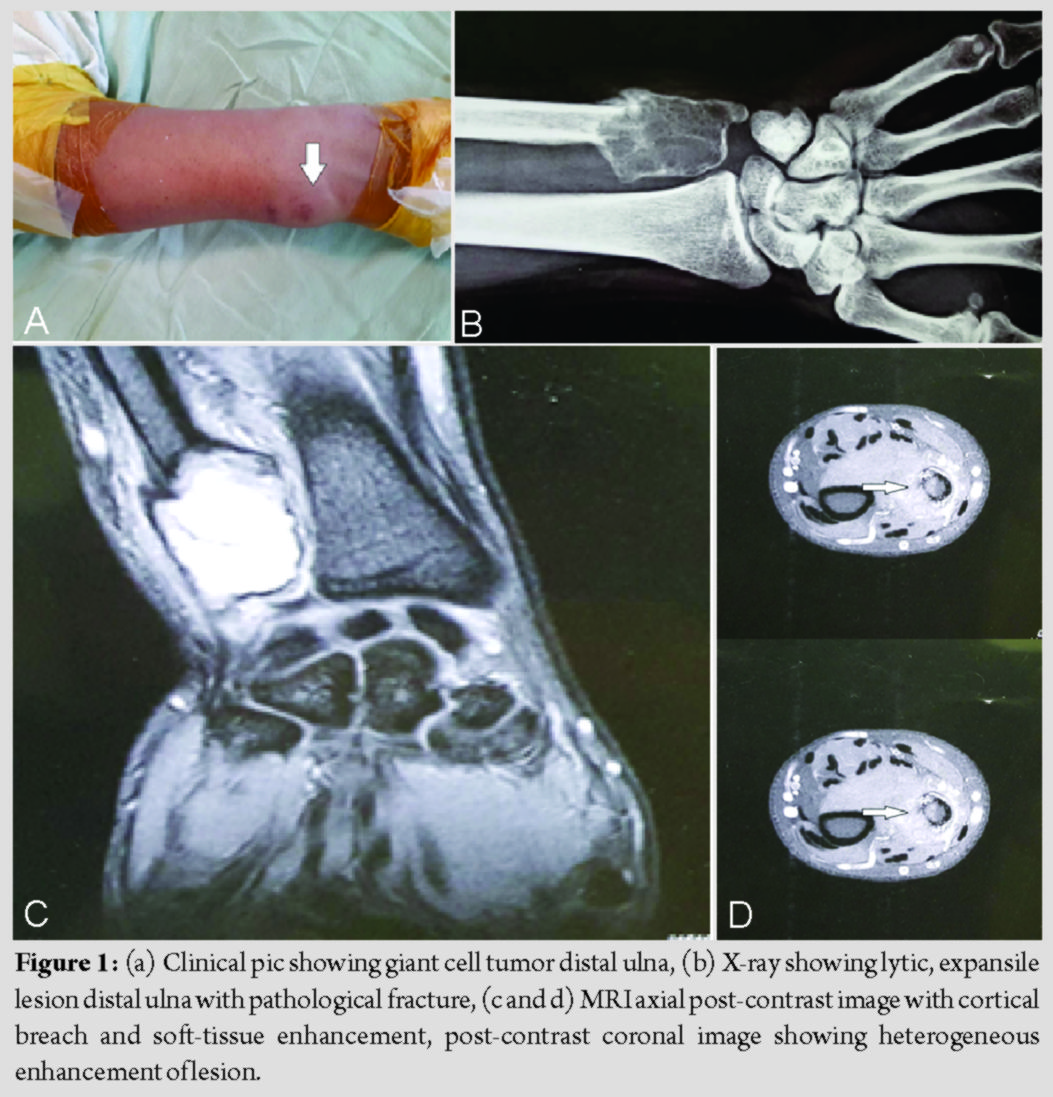
On histopathology, these tumors are well circumscribed with areas of hemorrhage and necrosis. Microscopically, these are characterized by the presence of a number of osteoclast like giant cells in a background of mononuclear stroma. Since GCT ulna is a highly aggressive tumor and has a high potential for local recurrence, the treatment of GCTs focuses on minimizing the recurrences.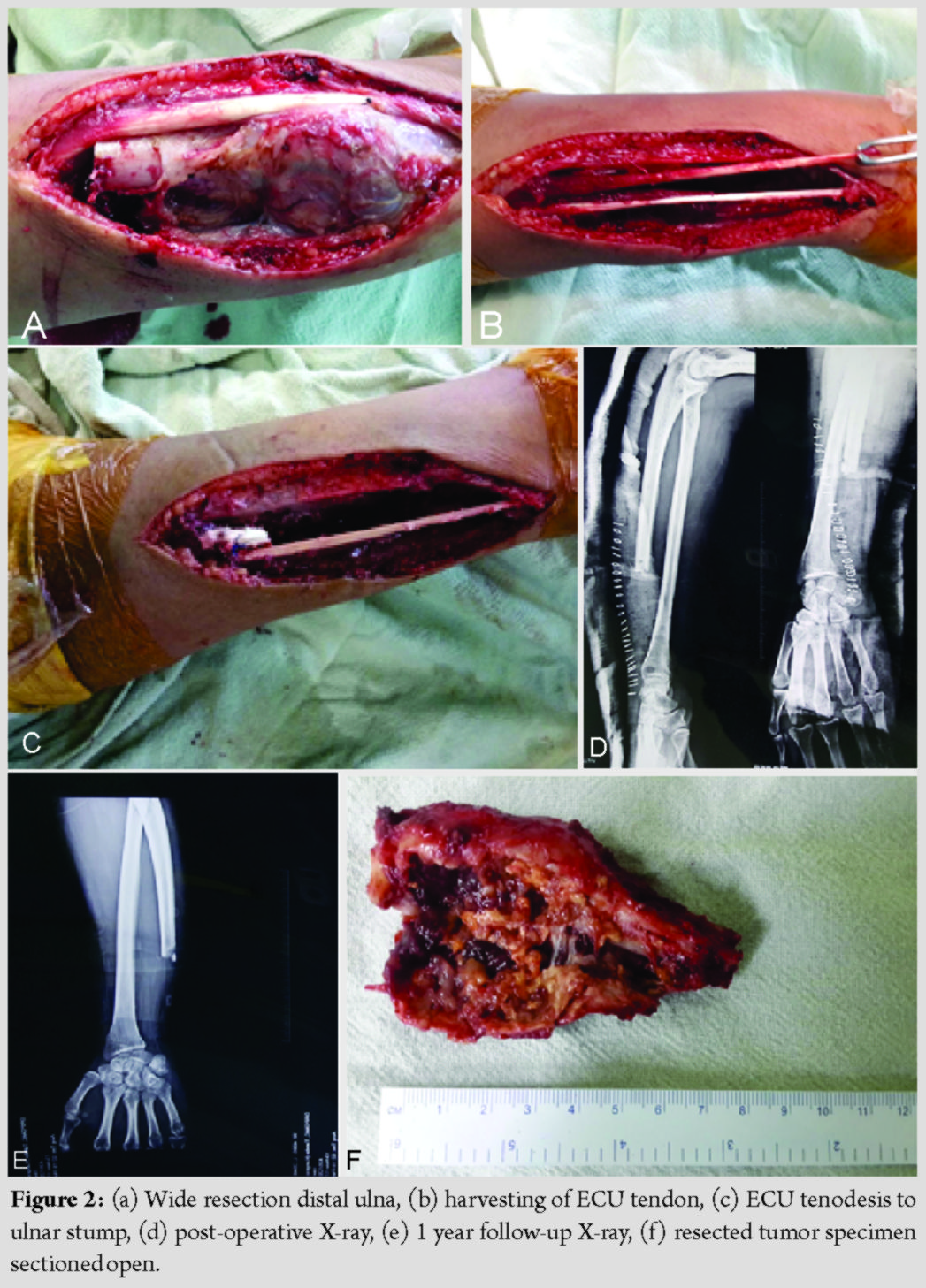
Various treatment options have been reported in literature for GCTs of ulna which range from extended curettage and bone grafting/cementation to wide resection, with or without reconstruction with allografts, prosthesis, or bone transport by Ilizarov.
Grade 1 and 2 lesions are managed nicely with extended curettage with or without adjuvants, use of adjuvants during intralesional curettage has been advocated by some, while high recurrence rates (40%) have been reported with intralesional curettage alone. Intralesional curettage with adjuvants has reported a recurrence rate of 18% [3]. Some others have stressed on adequate removal of tumor as a more important predictive factor for the outcome of surgery [5]. There is a consensus on management of Grade I and II lesions of GCT ulna in the form of curettage; [3, 6] while Grade III lesions have been managed by wide resection ulna [4]. Zhang et al. compared outcomes of curettage (Grade 1) with resection (Grade II) in GCTs distal ulna. Post-operative recurrence was found to be significantly higher in patients treated by curettage as compared to en bloc resection (P = 0.024) [7]. Higher recurrence rates in GCT ulna expose patient to an increased risk of pulmonary metastasis [8]. A six-fold increase in risk for metastasis has been reported with recurrence [9] resulting in mortality in the range of 14–23% in studies with follow-up longer than 8 years [10]. This factor also has prompted surgeons to go for wide resection in GCT ulna, especially in Enneking III lesions [11]. Literature provides a variety of options for resection distal ulna, either reconstruction or leaving ulnar stump alone. Reconstructions with allograft, prosthesis, or bone transport with Ilizarov have been reported [8, 12]. While allograft reconstruction requires bone bank facilities, Ilizarov bone transport is time consuming and use of prosthesis is limited by its availability and cost-effectiveness and possible complications like loosening. Hence, we chose resection of distal ulna followed by ulnar stump stabilization with ECU. Resection alone as a treatment option for GCT distal ulna alleviates risk of recurrence and pulmonary metastasis [8], but is known to compromise stability of carpus, radioulnar convergence, ulnar stump stability, and rarely rupture of digital extensor tendons [8, 13]. Still studies have reported excellent outcome (75%) following distal ulna resection without any reconstruction [14]. Lasso tendon graft [15], FCU, Fascia Lata autograft, or plate arthrodesis have been used in studies for stabilization of distal ulnar stump [16]. Other procedures where resection ulna is combined with ulnar buttress arthroplasty using iliac bone have also been reported [2, 17] with excellent outcome. Roidis et al. described a GCT resection with distal ulnar arthroplasty. Stabilization was achieved by suturing triangular fibrocartilage and the extensor carpi ulnaris subsheath to the stem of the prosthesis [11]. In our case, ECU tenodesis was used as a stabilization procedure for proximal ulnar stump. Initially mentioned by Goldner and Hayes in 1979 [18] and later by Kayias et al. [19] ,ECU tenodesis has been used commonly for ulnar stump stabilization following ulnar resections. One difficulty mentioned with this procedure in literature has been difficulty in separating ECU from tumor mass, but no such difficulty was faced by us while performing the procedure. In this study, ECU was longitudinally slit and a part of it was rerouted through drill hole made in proximal ulnar stump. At 1 year follow-up, the functional outcome was very good. Hence, wide resection of ulna, especially in Grade III tumors, is associated with good functional results and less recurrence rate.
Conclusion
This case highlights the fact that wide resection is a viable treatment option, especially in Grade III GCTs distal ulna. Tenodesis of ulnar stump with extensor carpi ulnaris split tendon goes a long way in stabilizing the ulnar stump and achieving a desirabl wrist function.
Clinical Message
GCT ulna is a very rare presentation. Keeping in view, the higher incidence of recurrence with these tumors, wide resection has emerged as a reasonable option to achieve a disease-free status and an optimum wrist function.
References
1. Sharma V, Sharma S, Mistry KA, Awasthi B, Verma L, Singh U. Giant cell tumor of bone in skeletally immature patients-a clinical perspective. J Orthop Case Rep 2015;5:57-60.
2. Minami A, Iwasaki N, Nishida K, Motomiya M, Yamada K, Momma D. Giant-cell tumor of the distal ulna treated by wide resection and ulnar support reconstruction: A case report. Case Rep Med 2010;2010:8712-78.
3. Vanni D, Pantalone A, Andreoli E, Caldora P, Salini V. Giant cell tumor of the distal ulna: A case report. J Med Case Rep 2012;6:143.
4. Pathak AC, Shahane SM, Samant A, Kapopara H. Unusual case of giant cell tumor indistal ulna. Astrocyte 2015;1:317-9.
5. Puri A, Agarwal M. Treatment of giant cell tumor of bone: Current concepts. Indian J Orthop 2007;41:101-8.
6. Harness NG, Mankin HJ. Giant-cell tumor of the distal forearm. J Hand Surg Am 2004;29:188-93.
7. Zhang J, Li Y, Li D, Xia J, Li S, Yu S, et al. Clinical effects of three surgical approaches for a giant cell tumor of the distal radius and ulna. Mol Clin Oncol 2016;5:613-7.
8. Burke CS, Gupta A, Buecker P. Distal ulna giant cell tumor resection with reconstruction using distal ulna prosthesis and brachioradialis wrap soft tissue stabilization. Hand (N Y) 2009;4:410-4.
9. Kay RM, Eckardt JJ, Seeger LL, Mirra JM, Hak DJ. Pulmonary metastasis of benign giant cell tumor of bone. Six histologically confirmed cases, including one of spontaneous regression. Clin Orthop Relat Res 1994;302:219-30.
10. Tubbs WS, Brown LR, Beabout JW, Rock MG, Unni KK. Benign giant-cell tumor of bone with pulmonary metastases: Clinical findings and radiologic appearance of metastases in 13 cases. AJR Am J Roentgenol 1992;158:331-4.
11. Roidis NT, Gougoulias NE, Liakou PD, Malizos KN. Distal ulnar implant arthroplasty as a definitive treatment of a recurrent giant-cell tumor. J Hand Surg 2007;32:1262-6.
12. Stoffelen D, Lammens J, Fabry G. Resection of a periosteal osteosarcoma and reconstruction using the Ilizarov technique of segmental transport. J Hand Surg Br 1993;18:144-6.
13. Naik MA, Sujir P, Rao SK, Tripathy SK. Ulnar buttress arthroplasty after enbloc resection of a giant cell tumor of the distal ulna. Indian J Orthop 2013;47:211-4.
14. Cooney WP, Damron TA, Sim FH, Linscheid RL. En bloc resection of tumors of the distal end of the ulna. J Bone Joint Surg 1997;79:406-12.
15. Gainor BJ. Lasso stabilization of the distal ulna after tumor resection: A report of two cases. J Hand Surg Am 1995;20:324-6.
16. Ferracini R, Masterson EL, Bell RS, Wunder JS. Distal ulnar tumours: Results of management by en bloc resection in nine patients and review of the literature. J Hand Surg 1988;23:517-21.
17. Hashizume H, Kawai A, Nishida K, Sasaki K, Inoue H. Ulnar buttress arthroplasty for reconstruction after resection of the distal ulna for giant cell tumour. J Hand Surg Br 1996;21:213-5.
18. Goldner JL, Hayes MG. Stabilization of the remaining ulna using one-half of the extensor carpi ulnaris tendon after resection of the distal ulna. Orthop Trans 1979;3:330-1.
19. Kayias EH, Drosos GI, Anagnostopoulou GA. Resection of the distal ulna for tumours and stabilisation of the stump. A case report and literature review. Acta Orthop Belg 2006;72:484-91.
 |
 |
 |
 |
 |
| Dr. Vipin Sharma | Dr. Kavya Sharma | Dr. Sachin Kanwar | Dr. Ravi K Soni | Dr. Punit Katoch |
| How to Cite This Article: Sharma V, Sharma K, Sharma S, Kanwar S, Soni RK, Katoch P. Resection and Stump Stabilization in Giant Cell Tumor Distal Ulna: A Case Report. Journal of Orthopaedic Case Reports 2020 July;10(4): 45-48. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com




