[box type=”bio”] Learning Point of the Article: [/box]
Anterior release through the standard anterior cervica approach with posterior fixation is a valid option to be considered for the management of neglected odontoid fractures.
Case Report | Volume 10 | Issue 5 | JOCR August 2020 | Page 20-23 | Anandkumar Khatavi, Charanjit Singh Dhillon, Nilay Chhasatia, Chetan Shashikant Pophale, Narendra Reddy Medagam. DOI: 10.13107/jocr.2020.v10.i05.1820
Authors: Anandkumar Khatavi[1], Charanjit Singh Dhillon[1], Nilay Chhasatia[1], Chetan Shashikant Pophale[1], Narendra Reddy Medagam[1]
[1]Department of Spine Surgery, MIOT Hospitals, Chennai, Tamil Nadu, India.
Address of Correspondence:
Dr. Anandkumar Khatavi,
Department of Spine Surgery, MIOT Hospitals, Sathya Nagar Road, Porur, Manapakkam, Chennai. Tamil Nadu, India.
E-mail: anandkhatavi@gmail.com
Abstract
Introduction: While odontoid fractures frequently lead to non-union in elderly population,they are relatively rare in the younger age group. We present our management of a rare case of neglected odontoid fracture in an ankylosed spine of a young female.
Case Report: A 28-year-old female presented to our emergency department with neck deformity after a history of fall 1 year back. She presented with clinical symptoms and signs of cervical myelopathy. Diagnostic imaging confirmed ankylosis of the cervical spine with a non-union of the odontoid fracture with atlantoaxial instability and kyphosis. She was treated with anterior release of the odontoid through a standard Smith-Robinson approach, anatomical reduction, and posterior occipitocervical stabilization and fusion.
Conclusion: Non-union with a malpsitioned odontoid fracture in an ankylosed spine can be addressed by an anterior release and reduction with posterior fusion with good functional outcome.
Keywords: Non-union, odontoid, ankylosis, cervical spine, myelopathy, anterior release.
Introduction
Ankylosing spondylitis (AS) is a progressive, systemic, inflammatory spondyloarthropathy typically affecting the subaxial spine. Cervical spine involvement has been reported in 75% of AS patients [1]. Patients with long-standing AS are 3.5 times more likely to sustain a cervical spine fracture compared to the general population, with a mortality rate of 35%. The majority of these fractures involve the subaxial cervical spine. Upper cervical spine injuries are relatively rare among these patients [2, 3]. Although the numbers of missed fractures are decreasing due to better availability of computed tomographic (CT) scan and magnetic resonance imaging (MRI) [4], injuries of the cervicothoracic junction and the occipitocervical region are still frequently missed due to the absence of neurological symptoms, complex anatomy, suboptimal radiographic images, and low index of suspicion to obtain CT/MRI scans in indicated cases [5, 6, 7]. Neglected odontoid fractures can seldom affect the neurology of the patient. Surgical management of these patients with the symptoms of cervical myelopathy is challenging. We present a novel technique for the reduction and stabilization of neglected odontoid fracture with kyphosis in a case of ankylosed spine.
Case Report
A 28-year-old female presented to the emergency department with neck pain, difficulty in balance while walking, and restricted neck range of motion for the past 6 months. She was a diagnosed case of AS not under regular follow-up. She had sustained injury to her neck, 1 year back due to a fall which was managed conservatively. On examination, she had near-complete restriction of neck movements and weakness of her right-hand grip, Medical Research Council (MRC) Grade 3. Rest of the myotomes of the upper lims and lower limbs scored MRC Grade 5. She also had signs of cervical myelopathy,that is, exaggerated deep tendon reflexes, spasticity in the both upper and lower limbs, Hoffman’s and Babinskis signs were positive and the patient was unable to walk tandem. Sensations in both upper and lower limbs were normal. Her bowel and bladder habits were normal and modified Japanese Orthopedic Association score was 15. Radiographs revealed a fixed anterior subluxation of the atlas over the axis and kyphosis of 20° between C1 and C2 (Fig. 1a). CT scans revealed non-union of Type II odontoid fracture with subluxation and arthritis of the atlantoaxial joint (Fig. 1b). CT also demonstrated ankylosis of the occipitocervical joint and the facet joints of the subaxial cervical spine. MRI revealed cord compression at the craniocervical junction and cord edema at C1-C2 level (Fig. 1c). CT angiography revealed normal flow in both the vertebral arteries.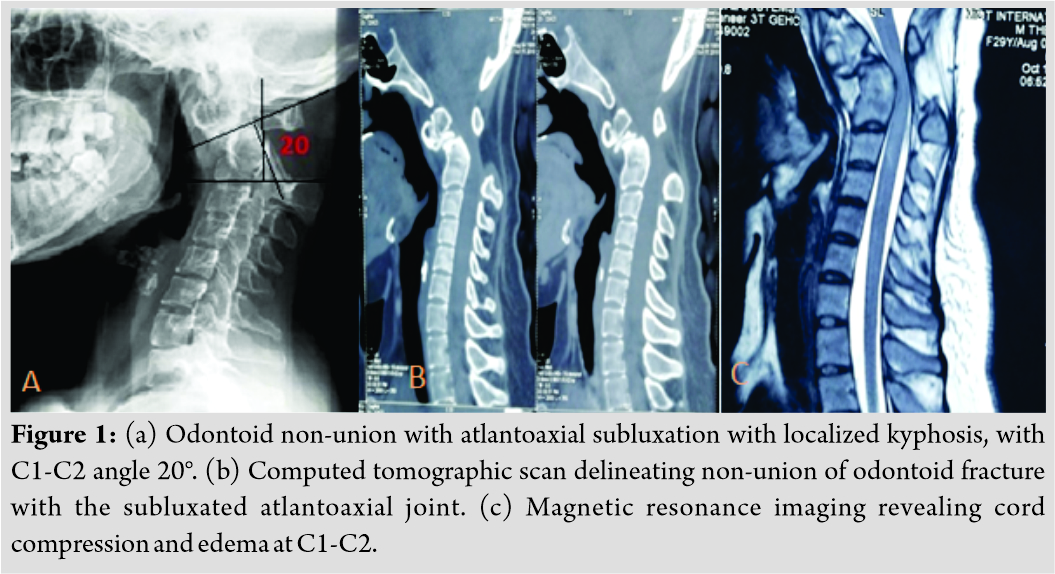
In view of her neurological deficits, an anterior release of the non-union of odontoid was planned followed by posterior stabilization and occipitocervical fusion.
Surgical technique
With the patient in the supine position, the Smith-Robinson approach to the cervical spine was performed through a horizontal skin incision at the C5-C6 level. Following this, the anteriorly subluxated arch of C1 was palpated, and the non-union site was marked with a K-wire under fluoroscopy guidance. An osteotome was then gently advanced into the non-union site under fluoroscopy guidance, and osteoclasis was performed (Fig. 2a and b). Care was taken to avoid inadvertant injury to the cord. Once osteoclasis was performed, rest of the adhesions were released from the anterior aspect of the spine. The cervical spine was repositioned in gentle lordosis under fluoroscopic guidance, and satisfactory restoration of alignment of C1-C2 was confirmed.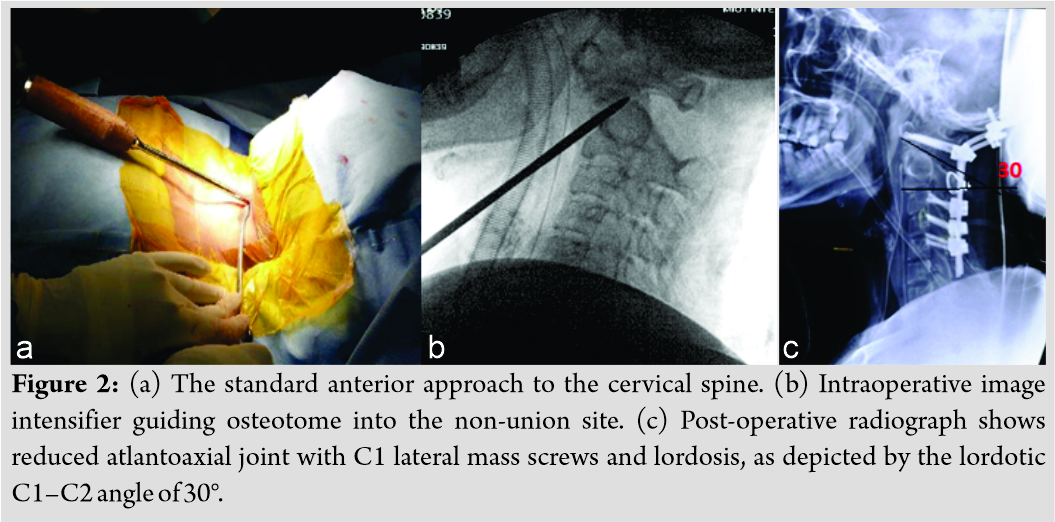
The patient was then positioned prone using the Mayfield’s clamp. The adequate reduction was ensured under fluoroscopic guidance. The standard posterior approach was performed to expose the atlantoaxial and occipitocervical region. C1-C2 joint was curetted, wedge-shaped bone graft was placed and fusion performed along with posterior fusion from occiput to C5 using occipital plate and lateral mass screws at C1, C3, C4, and C5. C1-C2 joint was reduced using DCER (distraction, compression, extension, and reduction) technique; hence, decompression was deferred as joint was reduced anatomically [8]. Sublaminar wires were used at the C2 lamina. The construct was stabilized with pre-bent rods. Posterior fusion was performed using cancellous graft chips obtained from the right posterior iliac crest (Fig. 2c). The post-operative period was uneventful, and the patient was advised to use the soft cervical collar for 3 months. By the end of 3 months, she recovered significantly from her myelopathic symptoms. CT scan performed at the end of 1 year demonstrated a well-reduced atlantoaxial joint adequate space available for cordand a maintained cervical sagittal alignment with sound fusion at C1-C2 joint (Fig. 3a and b).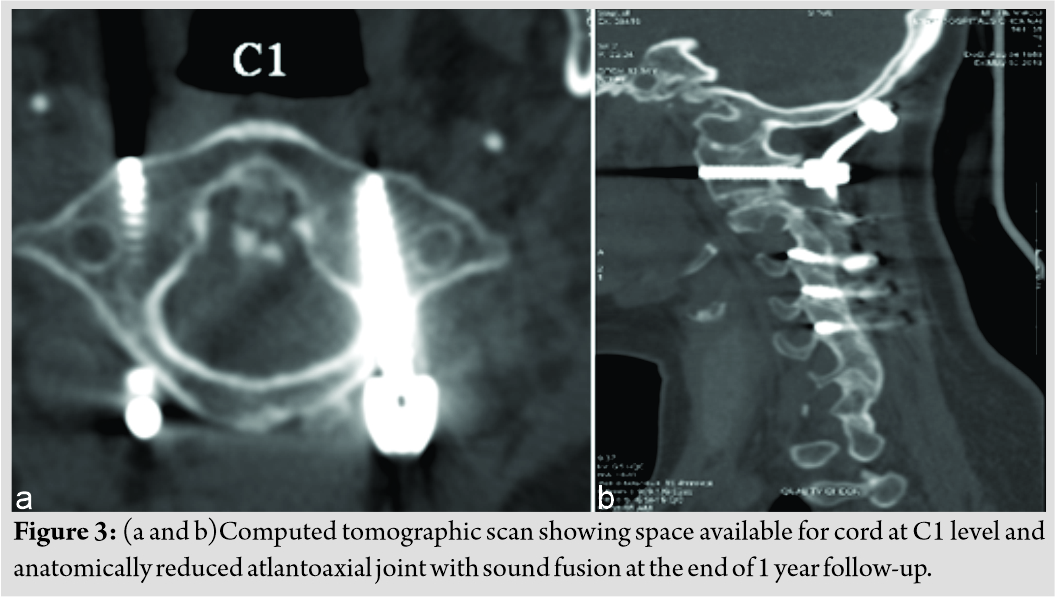
Discussion
Ankylosed cervical spine results in a long lever arm, with a 5-fold higher risk of spine fractures in comparison to the healthy population [9]. Delay in diagnosis is due to the often trivial nature of injury resulting in a fracture and junctional anatomical locations such as the occipitocervical and cervicothoracic junctions [7]. Odontoid fractures are relatively rare in ankylosed spine, and the consensus regarding the treatment options is yet to be achieved [2]. Giannoudis et al.[10] reported a significant association between non-union and NSAIDs, which are frequently used in the symptomatic management of spondyloarthropathies. Furthermore, osteoporosis associated with AS may also alter the process of fracture healing [11]. The reported incidence of non-union of odontoid fracture varies from 26% to 76% [12]. The probable explanations for the non-union are numerous. The inadequate vascular supply to the waist of the odontoid is a crucial contributory factor. If left untreated, C1 eventually loses its support from the C2 superior articular process due to the degeneration of the facet joints and its sequelae. Subsequently, the muscles and soft-tissue anterior to the craniovertebral junction contract and shorten. In addition to the soft-tissue contractures, bony changes develop overtime and play a role in the irreducibility of the fracture. The articular surfaces of C1–C2 may become gradually more vertical and arthritic. The union may prevent the reduction of C1 over C2. Our patient had AS; she not only presented with the arthritis of the C1-C2 joint, but the rest of her subaxial cervical spine was ankylosed. Often, these injuries cannot be treated with conventional surgical techniques and require improvised approaches. Multiple treatment options have been reported in literature. Reports of anterior odontoidectomy followed by posterior fusion have shown satisfactory outcomes [13,14], especially with the advent of microsurgical techniques. However, the transoral odontoid resection has a steeper learning curve and carries a small but significant risk of dural tear leading to meningitis. In transoral odontoidectomy, it is difficult to correct the kyphosis and reduce the C1-C2 joint, which may result in a swan neck deformity [15]. Wang et al. reported excellent results with the transoral release of the odontoid followed by posterior fusion, even in severe atlantoaxial dislocations [15]. The anterior release can be done transorally or through the retropharyngeal approach. The crucial advantage of this technique is the anatomical reduction and prevention of progressive neck deformity. Furthermore, the complications associated with dural tears are avoided. Microendoscopic anterior release and video-assisted transcervical release have also been reported in recent literature [15, 16]. Goel et al. described posterior atlantoaxial joint release and distraction for irreducible atlantoaxial dislocations. However, it works well only in the less severe irreducible dislocations [17]. This procedure of posterior distraction falls short in addressing the anterior tether in chronically dislocated joints. Rishi et al. described the single-stage anterior release of atlantoaxial joint along with contracted muscles and followed by posterior stabilization for neglected odontoid fracture with atlantoaxial dislocation [18]. In the present case, we performed the release of odontoid through the standard anterior retropharyngeal approach followed by posterior stabilization and fusion with an occipital plate and lateral mass screws. At the end of 6 months follow-up, radiographs demonstrated sound fusion with satisfactory cervical alignment. The patient had complete neurological recovery.
Conclusion
Anterior release and posterior fusion can provide sufficient decompression, adequate deformity correction, and sound fusion in cases with neglected odontoid fractures in the ankylosed spine while avoiding the pitfalls associated with the odontoidectomy. Our technique of anterior release of the odontoid (using standard anterior approach) with posterior fusion has shown good clinical outcome and anatomical restoration of sagittal alignment.
Clinical Message
Irreducible atlantoaxial dislocation is addressed by anterior and posterior approach. The described technique avoids the complications of transoral surgeries. One should be vigilant in releasing the adhesions anteriorly to reduce the joint in anatomical position.
References
1. Wilkinson M, Bywaters EG. Clinical features and course of ankylosing spondylitis; as seen in a follow-up of 222 hospital referred cases. Ann Rheum Dis 1958;17:1209-28.
2. Vosse D, Feldtkeller E, Erlendsson J, Geusens P, van der Linden S. Clinical vertebral fractures in patients with ankylosing spondylitis. J Rheumatol 2004;31:1981-5.
3. Graham B, Van Peteghem PK. Fractures of the spine in ankylosing spondylitis: Diagnosis, treatment, and complications. Spine (Phila Pa 1976) 1989;14:803-7.
4. Heyde CE, Fakler JK, Hasenboehler E, Stahel PF, John T, Robinson Y, et al. Pitfalls and complications in the treatment of cervical spine fractures in patients with ankylosing spondylitis. Patient Saf Surg 2008;2:15.
5. Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: A systematic review of the literature on treatment, neurological status and complications. Eur Spine J 2009;18:145-56.
6. Caron T, Bransford R, Nguyen Q, Agel J, Chapman J, Bellabarba C. Spine fractures in patients with ankylosing spinal disorders. Spine (Phila Pa 1976) 2010;35:E458-264.
7. Tan E, Schweitzer ME, Vaccaro L, Spetell AC. Is computed tomography of nonvisualized C7-T1 cost-effective? J Spinal Disord 1999;12:472-6.
8. Chandra PS, Bajaj J, Singh PK, Garg K, Agarwal D. Basilar invagination and atlantoaxial dislocation: Reduction, deformity correction and realignment using the dcer (distraction, compression, extension, and reduction) technique with customized instrumentation and implants. Neurospine 2019;16:231-50.
9. Prieto-Alhambra D, Mun˜oz-Ortego J, De Vries F, Vosse D, Arden NK, Bowness P, et al. Ankylosing spondylitis confers substantially increased risk of clinical spine fractures: A nationwide case-control study. Osteoporos Int 2015;26:85-91.
10. Giannoudis PV, MacDonald DA, Matthews SJ, Smith RM, Furlong AJ, De Boer P. Nonunion of the femoral diaphysis. The influence of remaining and non-steroidal anti-inflammatory drugs. J Bone Joint Surg Br 2000;82:655-8.
11. Giannoudis P, Tzioupis C, Almalki T, Buckley R. Fracture healing in osteoporotic fractures: Is it really different? A basic science perspective. Injury 2007;38:S90-9.
12. Pal D, Sell P, Grevitt M. Type II odontoid fractures in the elderly: An evidence-based narrative review of management. Eur Spine J 2011;20:195-204.
13. Jain VK, Behari S, Banerji D, Bhargava V, Chhabra DK. Transoral decompression for craniovertebral osseous anomalies: Perioperative management dilemmas. Neurol India 1999;47:188-95.
14. Tuite GF, Veres R, Crockard HA, Sell D. Pediatric trans oral surgery: Indications, complications, and long-term outcome. J Neurosurg 1996;84:573-83.
15. Wu YS, Chi YL, Wang XY, Xu HZ, Lin Y, Mao FM, et al. Microendoscopic anterior approach for irreducible atlantoaxial dislocation: Surgical techniques and preliminary results. J Spinal Disord Tech 2010;23:113-20.
16. Liu T, Li F, Xiong W, Du X, Fang Z, Shang H, et al. Video-assisted anterior transcervical approach for the reduction of irreducible atlantoaxial dislocation. Spine (Phila Pa 1976) 2010;35:1495-501.
17. Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine 2004;1:281-6.
18. Rishi AA, Rathod AK, Chaudhary KS. Irreducible atlanto-axial dislocation in neglected odontoid fracture treated with single stage anterior release and posterior instrumented fusion. Asian Spine J 2016;10:349-54.
 |
 |
 |
 |
 |
| Dr. Anandkumar Khatavi | Dr. Charanjit Singh Dhillon | Dr. Nilay Chhasatia | Dr. Chetan Shashikant Pophale | Dr. Narendra Reddy Medagam |
| How to Cite This Article: Khatavi A, Dhillon CS, Chhasatia N, Pophale CS, Medagam NR. Management of Neglected Odontoid Fracture in the Ankylosed Spine: A Case Report and Technical Note. Journal of Orthopaedic Case Reports 2020 August;10(5): 20-23. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com








