[box type=”bio”] Learning Point of the Article: [/box]
Any solitary lytic lesion of vertebral body should carry a high degree of suspicion of solitary plasmacytoma and requires a thorough investigation followed by appropriate treatment to prevent progressive kyphosis and neurological deterioration.
Case Report | Volume 10 | Issue 6 | JOCR September 2020 | Page 23-27 | Nagaraj Manju Moger, Syed Ifthekar, Kaustubh Ahuja, Samarth Mittal, J Pragadeeshwaran, Pankaj Kandwal. DOI: 10.13107/jocr.2020.v10.i06.1860
Authors: Nagaraj Manju Moger[1], Syed Ifthekar[1], Kaustubh Ahuja[1], Samarth Mittal[1], J Pragadeeshwaran[1], Pankaj Kandwal[1]
[1]Department of Orthopaedics, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
Address of Correspondence:
Dr. Pankaj Kandwal,
Department of Orthopaedics, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
E-mail: pankajkandwal27@gmail.com
Abstract
Introduction: Malignant bone tumors of the spine are extremely rare with an incidence of 0.05% of primary neoplasms. Solitary plasmacytoma of the vertebra accounts for about 30% of the total within this group.
Case Presentation: A 23-year-old female presented to spine clinic, with complaints of low back pain, deformity in lower back, and difficulty in walking for 3 months duration. Radiological investigations revealed destruction of L3 vertebra with soft-tissue mass around it. USG-guided biopsy from the lesion was suggestive of plasma cell dyscrasia. Routine blood investigations showed no abnormality. Urine myeloma profile and immunoelectrophoresis were done which were within normal limit and ruled out multiple myeloma. Due to the profound neurological deficit and existing instability, the patient underwent decompression, resection of tumor, anterior column reconstruction with cage, and instrumented posterior and posterolateral fusion (360° fusion) from L1-L5, before radiotherapy. The patient was subjected to 23 cycles of intensity-modulated radiotherapy and is doing good on subsequent follow-ups with good fusion.
Conclusion: Solitary plasmacytoma of vertebra when associated with neurological deficit and/or instability should be treated with spinal stabilization surgery followed by radiotherapy to achieve good and overall predictable outcomes.
Keywords: Plasma cell dyscrasias, solitary plasmacytoma, 360° fusion spine surgery.
Introduction
Solitary plasmacytoma of bone (SPB) is an uncommon plasma cell dyscrasia with an incidence of 2–5%. SPB is characterized with the proliferation of neoplastic plasma cells in localized bone (osseous – 69%) and soft tissue (extramedullary –31%). Involvement of axial skeleton (spine – 68.5%) is the most common presentation of the osseous type of plasmacytoma [1, 2]. The common symptoms of spinal SPB are pain, kyphotic deformity, vertebral instability, and sensory and motor deficits as the disease progresses. Here, we report a case of SPB, which presented with progressive pain, deformity, and neurological deficit.
Case Report
A 23-year-old female presented to the spine clinic of a tertiary teaching hospital with complaints of low back pain (VAS -– 8/10) for 3 years. The patient had a Deformity in the lower back and difficulty in walking for 3 months duration. Low back pain was insidious in onset, progressive in intensity, more during night time and relieved on taking medication. Deformity in low back was noticed by parents which gradually progressed to the presenting state. There was weakness in bilateral lower limbs with difficulty in walking and sensory disturbances in the form of tingling and numbness over the areas of both lower limbs for three 3 months as described in the clinical examination below. There were no complaints suggestive of of bowel and bladder involvement. On examination, there was visible knuckle deformity in the mid lumbar region which was tender on direct palpation (Fig. 1 ). The neurological evaluation of the patient is as shown in the (Table 1) below.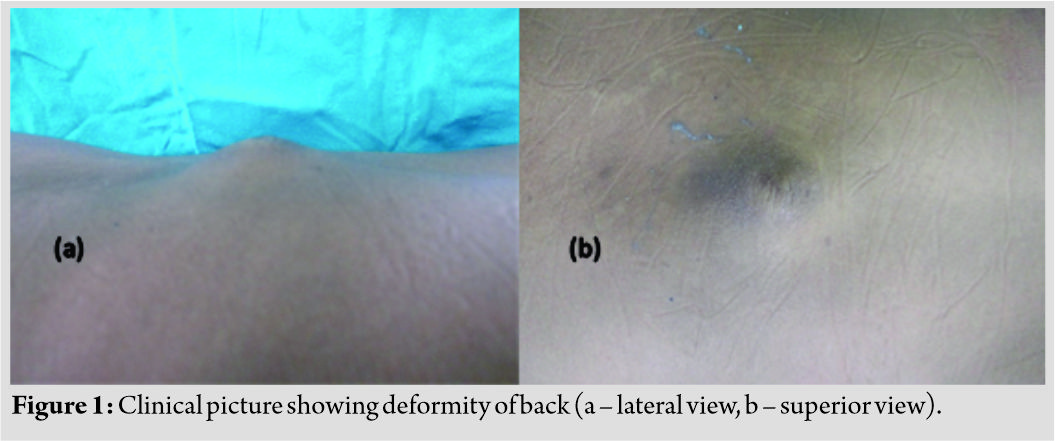
Knee, ankle, and plantar reflexes were absent bilaterally and graded sensory loss was seen over L3, L4, L5, and S1 dermatomes bilaterally. The patient had had X-rays taken at the interval of three 3 months, before presentation to our OPD which showed the evolution of the involvement of vertebra from a lytic lesion to complete collapse and dislocation ( Fig. 2). NCCT scan showed destruction of L3 body with only remnants of endplates seen with a point contact between L2-L4 and dislocation of L3-L4 facet joint (Fig. 3).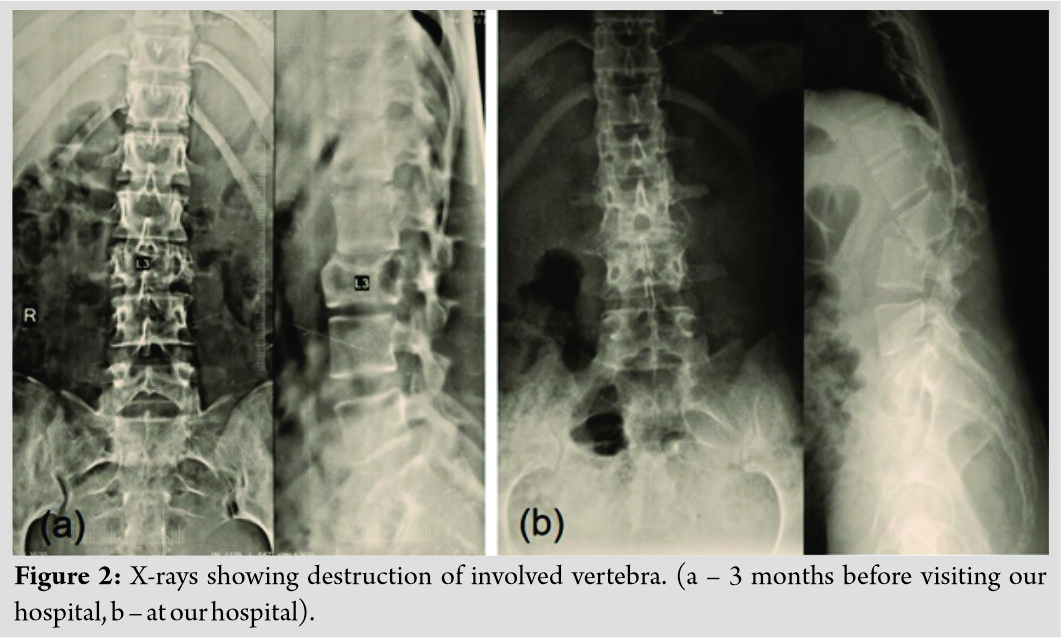 MRI revealed that a homogeneous mass was at the level of L3L4 L3L4 and on either side of the pedicles of L4 with obliteration of bilateral neural foramina. The lesion and mass were hypointense on T1- weighted images and iso to hyperintense on T2 weighted and in contrast images. There was also considerable compression on the thecal sac at the level of L3 (Fig. 4).
MRI revealed that a homogeneous mass was at the level of L3L4 L3L4 and on either side of the pedicles of L4 with obliteration of bilateral neural foramina. The lesion and mass were hypointense on T1- weighted images and iso to hyperintense on T2 weighted and in contrast images. There was also considerable compression on the thecal sac at the level of L3 (Fig. 4).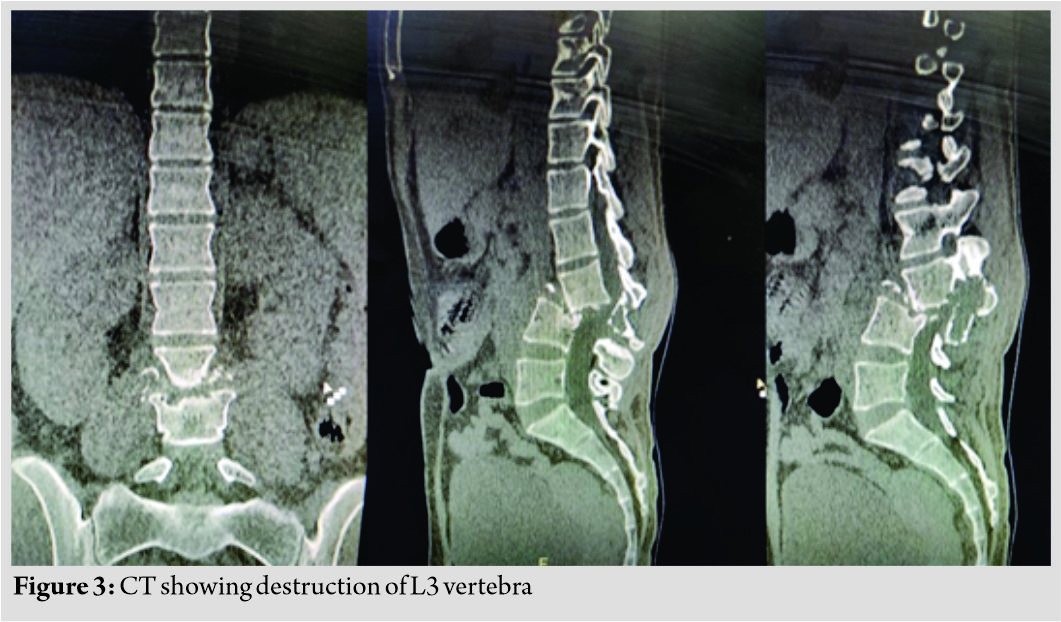 USG- guided biopsy was done from the lesion and was suggestive of plasma cell dyscrasia. Routine blood investigations showed no abnormality. Complete multiple myeloma workup was done in the form of serum myeloma profile, urine for Bence Jones proteins, and serum immunoelectrophoresis.
USG- guided biopsy was done from the lesion and was suggestive of plasma cell dyscrasia. Routine blood investigations showed no abnormality. Complete multiple myeloma workup was done in the form of serum myeloma profile, urine for Bence Jones proteins, and serum immunoelectrophoresis.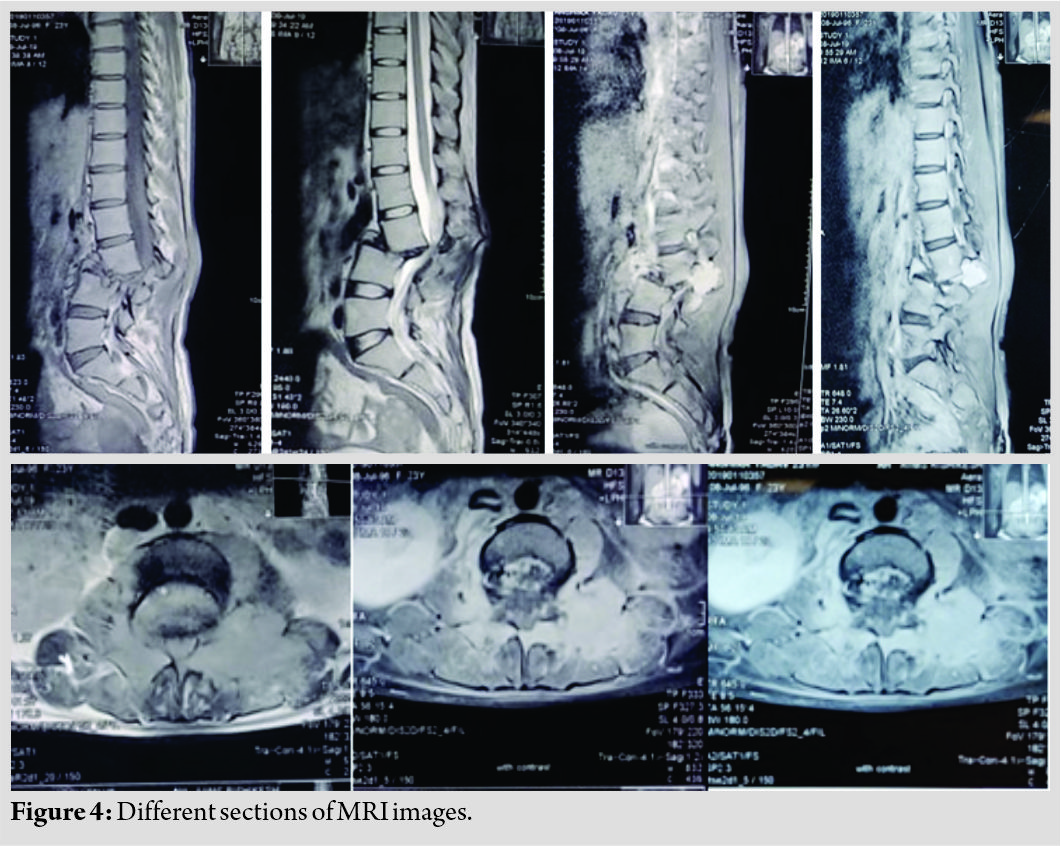 The workup was normal and did not suggest multiple myeloma. Owing Due to the profound neurological deficit and existing instability, the patient was offered decompression, correction of deformity, and instrumented spinal stabilization followed by radiotherapy. The patient underwent decompression, resection of tumour, anterior column reconstruction with cage, and instrumented posterior and posterolateral fusion (360° fusion) from L1- L5 (Fig. 5, 6).
The workup was normal and did not suggest multiple myeloma. Owing Due to the profound neurological deficit and existing instability, the patient was offered decompression, correction of deformity, and instrumented spinal stabilization followed by radiotherapy. The patient underwent decompression, resection of tumour, anterior column reconstruction with cage, and instrumented posterior and posterolateral fusion (360° fusion) from L1- L5 (Fig. 5, 6).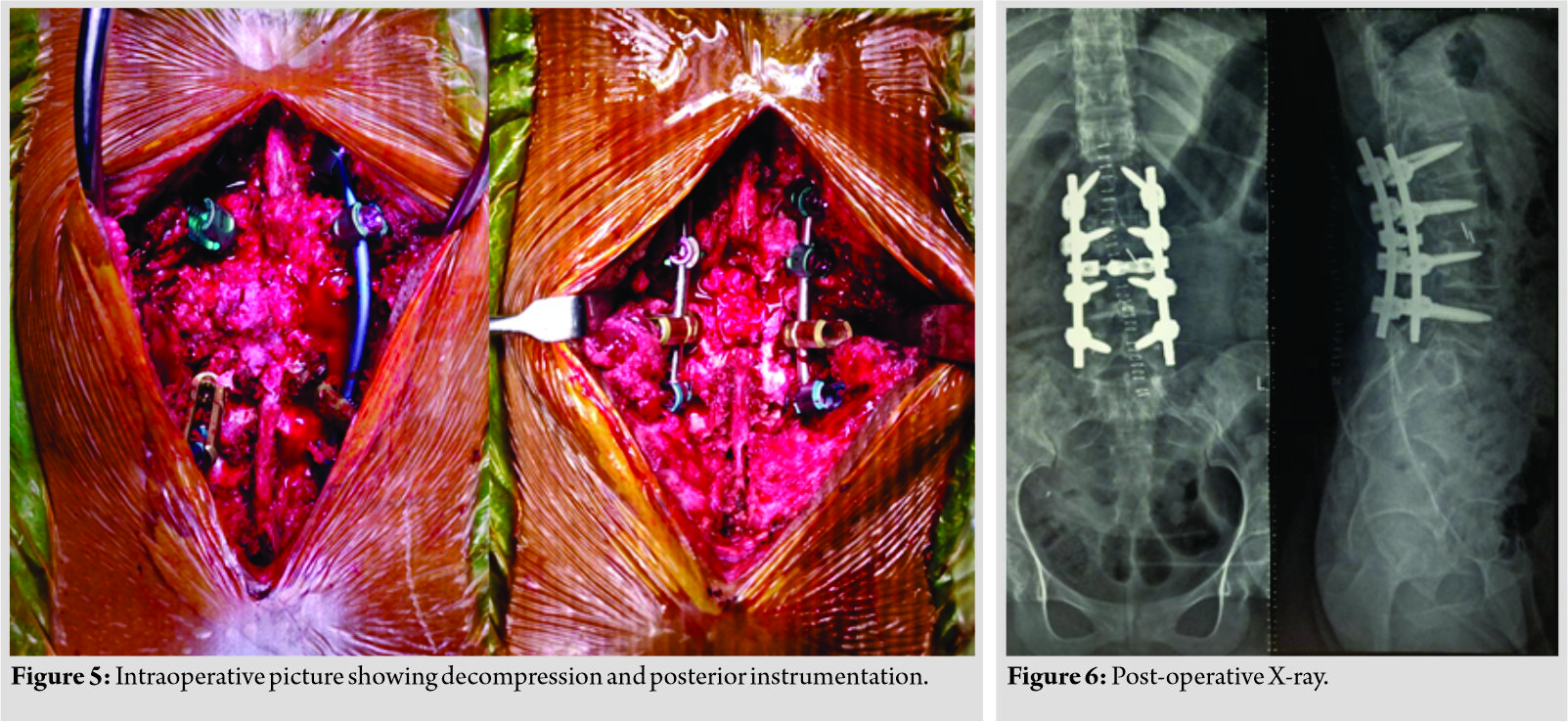 Extensive physiotherapy and passive range of movements of lower limbs were started immediately in the post-operative period. An ankle-foot orthosis was given to prevent equinus deformity at the ankle. The patient was subjected to 23 cycles of intensity-modulated radiotherapy and is symptom- free with good fusion at the latest follow- up (14 months) (Fig. 7, 8). Sensory disturbances recovered completely. (Table 2) shows neurological examination finding at latest follow-up.
Extensive physiotherapy and passive range of movements of lower limbs were started immediately in the post-operative period. An ankle-foot orthosis was given to prevent equinus deformity at the ankle. The patient was subjected to 23 cycles of intensity-modulated radiotherapy and is symptom- free with good fusion at the latest follow- up (14 months) (Fig. 7, 8). Sensory disturbances recovered completely. (Table 2) shows neurological examination finding at latest follow-up.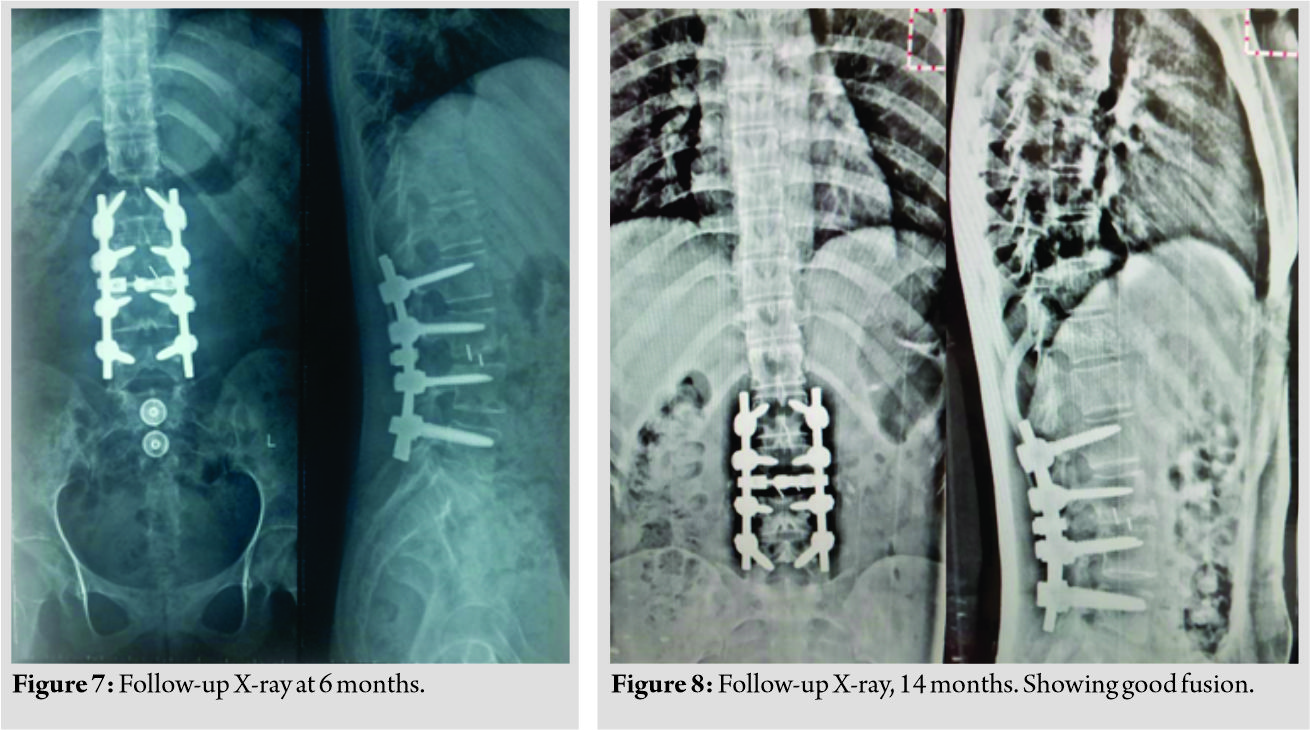
Discussion
SBP is a rare type of plasma cell dyscrasia with a male:female ratio of 2:1. Malignant bone tumors of the spine are extremely rare with an incidence of 0.05% of primary neoplasms and solitary plasmacytoma of the vertebra accounts for about 30% of the total within this group [3]. The standard treatment protocol involves radiotherapy and chemotherapy with or without spinal stabilization surgeries. As the tumor cells are sensitive to radiation, it is a well-established treatment modality in any stage of the disease [4, 5, 6, 7]. If a patient presents with spinal instability and neurological deficit, surgical management is the modality of choice followed by radiotherapy and/or chemotherapy [8]. The patient in this report presented with severe instability pain, kyphotic deformity of lower back, and neurological deficit. She was managed with posterior decompression and instrumented spine stabilization with 360° fusion (TLIF +PLF) and iliac crest graft followed by 23 cycles of intensity-modulated radiation therapy (total of 46 Gy). Ozsahin et al., in a retrospective study, studied 5-year survival rate, disease-free survival, and local recurrence rate in patients with SPB (206 patients) and extramedullary plasmacytoma (52 patients) who were treated alone with radiotherapy (214 patients), radiotherapy combined with chemotherapy (34 patients), and with surgery alone (8 patients). The 5-year overall survival, disease-free survival, and local control rate were 74%, 50%, and 86%, respectively [9]. The local recurrence rate following 40–50 Gy radiotherapy and those without radiotherapy was 12% and 60%, respectively [10]. This showed that radiotherapy promised a favorable and disease-free survival with minimal local recurrence. Tsang et al. studied local recurrence with respect to the diameter of SBP tumor. Tumor with diameter <5 cm showed 0% local recurrence and the tumor of diameter >5 cm showed 62% local recurrence [11, 12]. The recommended treatment for SPB is localized radiotherapy with a dose of 40–50 Gy over 4 weeks [3]. Radiotherapy is the first modality of treatment in SPB but many may present in the later stages of the disease with the neurological deficit for the 1st time to spine clinic. In these situations, surgery becomes the primary modality of treatment before radiotherapy which should be aimed at decompressing the neural tissues and to stabilize the spine. Modern methods such as vertebroplasty and kyphoplasty allow a surgical solution for patients who develop vertebral fractures, kyphotic deformity, neurological complications, or a combination of these. Radiotherapy can be delayed until after surgery but it is still required because tumor excision without subsequent radiotherapy results in a very high rate of local recurrence [7]. The role of chemotherapy as adjuvant therapy in SPB is controversial. A study by Holland et al. with 32 SPB patients showed that the incidence of progression of SPB to multiple myeloma is not affected by chemotherapy, but it delays the progression of SBP to multiple myeloma from 29 to 59 months [13]. Aviles also showed improved outcomes in a small randomized prospective clinical trial on SBP when patients received adjuvant melphalan and prednisolone for 3 years [14]. Baba et al. [15] reported eight patients with a solitary plasmacytoma of the spine associated with neurological complications. The tumor was confined to the thoracic spine in six cases, cervical spine in one, and lumbar spine in one. Treatment consisted of a combination of radiotherapy, melphalan, and surgery. Surgical decompression (anterior surgery in three cases and posterior surgery in five) produced neurological improvement in all patients. The study group concluded the importance of early diagnosis followed by appropriate treatment including surgery for this clinical entity and long-term follow-up for early detection of disseminated disease. Dafang Zhang D et al. [16] reported a similar case of solitary plasmacytoma involving L3 vertebral body and pedicles with mild vertebral collapse which was treated with minimally invasive posterior stabilization from L2-L4 without fusion and definitive localized radiation therapy. Patient’s symptoms improved in terms of pain. There was no recurrence or hardware failure and was experiencing an excellent quality of life. Venkatesh et al. [17] reported a case of solitary plasmacytoma of L3 vertebral body in 72 years old with progressive neurological deficit. The minimally invasive approach was used, anterior column reconstruction in the lumbar spine using an expandable cage was done, and no local recurrence of tumor or deterioration of neurological deficit was observed. The patients of plasmacytoma, especially involving the lumbar vertebrae, have local symptoms such as back pain and deformity in the initial phases. The neurological involvement and deformity occur late in the disease process when the local symptoms are either ignored/not diagnosed or improperly treated as demonstrated in our case report. The patient’s surgical stabilization can be achieved by minimally invasive methods and tumor addressed by radiotherapy if the condition is diagnosed in the early phase of disease as demonstrated by a few case reports [16]. Even when these patients present late with grotesque deformity, frank neurological involvement, they should be treated appropriately by surgery to stabilize the spine, correct the deformity, and in collaboration with oncology department for the definitive radiation therapy. The outcomes are usually good in these patients of single-level involvement when treated appropriately with significant improvement in pain, neurology, and deformity as shown in our case. The patient showed clinical, radiological, and neurological improvement (ambulatory without any assistance) at follow-up of 14 months.
Conclusion
Solitary plasmacytoma of vertebra with neurological deficit and instability should be treated with spinal stabilization surgery followed by radiotherapy to achieve predictable outcomes in terms of neurological improvement and activities of daily living.
Clinical Message
In a suspected case of solitary plasmacytoma of the spine, thorough investigations and prompt treatment should be undertaken to avoid the progress of the tumor which may lead to further deformity and neurological deterioration. Our case is unique due to its delayed presentation with deformity and neurological deficit which recovered to near normal status after treatment.
References
1. Dingli D, Kapoor P. Solitary plasmacytoma. In: Multiple Myeloma: Diagnosis and Treatment. New York: Springer; 2014. p. 195-210.
2. Mendoza S, Urrutia J, Fuentes D. Surgical treatment of solitary plasmocytoma of the spine: Case series. Iowa Orthop J 2004;24:86-94.
3. Soutar R, Lucraft H, Jackson G, Reece A, Bird J, Low E, et al. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Br J Haematol 2004;124:717-26.
4. Elman R. The part-time faculty member in medical education and research; clinical investigation. J Med Educ 1953;28:19-23.
5. Galieni P, Cavo M, Pulsoni A, Avvisati G, Bigazzi C, Neri S, et al. Clinical outcome of extramedullary plasmacytoma. Haematologica 2000;85:47-51.
6. Kilciksiz S, Celik OK, Pak Y, Demiral AN, Pehlivan M, Orhan O, et al. Clinical and prognostic features of plasmacytomas: A multicenter study of Turkish oncology group-sarcoma working party. Am J Hematol 2008;83:702-7.
7. Knobel D, Zouhair A, Tsang RW, Poortmans P, Belkacémi Y, Bolla M, et al. Prognostic factors in solitary plasmacytoma of the bone: A multicenter rare cancer network study. BMC Cancer 2006;6:1-9.
8. Kilciksiz S, Karakoyun-Celik O, Agaoglu FY, Haydaroglu A. A review for solitary plasmacytoma of bone and extramedullary plasmacytoma. Sci World J 2012;2012:895765.
9. Ozsahin M, Tsang RW, Poortmans P, Belkacémi Y, Bolla M, Öner Dinçbas F, et al. Outcomes and patterns of failure in solitary plasmacytoma: A multicenter rare cancer network study of 258 patients. Int J Radiat Oncol Biol Phys 2006;64:210-7.
10. Dunn AM, Hofmann OS, Waters B, Witchel E. Cloaking Malware with the Trusted Platform Module. San Francisco, CA: Proceedings of the 20th USENIX Security Symposium; 2011. p. 395-410.
11. Warsame R, Gertz MA, Lacy MQ, Kyle RA, Buadi F, Dingli D, et al. Trends and outcomes of modern staging of solitary plasmacytoma of bone. Am J Hematol 2012;87:647-51.
12. Reed V, Shah J, Medeiros LJ, Ha CS, Mazloom A, Weber DM, et al. Solitary plasmacytomas: Outcome and prognostic factors after definitive radiation therapy Cancer 2011;117:4468-74.
13. Holland J, Trenkner DA, Wasserman TH. Plasmacytoma. Treatment results and conversion to myeloma. Cancer 1992;69:1513-7.
14. Aviles A. Improved outcome in solitary bone plasmacytomata with combined therapy. Hematol Oncol 1996;14:111-7.
15. Baba H, Maezawa Y, Furusawa N, Wada M, Kokubo Y, Imura S. Solitary plasmacytoma of the spine associated with neurological complications. Spinal Cord 1998;36:470-5.
16. Zhang D, Hess K, Nielsen GP, Schwab JH. Minimally invasive posterior stabilization of a solitary plasmacytoma of the lumber spine with long-term follow-up: A case report. Orthop J Harv Med Sch 2016;17:79-83.
17. Venkatesh R, Tandon V, Patel N, Chhabra HS. Solitary plasmacytoma of L3 vertebral body treated by minimal access surgery: Common problem different solution! J Clin Orthop Trauma 2015;6:259-64.
 |
 |
 |
 |
 |
 |
| Dr. Nagaraj Manju Moger | Dr. Syed Ifthekar | Dr. Kaustubh Ahuja | Dr. Samarth Mittal | Dr. J Pragadeeshwaran | Dr. Pankaj Kandwal |
| How to Cite This Article: Moger NM, Ifthekar S, Ahuja K, Mittal S, Pragadeeshwaran J, Kandwal P. Single-stage 360° Reconstruction in a Case of Solitary Vertebral Plasmacytoma of L3 vertebra – A Case Report. Journal of Orthopaedic Case Reports 2020 September;10(6): 23-27. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com