[box type=”bio”] Learning Point of the Article: [/box]
One should suspect hyperparathyroidism in cases of multiple osteolytic lesions and get serum PTH and USG neck done for diagnosing it.
Case Report | Volume 10 | Issue 6 | JOCR September 2020 | Page 49-53 | Nareshkumar Satyanarayan Dhaniwala, Mukund Naresh Dhaniwala. DOI: 10.13107/jocr.2020.v10.i06.1872
Authors: Nareshkumar Satyanarayan Dhaniwala[1], Mukund Naresh Dhaniwala[2]
[1]Department of Orthopedics, Jawaharlal Nehru Medical College and Acharya Vinoba Bhave Rural Hospital, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India.
[2]Department of Orthopedics, Mahatma Gandhi Institute of Medical Sciences, Wardha, Maharashtra, India.
Address of Correspondence:
Dr. Nareshkumar Satyanarayan Dhaniwala,
Department of Orthopedics, Jawaharlal Nehru Medical College and Acharya Vinoba Bhave Rural Hospital, Datta Meghe Institute of Medical Sciences, Sawangi (Meghe), Wardha – 442 107, Maharashtra. India.
E-mail: nsdhaniwala@gmail.com
Abstract
Introduction: Pathological fractures in long bones are commonly caused by simple bone cyst or Osteogenesis imperfecta in children and by metastatic tumors from primary carcinoma, multiple myeloma, osteoporosis, and bone tumors in adults. Hyperparathyroidism causing pathological fractures, though a well-known entity, is seen infrequently in clinical practice. The fractures occur in the expansile fibro-cystic bone lesions called as “Brown tumor.” The reported case describes a patient with classical features of primary hyperparathyroidism (PHPT) having multiple lytic lesions in pelvis and bilateral femur with pathological fracture. It is being reported due to its rarity.
Case Report: A 28–year-old young married lady presented with chronic dull aching pain in both thighs and difficulty in walking for 2 years. Examination revealed tenderness in both thighs, with antalgic gait. X-ray pelvis with both thighs showed multiple lytic lesions of variable size in both femora and pelvis. Blood investigations showed raised levels of serum calcium, with highly raised levels of serum parathyroid hormone (PTH). Contrast-enhanced computerized tomography (CT) scan of neck demonstrated parathyroid adenoma. The patient admitted for prophylactic nailing for right femur, developed a fracture while indoor and was managed by right proximal femoral nailing, followed by parathyroid adenoma excision. Follow-up showed dramatic clinical and radiological improvement with good healing of fracture. Lytic lesions healed gradually and blood parameters returned to normal. The patient remains asymptomatic at 2 years follow-up.
Conclusion: Advanced case of symptomatic PHPT affecting bones is rare and it should be considered as a differential diagnosis in cases of a solitary and or multiple osteolytic lesions. Serum calcium and PTH level estimation at an early stage prevents missing the diagnosis and progression of disease. Early diagnosis and appropriate treatment help in rapid clinical improvement with almost total reversal of bony changes, thus avoiding devastating complications.
Keywords: Hyperparathyroidism, brown tumor, osteitis fibrosa cystica, femur, pathological fracture.
Introduction
Primary hyperparathyroidism (PHPT), also known as Osteitis fibrosa cystica, Von Recklinghausen’s disease or Para-thyrotoxicosis results in excessive secretion of parathyroid hormone (PTH). This leads to marked increase in osteoclasts, rapid resorption of the bone, and fibrous replacement of marrow. PTH mobilizes calcium from bone and causes phosphorous diuresis, both actions depleting the mineral reservoirs of bone. Alkaline phosphatase (ALP) is increased indicating compensatory bone formation. “Brown tumors” are localized accumulation of hemorrhage, blood pigments, and reactive mass of osteoclasts in a spindle cell stroma. It is a well circumscribed dark brown area of soft consistency in the area of gross bony resorption. Solitary parathyroid adenoma is the most common cause of PHPT, representing 80% of cases [1]. The condition often occurs in middle aged women, remaining asymptomatic in half of the patients, and symptoms being mild for a long duration in others. Pain in back and lower limbs, generalized muscle weakness, pathologic fractures in long bones, vague abdominal complaints, polyuria, and polydipsia may be seen along with neuro-psychiatric symptoms. If it is not diagnosed and left untreated, devastating consequences such as osteoporosis, pathological fractures, nephrolithiasis, and renal failure may occur. Hyperparathyroidism is always considered as a differential diagnosis of generalized osteoporosis. Clinical suspicion of PHPT can be confirmed by abnormally raised serum PTH value, along with evidence of parathyroid growth on ultrasonography (USG) or CT scan of neck. Cure is by parathyroidectomy. After surgery, osteoblastic activity increases replacing brown tumor by normal lamellar bone. Orthopedic management involves prophylactic or therapeutic fixation of fractures and regular follow-up to assess regain of bone density. Avoidance of hypo-calcemic crisis by suitable calcium supplementation is another important point to take note of after parathyroidectomy.
Case Report
A 28-year-old married housewife presented in the orthopedics outpatient department of tertiary care hospital in Central India with the chief complaints of pain in both thighs, more on the right side and difficulty in walking for the past 2 years. Pain had started spontaneously, was insidious in onset, and localized initially to both thighs. It increased with weight bearing, walking and household chores and partially got relieved on rest and medication. There was pain in elbow, wrist, and both hands for a few months initially. There was no history of fever, loss of appetite, loss of weight, or any change in menstrual cycle. Her joints’ pain and left thigh pain got completely relieved with drugs, but pain in the right thigh and hip area did not improve. She noticed progressively increasing difficulty in walking, squatting, and sitting cross-legged during the past 6 months. She started feeling rest pain in the right thigh and started taking stick support for the past 2 months. She had undergone repeated consultations, investigations, and treatment, but was not relieved of her symptoms. Examination revealed painful gait with minimal weight bearing on the right lower limb. The patient was thin built with mild pallor and without any systemic abnormality. Her pulse was 84/minute and blood pressure 130/70 mmHg. Tenderness was present on upper one-third of right thigh and both pubic rami with adductor muscle spasm. Right hip rotations and abduction adduction were grossly restricted with flexion possible up to 70°. Left hip movements were normal except terminal restriction of flexion. There was no neurovascular deficit. Examination of other bones and spine did not reveal any abnormality.
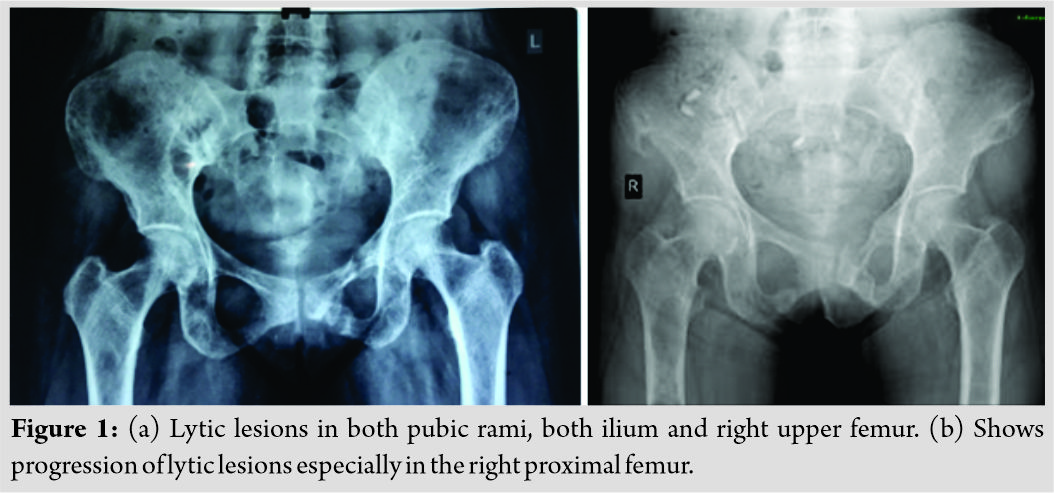
A clinical diagnosis of Osteomalacia with Looser’s zone in pubic rami and incomplete fracture in right femur was considered. Metastatic lesions, multiple myeloma, or hyperparathyroidism with brown tumors were considered as differential diagnoses. The patient underwent X-rays of relevant areas. X-ray of pelvis with both hips (Fig. 1a and b) showed multiple small osteolytic lesions in both ilium and femur, thinning of cortices and uniting fractures in bilateral pubic rami. X-rays of both thighs (Fig. 2a and b) showed generalized osteoporosis, multiple lytic areas of 2–3 cm size separated with each other by a small zone of normal bone in upper one-third of shaft.
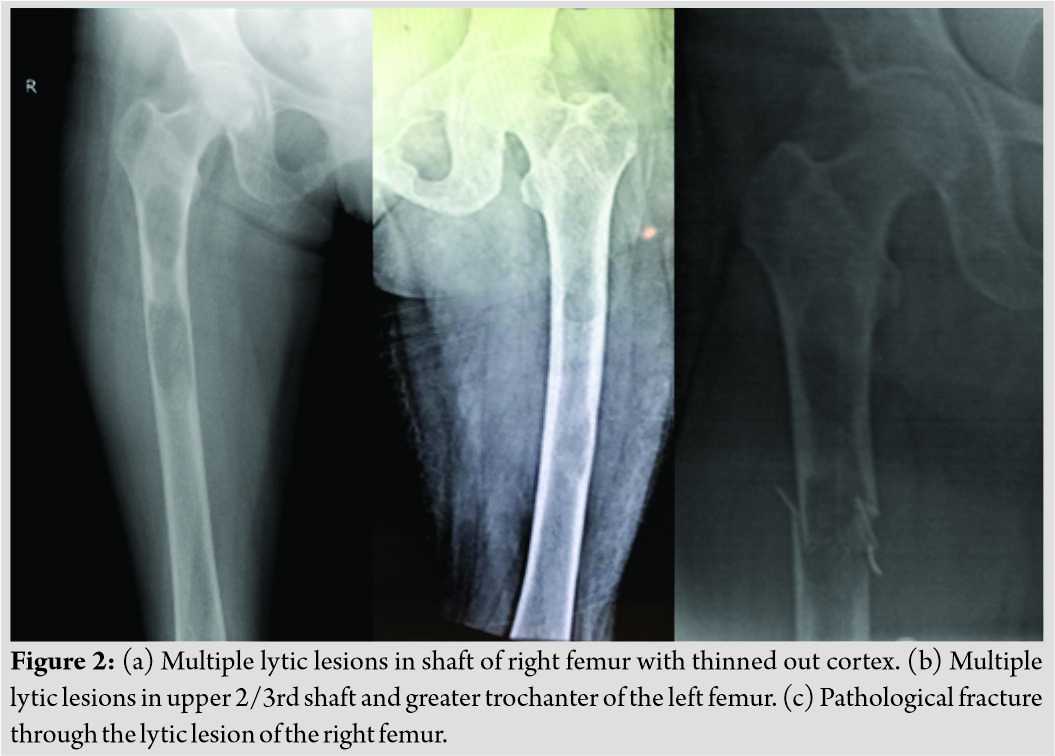
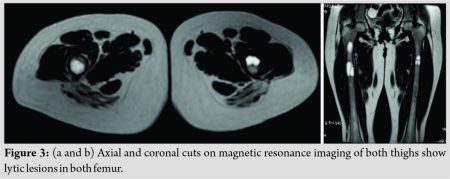
There were two large osteolytic areas in the right shaft femur. The patient was admitted for prophylactic nailing in right femur in view of the impending fracture through the lytic areas (Fig. 2a). She was given an above knee up to groin plaster slab and advised bed rest. In the left femur, the osteolytic areas were relatively smaller, cortices were thicker and there was no immediate risk of an impending fracture. Hence, fixation of left femur was not considered. X-rays of skull, chest, lumbar spine, feet, and hands did not show any obvious abnormality. Old magnetic resonance imaging (MRI) of thighs suspected the small lytic lesions in both femora as simple bone cyst. Fresh MRI with contrast (Fig. 3a and b) showed multiple intramedullary solid cystic lesions of varied size in both pubic rami, ischium, iliac blades, and upper and middle one-third of both femora probably due to browns tumor.
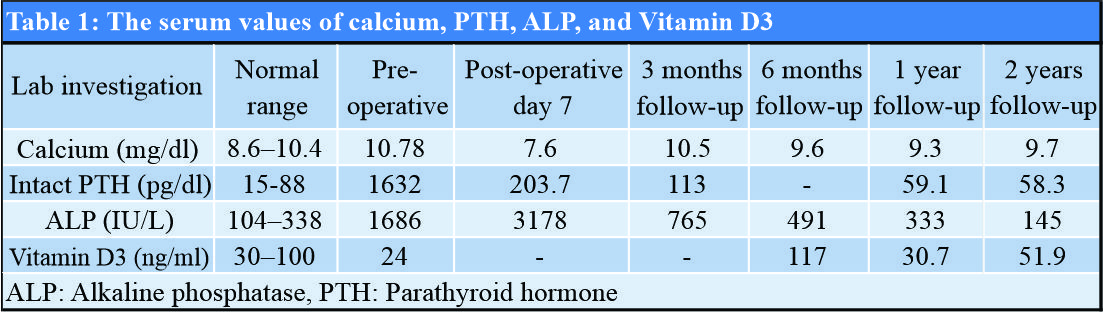
USG of neck suggested the possibility of parathyroid adenoma of size 37 mm × 19 mm. Contrast-enhanced CT scan of neck showed well defined heterogeneously enhancing nodular mass lesion of size 33 mm × 24 mm × 23 mm just posterior to the right lobe of thyroid, suggestive of parathyroid adenoma with lytic lesions in the base of skull and in the right occipital bone. USG-guided fine-needle aspiration cytology from lytic lesion over right iliac crest showed only hemorrhagic background without any cellularity. Patient’s complete blood count, erythrocyte sedimentation rate, C-reactive protein, rheumatoid factor, and urine examination were normal. She had hypercalcemia and hyperparathyroidism with serum calcium level of 10.78 mg/dl, PTH 1632 pg/dl, ALP 1686 IU/L, and Vitamin D3 24 ng/ml. Serum calcium, PTH, ALP, and Vitamin D3 levels done on various occasions are summarized in [Table 1].
While indoor, the patient tried going to bathroom and fell down, leading to fracture through the lytic area in the right proximal femur (Fig. 2c). The fracture was surgically stabilized with long proximal femur nail and static locking (Fig. 4a).
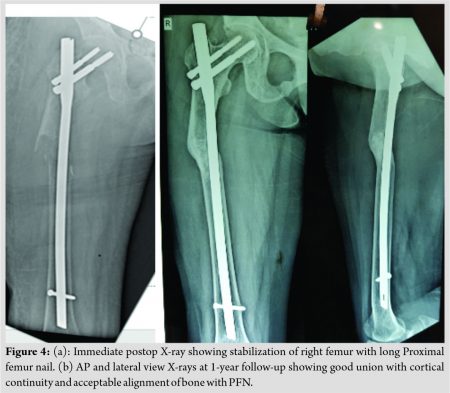
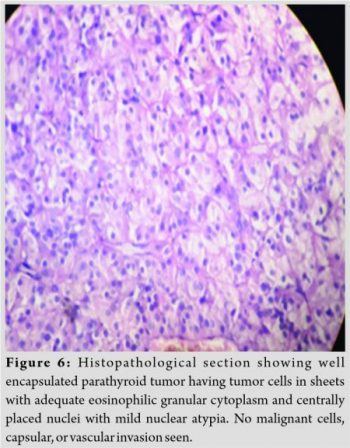
Open biopsy from lytic lesion was done after stabilization of fracture. The biopsy showed fibro-collagenous tissue having sheets of cells with adequate amount of eosinophilic granular cytoplasm and centrally placed nucleus without any malignant features. Per-operatively, the lytic area was very soft containing reddish brown friable tissue. Bony destruction was gross causing gap in cortical continuity at pathological fracture site despite nailing. Her post-operative period was uneventful. She was transferred to surgical unit for right parathyroid adenoma excision which was done successfully. The excised adenoma was of size 2.5 cm × 2.5 cm × 1 cm. Its histology showed typical features of adenoma without any features of malignancy and vascular or capsular invasion (Fig. 6). Immediately after adenoma excision she was kept on supportive intravenous calcium supplementation to avoid hypo-calcemic crisis (Hungry bone syndrome). The post-operative protocol followed was: Static quadriceps and hamstring exercises with active hip, knee, and ankle mobilization in bed for 2 weeks. After this, bedside knee mobilization and non-weight bearing mobilization with walker was started gradually. Patient was kept non-weight bearing for 12 weeks, followed by partial weight bearing with walker. Oral calcium and Vitamin D supplementation were continued. A 3 monthly follow-up was continued for clinical, radiological and serum calcium, and PTH estimation. She became asymptomatic at 6 months with near normal serum parameters and was permitted to walk with stick support. At 1 year (Fig. 4b), her fracture had consolidated satisfactorily; lytic lesions had almost disappeared and the patient was having full range of hip movement with normal weight bearing without support.

The X-ray of left femur at 1 year is shown in (Fig. 5). Serum calcium and PTH values had returned to normal. She conceived 1 year after the surgery and delivered a full-term normal baby. At 2 years follow-up, there is no pain in any bone, the right lower limb is shorter by 0.5 cm and her gait is normal. Patient is able to squat but has difficulty in sitting cross legged due to moderate restriction of external rotation in right hip. Nail removal is planned in a few months. The serum calcium, PTH, ALP, and Vitamin D levels are normal and majority of the brown tumors had regressed. The patient is asymptomatic and leading a normal life.
Discussion
“Brown tumor” is a characteristic focal osteolytic lesion seen in PHPT. It is filled with large number of osteoclasts, macrophages, and fibroblasts. The brown appearance is due to its high vascularity with concomitant hemorrhage and hemosiderin deposition. It may be solid, cystic, or a combination of both based on MRI [2]. The incidence of brown tumor in PHPT due to adenoma and hyperplasia is 3% [3, 4]. It may be single or multiple and may be located at any site. PHPT occurs due to one of the four parathyroid glands secreting excessive PTH which causes increase in both serum calcium and phosphorus due to rapid resorption of bones. Phosphorus diuresis decreases its serum levels. PHPT mostly occurs due to adenoma or rarely carcinoma. Secondary hyperparathyroidism occurs due to kidney disease while tertiary hyperparathyroidism develops in cases of long-term secondary hyperparathyroidism wherein the parathyroid glands overgrow and become permanently over active. Most patients of PHPT are clinically asymptomatic but some non-specific symptoms due to raised calcium levels are observed such as fatigue, malaise, joint pains, mild depression, and difficulty in concentration [5]. The signs and symptoms of PHPT are summarized in a rhyme as “stones, bones, abdominal groans, and psychiatric overtones” [6]. The stones in this phrase refer to renal stones; the abdominal groans refer to indigestion, nausea, vomiting, and peptic ulcers. The psychiatric overtones refer to depression, lethargy, and loss of memory. The bones refer to multiple small bone cysts, Osteomalacia and rarely, and brown tumor of long bones [7]. Other osseous manifestations may include subperiosteal and subchondral bone resorption around joints such as acromioclavicular, sternoclavicular, pubic symphysis and sacroiliac joints, salt and pepper appearance of skull, osteopenia, and frank osteoporosis [8]. Mishra et al. found that PHPT in Indians tends to be a severe, symptomatic disorder with skeletal, muscular, and renal manifestations at a younger age as compared to developed countries [9]. Vitamin D deficiency found in our population is a common comorbidity in Indians which further increases the severity of the disease [10]. Garla et al. [11] have reported a similar case in a 50-year-old lady with a large osteolytic lesion in distal femur. French et al. [12] and Ebina et al. [13] have also reported similar cases. Because it is a rare entity, the clinical symptoms and radiological findings can easily be confused with metastatic tumors. This delays the diagnosis and treatment, leading to disease progression, and complications. In this case, the patient reported to our center 2 years after the beginning of symptoms. There was a delay in diagnosis due to the non-specific nature of symptoms, late radiological assessment, and lack of suspicion about PHPT. The initial small osteolytic lesion in the right femur was considered as benign simple bone cyst. The crucial estimation of serum calcium and PTH which could have diagnosed hyperparathyroidism early was done after presentation to us. By this time, there was severe disease progression and impending pathological fracture in femur. Mirels’ criteria (Table 2) help to decide for prophylactic fixation of long bones in case of a pathologic lesion.
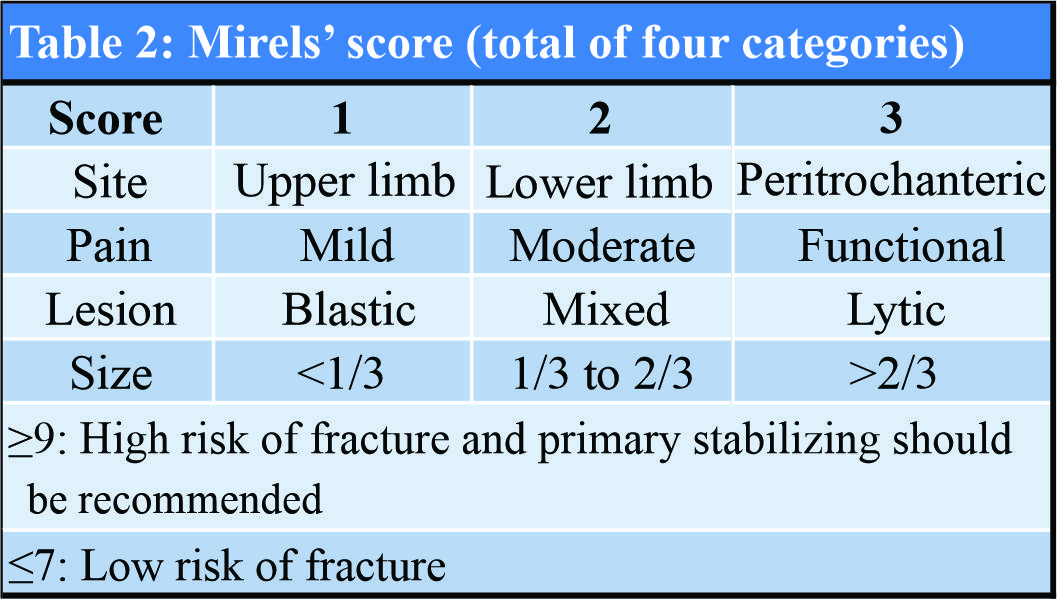
As per it, the patient’s Mirels’ score [14] was 12 for the right femur on admission which indicated a high risk for impending fracture. For left femur, it was eight without any pain and possibility of impending fracture. Hence, prophylactic fixation of left femur was not done. Suspicion of the condition prompted us to do USG and CT scan of neck, which clinched the rare diagnosis. CT scan is useful in defining the bony lesions better, besides it also helps in diagnosis of parathyroid adenoma in the neck. Surgical resection of parathyroid adenoma yielded good therapeutic results.
Conclusion
This case illustrates the importance of suspicion, early detection and diagnosis of PHPT by USG neck and biochemical markers for bone metabolism such as serum calcium and PTH. PHPT with brown tumors should be considered as a differential diagnosis when multiple osteolytic lesions are seen on plain X-rays of flat and long bones in adolescents and adults.
Parathyroidectomy with adequate calcium and Vitamin D supplementation helps the bony lesions to regress almost completely in due course of time. Few cases may require prophylactic internal fixation and Mirels’ score can help in this decision.
Clinical Message
Multiple lytic lesions in bones with none or mild symptoms of pain in an adult should be viewed with suspicion and detailed radiological and biochemical investigations including serum calcium and PTH should be done to rule out PHPT.
References
1. Jain AK, Jajodia N. Metabolic bone diseases and related dysfunction of the parathyroid glands. In: Jain AK, editor. Turek’s Orthopaedics. 7th ed. South Holland, Netherlands: Wolters Kluwer; 2017. p. 251-6.
2. Hong WS, Sung MS, Chun KA, Kim JY, Park SW, Lee KH, et al. Emphasis on the MR imaging findings of brown tumor: A report of five cases. Skeletal Radiol 2011;40:205-13.
3. Proimos E, Chimona TS, Tamiolakis D, Tzanakakis MG, Papadakis CE. Brown tumor of the maxillary sinus in a patient with primary hyperparathyroidism: A case report. J Med Case Rep 2009;3:7495.
4. Yilmazlar S, Arslan E, Aksoy K, Tolunay S. Sellar-parasellar brown tumor: Case report and review of literature. Skull Base 2004;14:163-8.
5. Eller-Vainicher C, Filopanti M, Palmieri S, Ulivieri FM, Morelli V, Zhukouskaya VV, et al. Bone quality, as measured by trabecular bone score, in patients with primary hyperparathyroidism. Eur J Endocrinol 2013;169:155-62.
6. Turner JJ. Hypercalcaemia and primary hyperparathyroidism. Medicine (Baltimore) 2017;45:551-4.
7. Misiorowski W, Czajka-Oraniec I, Kochman M, Zgliczyński W, Bilezikian JP. Osteitis fibrosa cystica a forgotten radiological feature of primary hyperparathyroidism. Endocrine 2017;58:380-5.
8. Osseous Manifestations of Primary Hyperparathyroidism: Imaging Findings. Available from: https://www.hindawi.com/journals/ije/2020/3146535. [Last accessed on 2020 May 16].
9. Mishra SK, Agarwal G, Kar DK, Gupta SK, Mithal A, Rastad J. Unique clinical characteristics of primary hyperparathyroidism in India. Br J Surg 2001;88:708-14.
10. Harinarayan CV, Gupta N, Kochupillai N. Vitamin D status in primary hyperparathyroidism in India. Clin Endocrinol (Oxf) 1995;43:351-8.
11. Garla VV, Akhtar I, Salim S, Subauste A. Osteitis fibrosa cystica masquerading as bone neoplasm. BMJ Case Rep 2018;2018:bcr2018224546.
12. French R, Oweis D, Kurup V. Bilateral femoral fractures in a 21-year-old man following a simple fall. BMJ Case Rep 2013;2013:bcr2013009753.
13. Ebina K, Miyoshi Y, Izumi S, Hashimoto J, Naka N, Tsukamoto Y, et al. A case of adolescent giant parathyroid adenoma presenting multiple osteolytic fractures and postoperative hungry bone syndrome. Clin Case Rep 2015;3:835-40.
14. Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res 1989;249:256-64.
 |
 |
| Dr. Nareshkumar Satyanarayan Dhaniwala | Dr. Mukund Naresh Dhaniwala |
| How to Cite This Article: Dhaniwala NS, Dhaniwala MN. Multiple brown tumors in a case of primary hyperparathyroidism with pathological fracture in femur. Journal of Orthopaedic Case Reports 2020 September;10(6): 49-53. |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com








